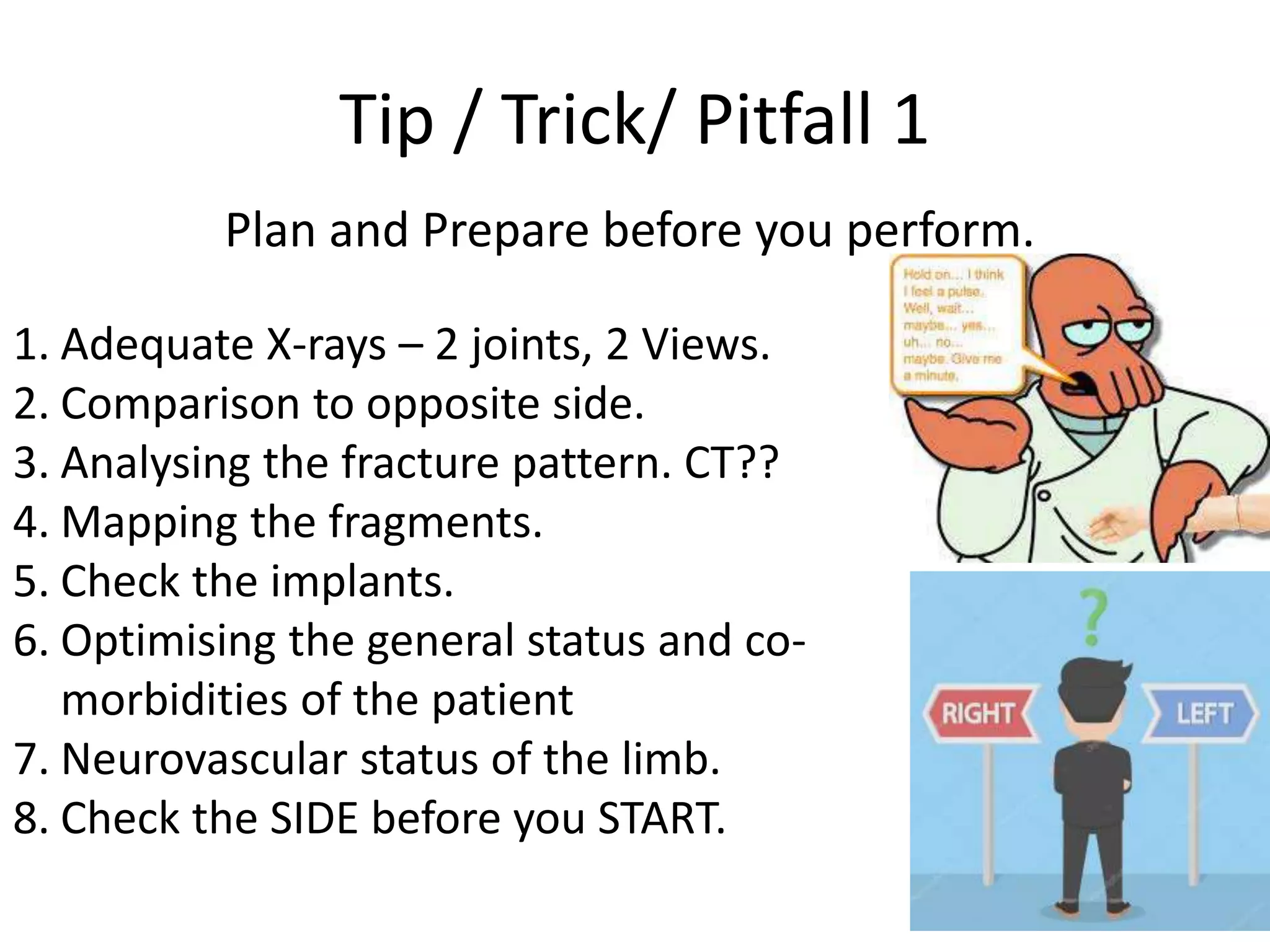
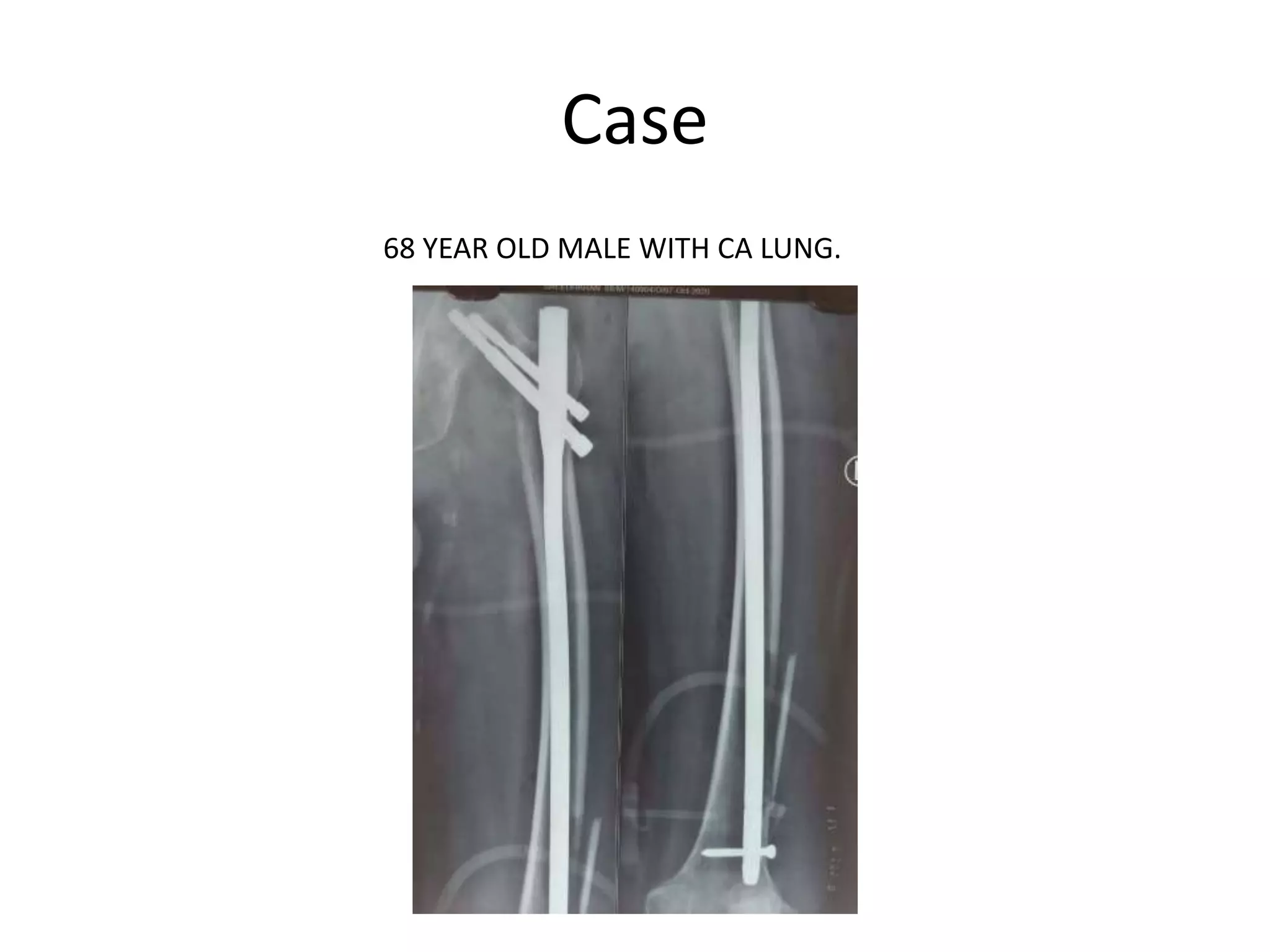
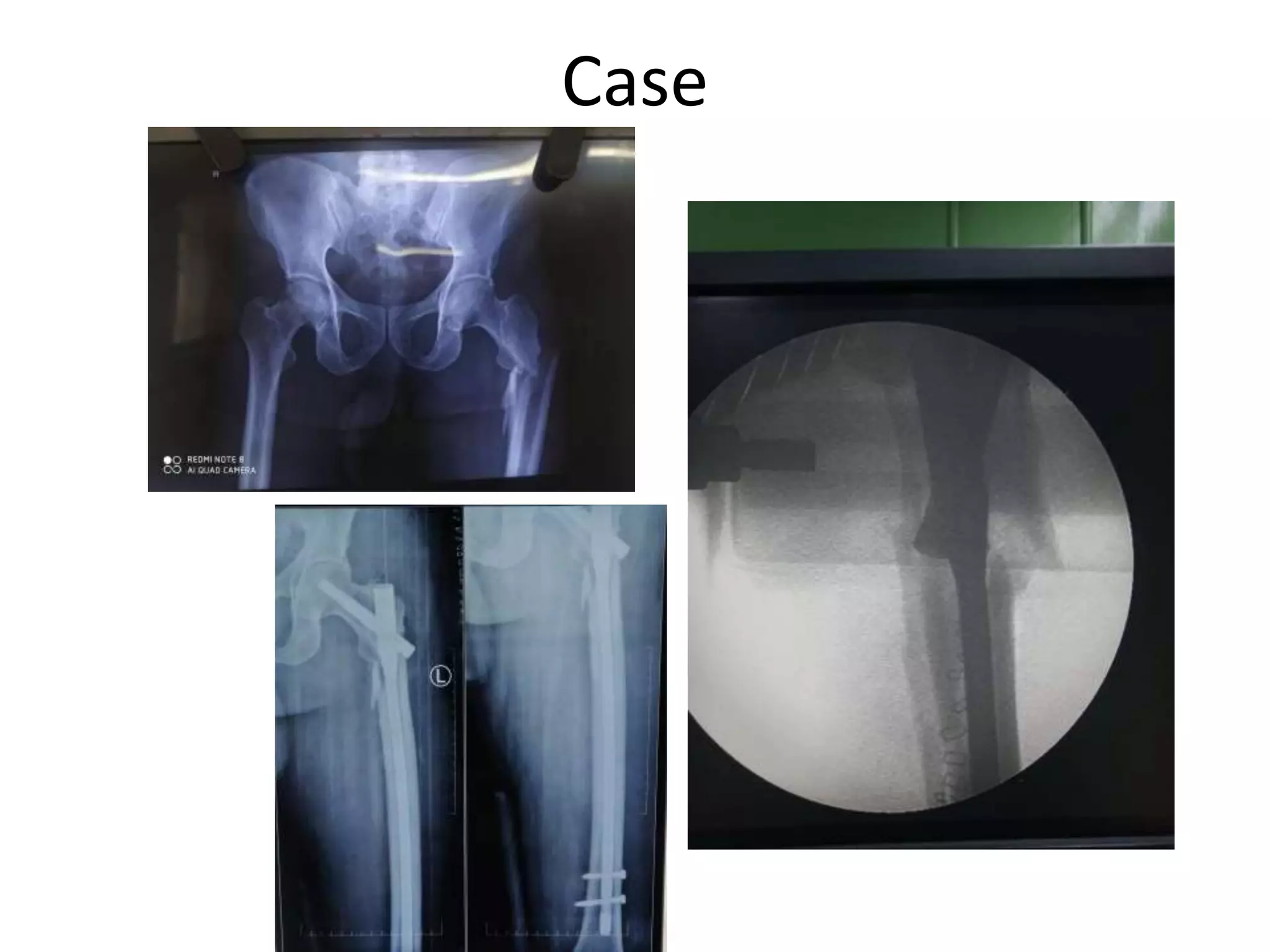
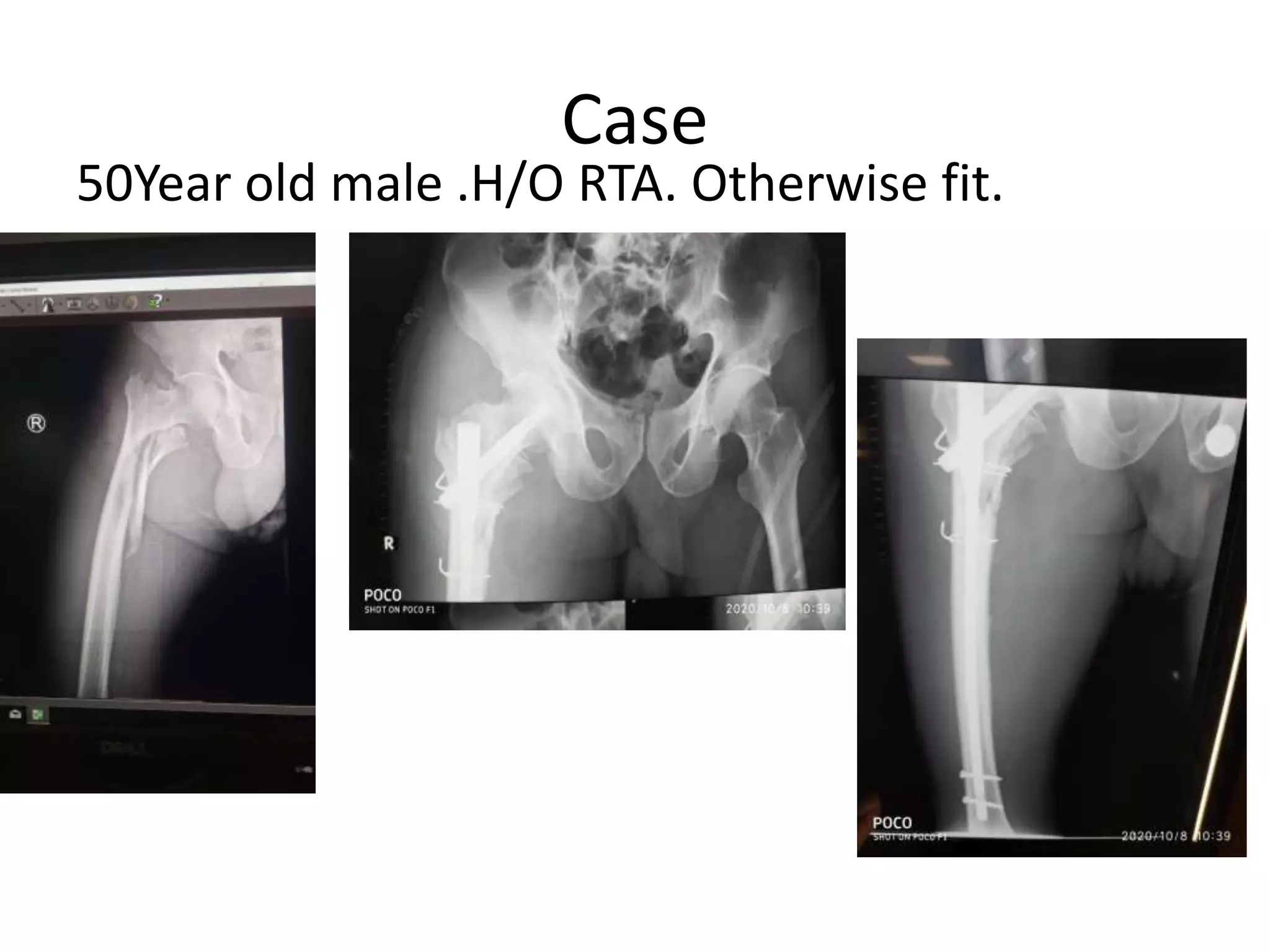
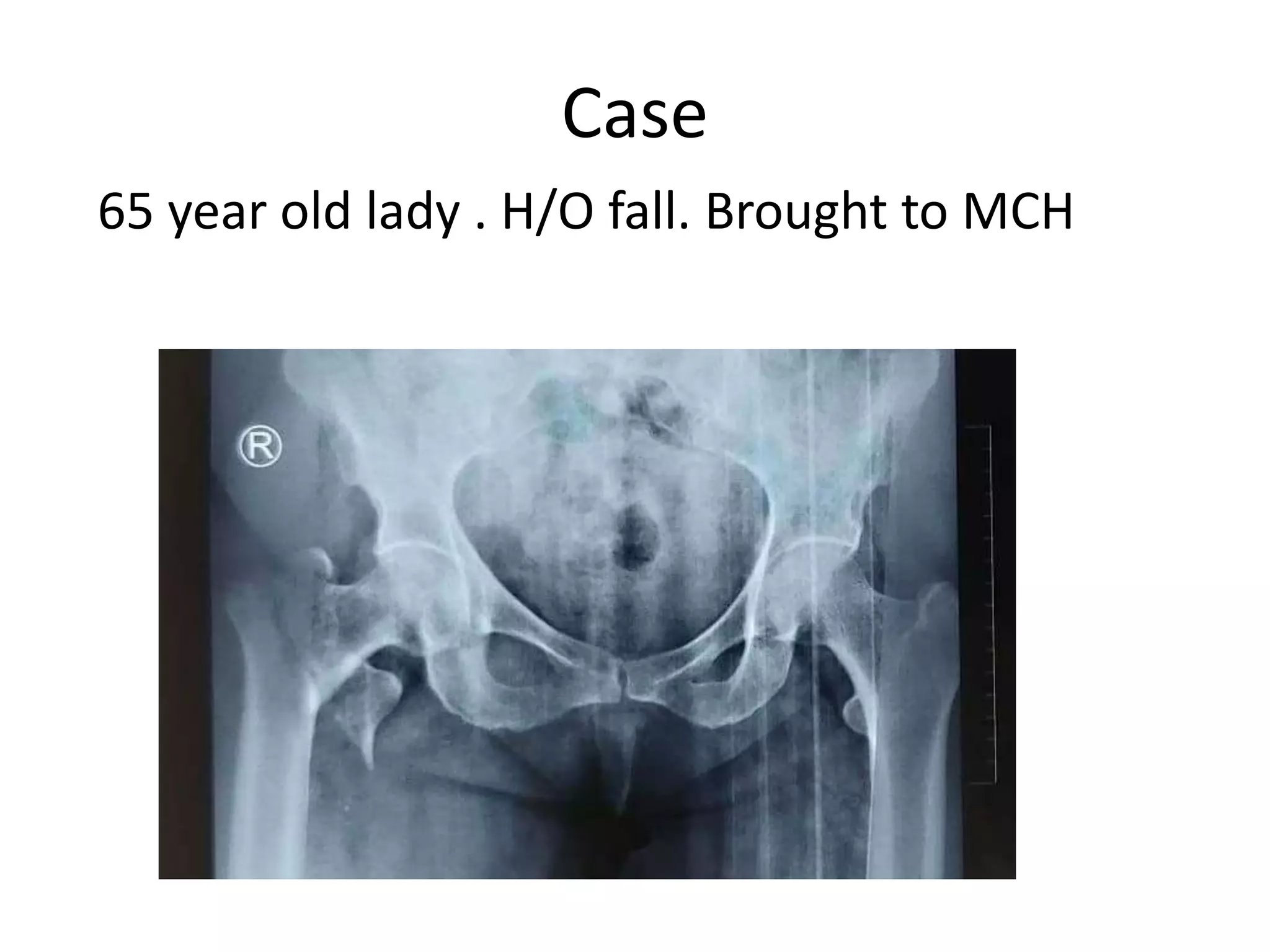
1. Proximal femoral nailing (PFN) requires thorough pre-operative planning including imaging and assessment of fracture pattern and patient comorbidities.
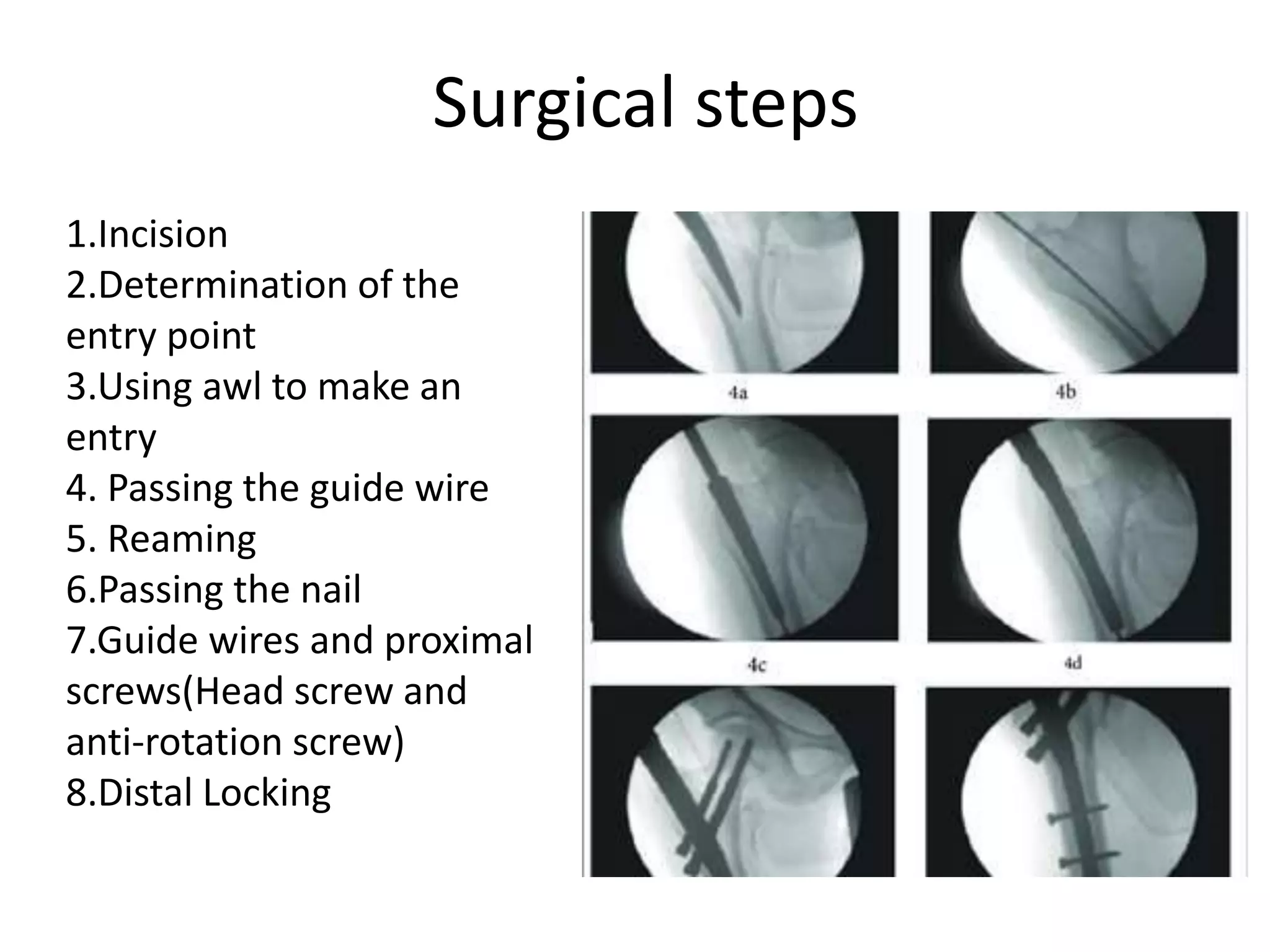
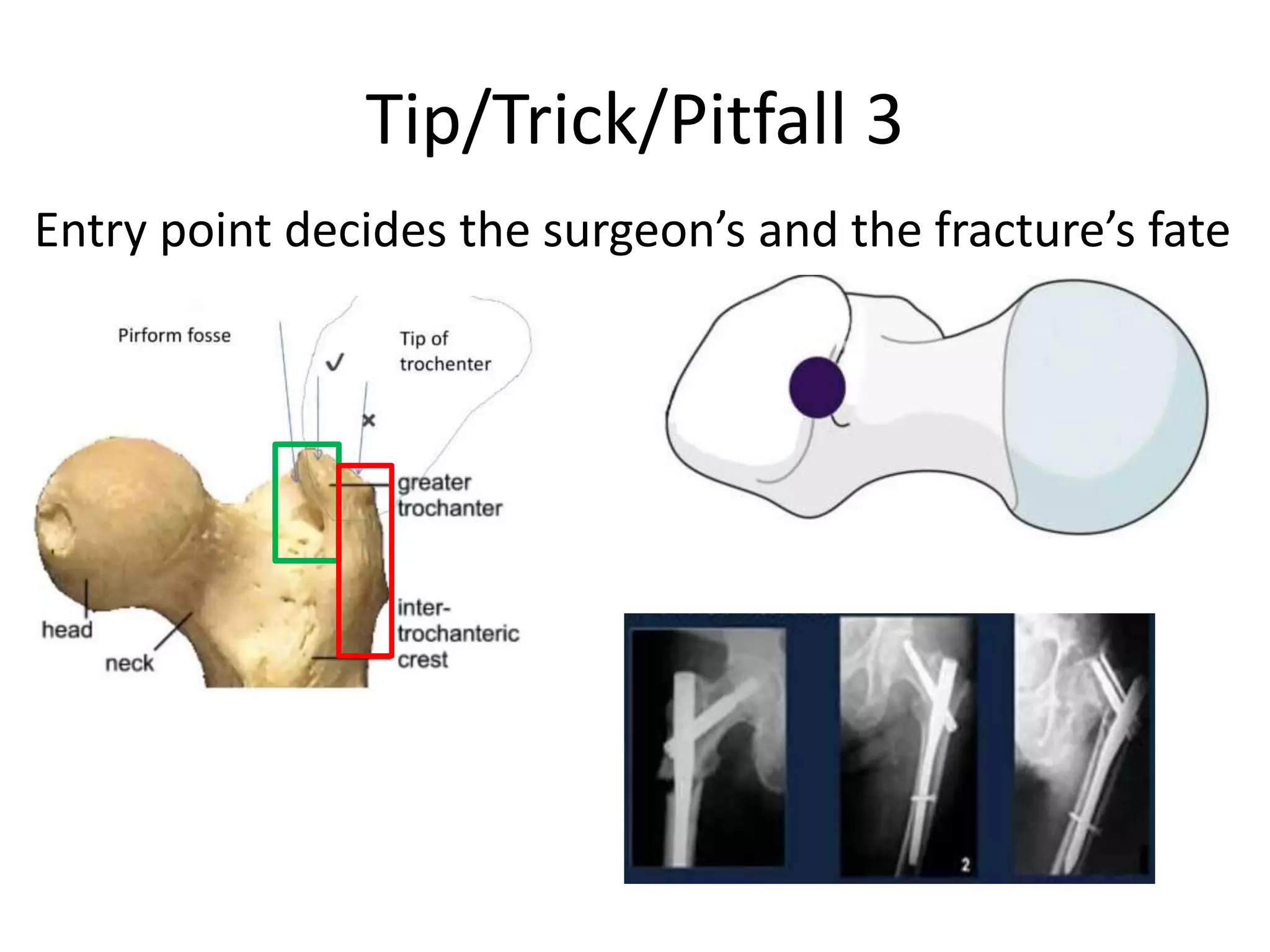
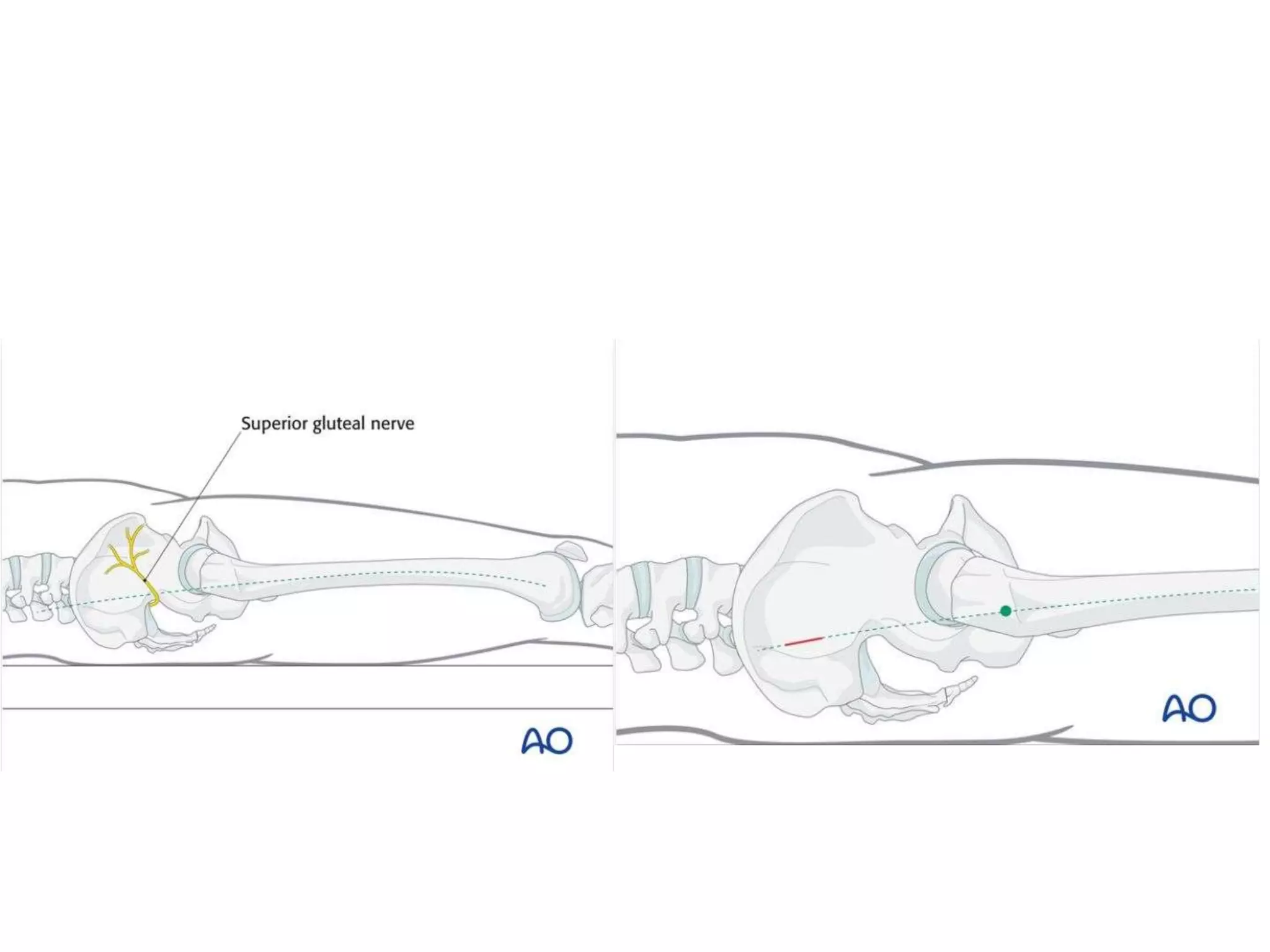
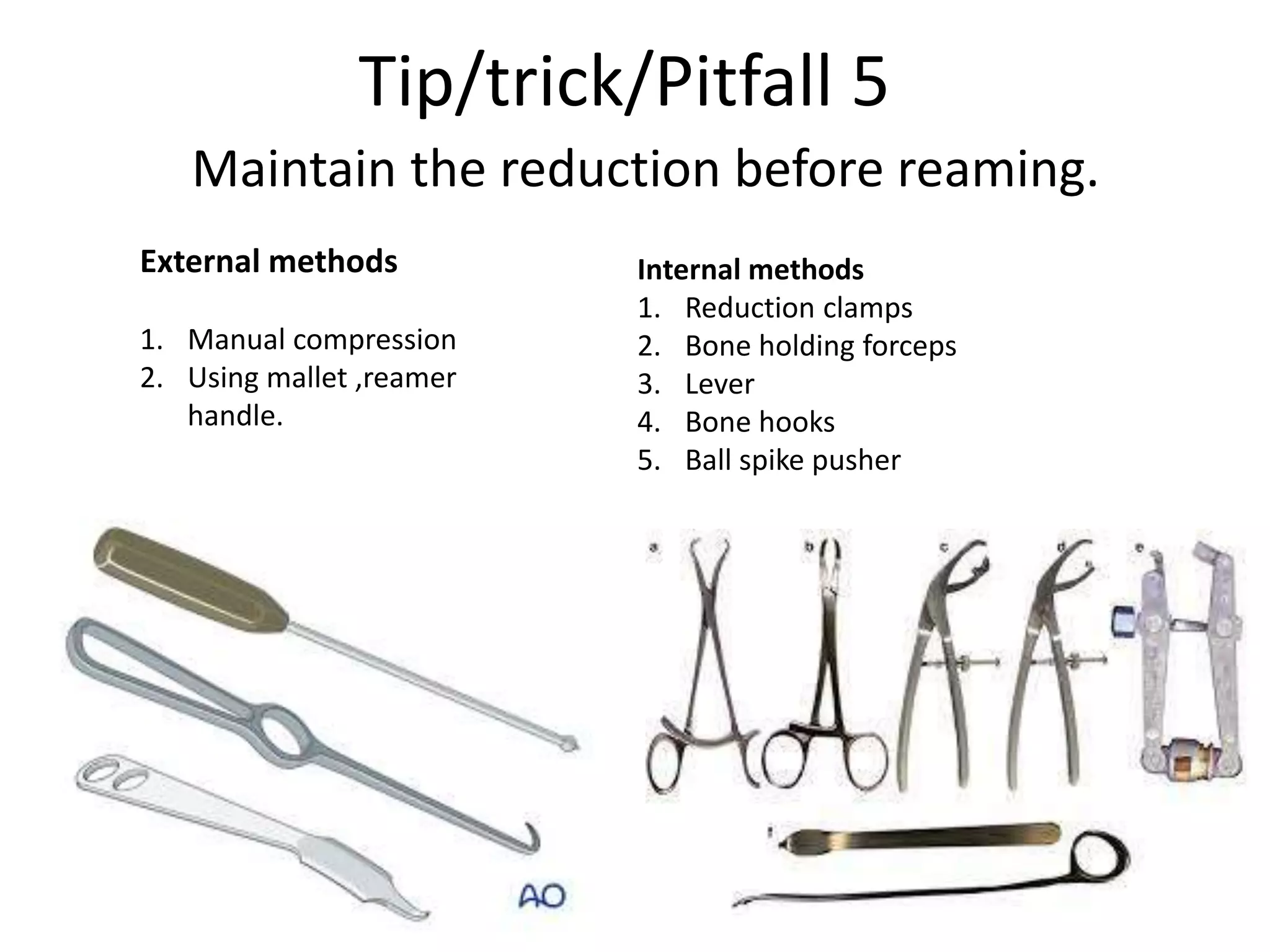
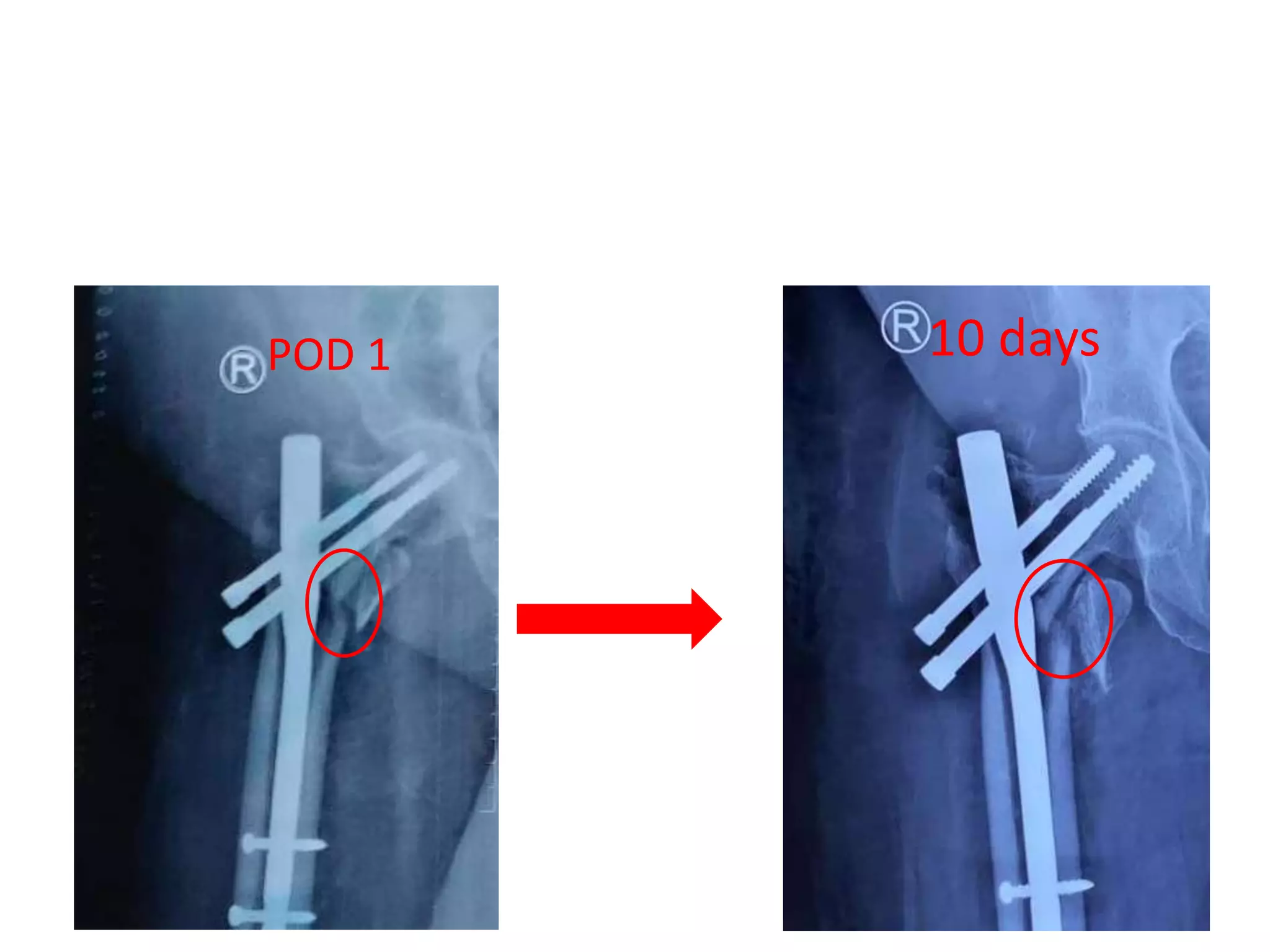
2. It is important to reduce the fracture before making the entry point, as the entry point will determine surgical success.
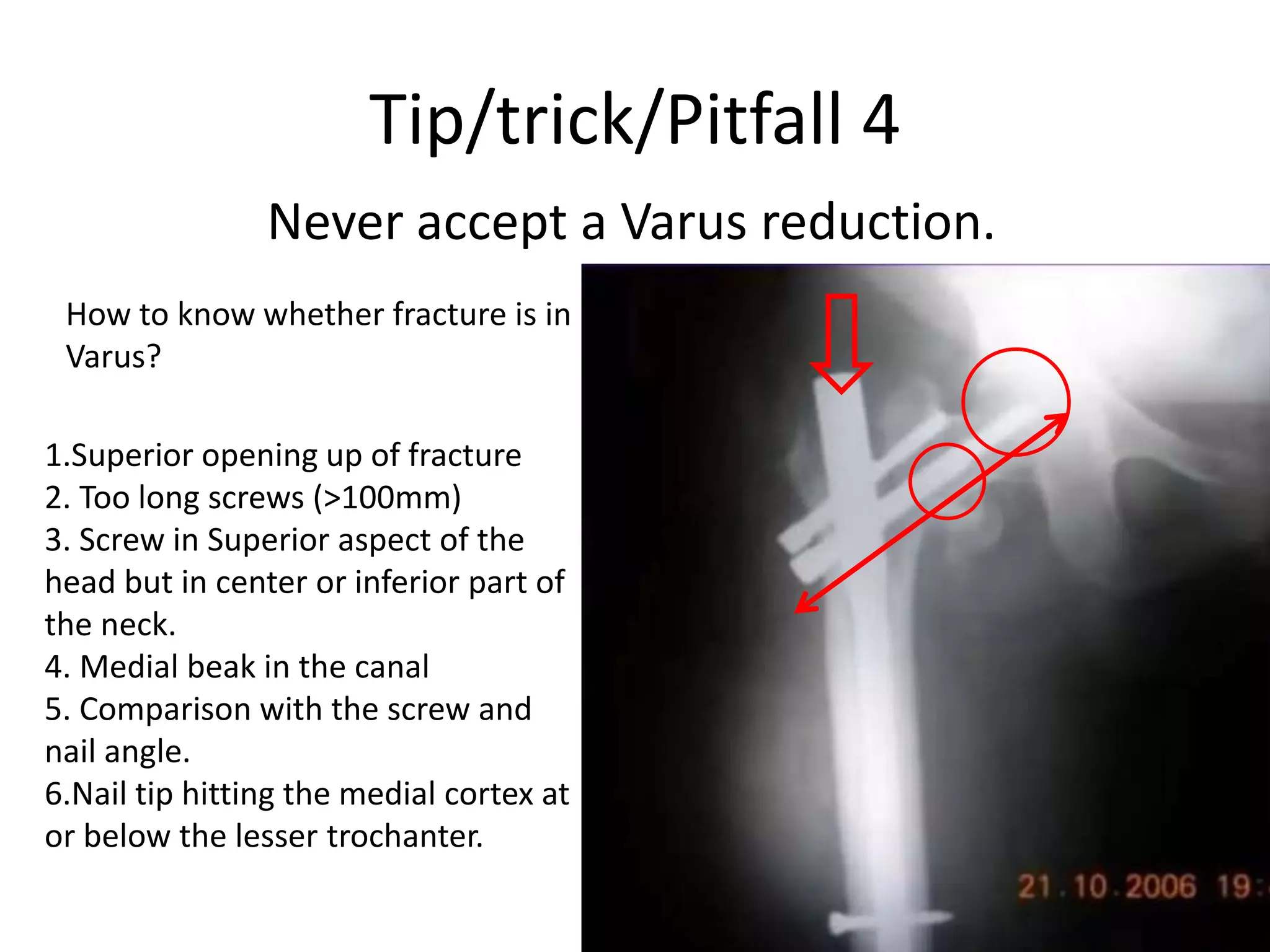
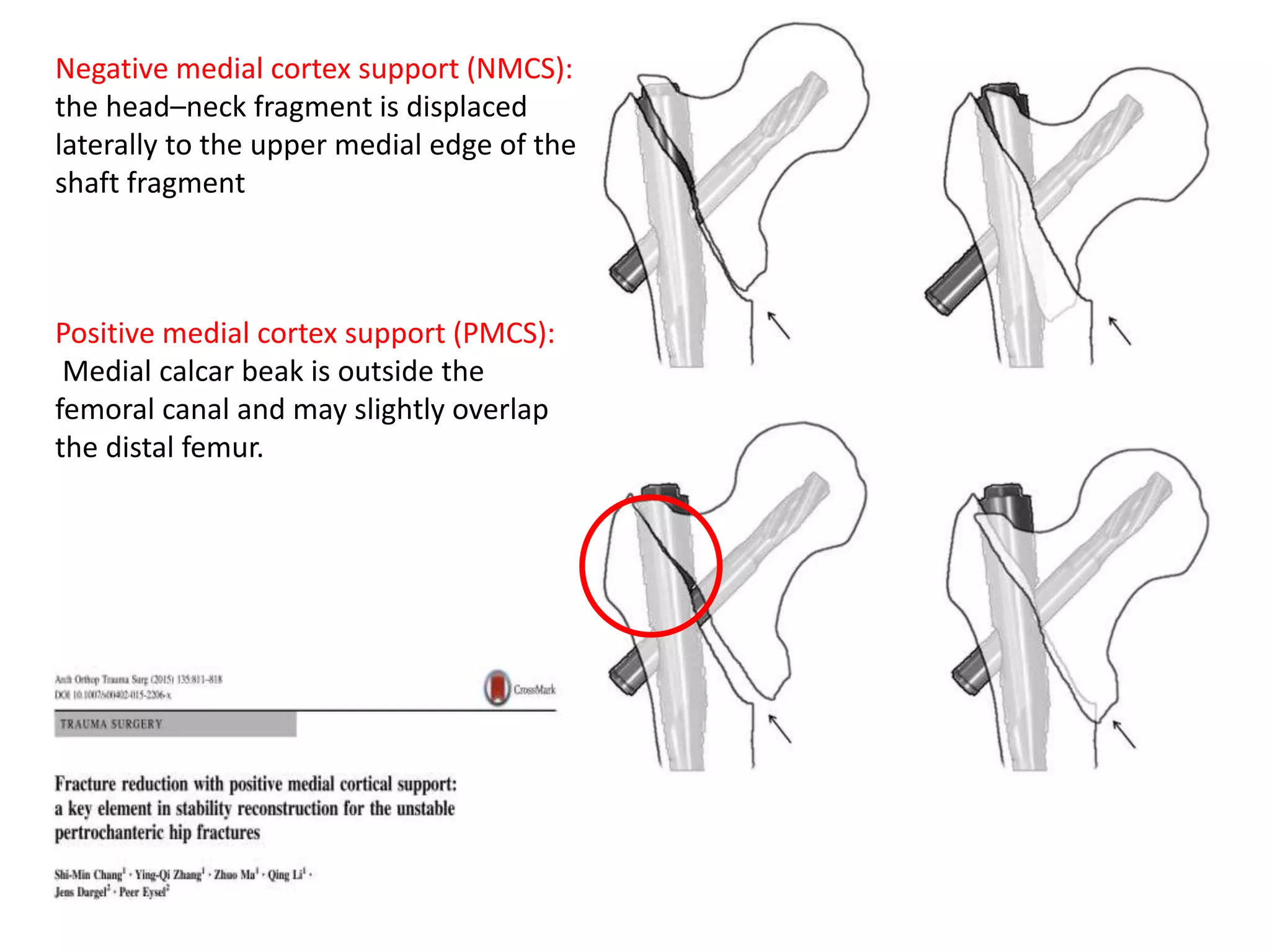
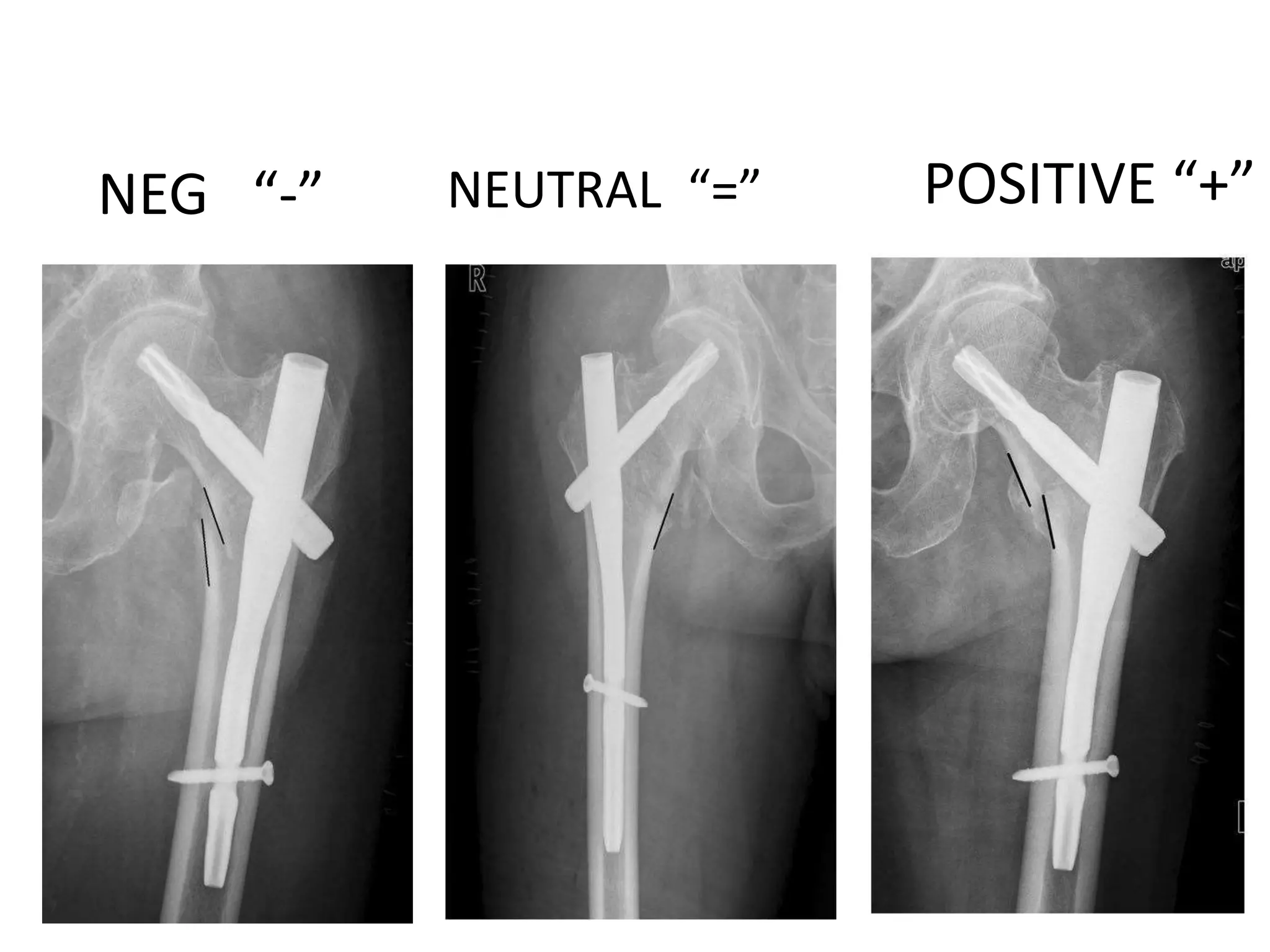
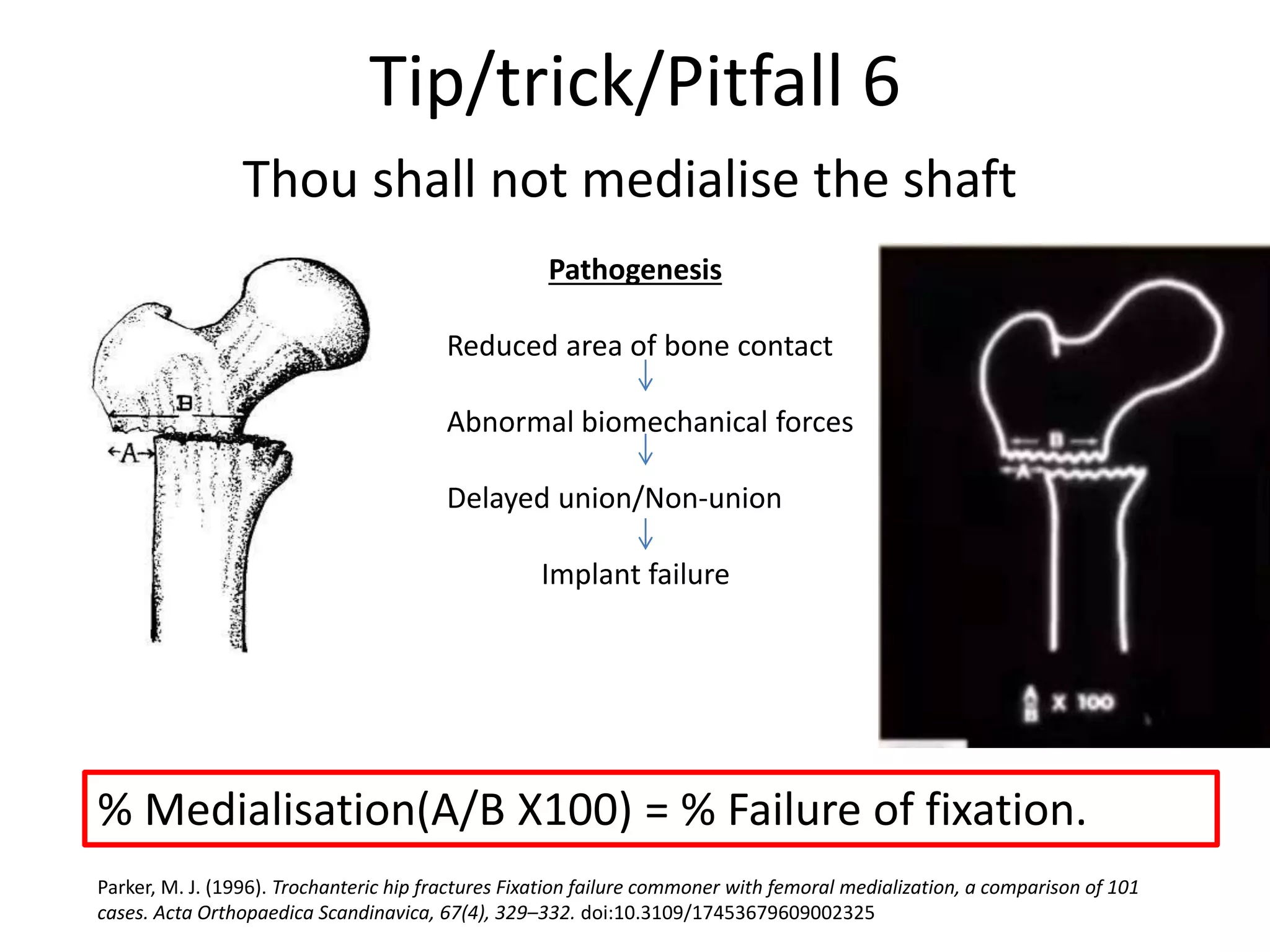
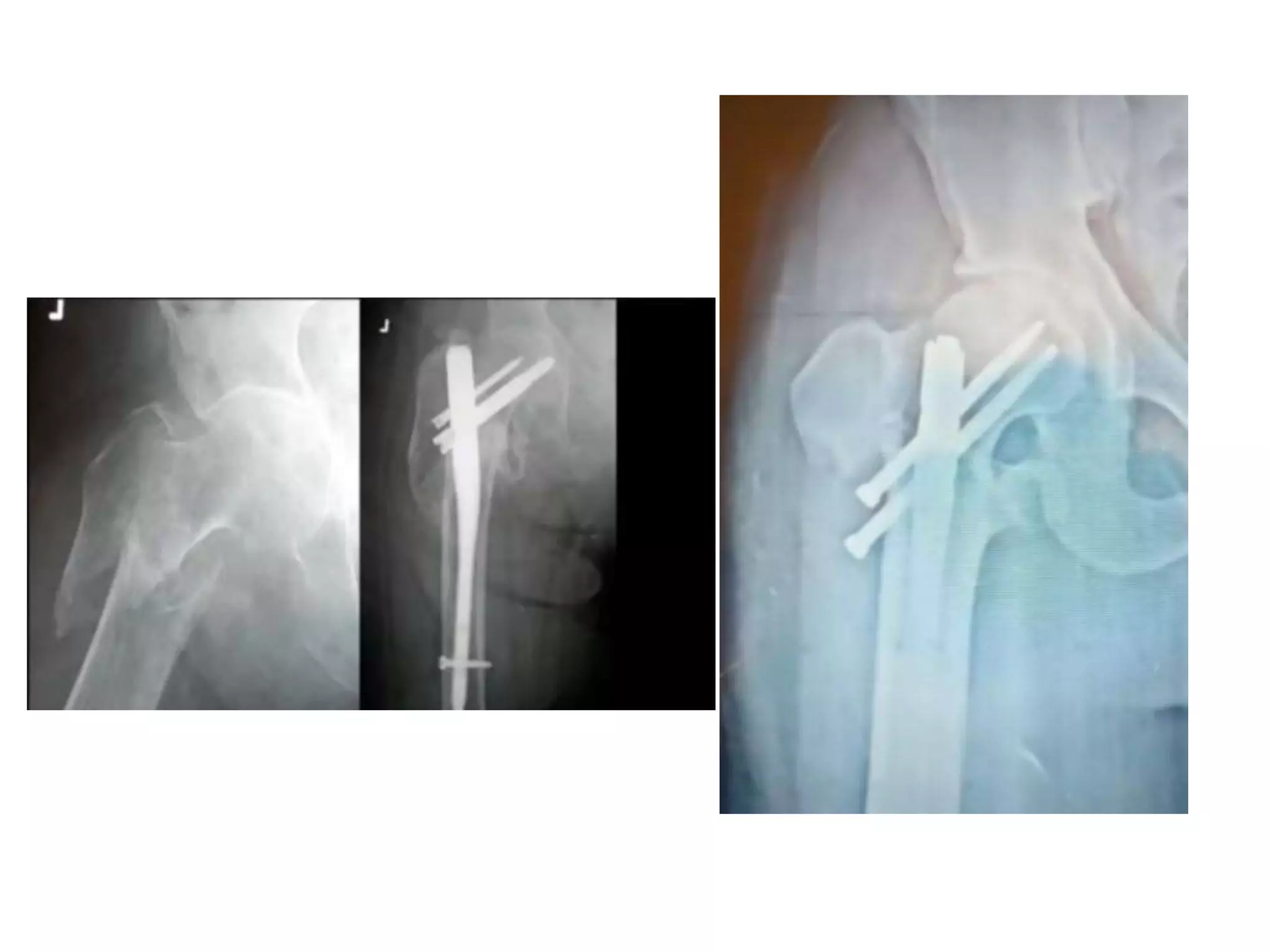
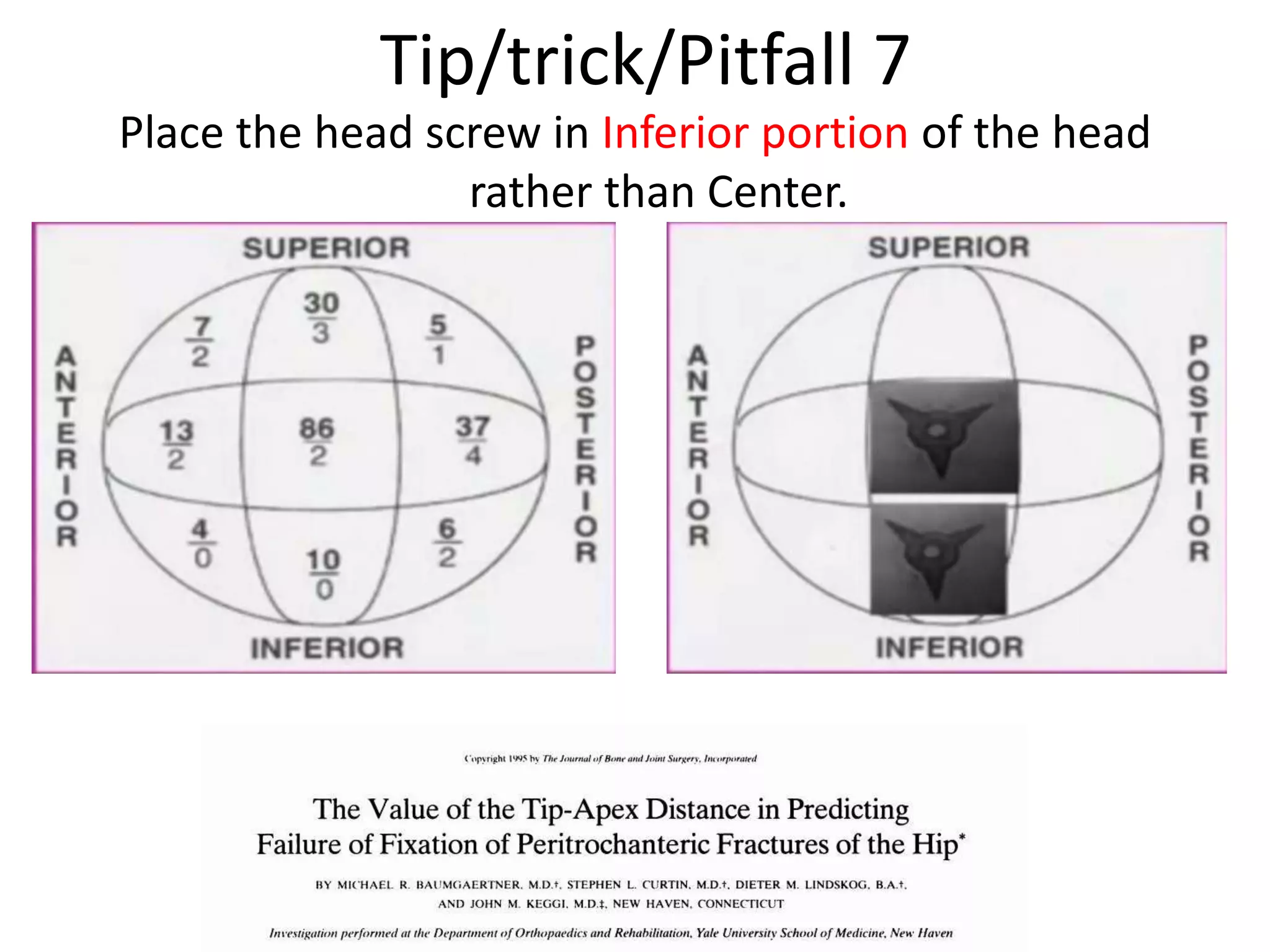
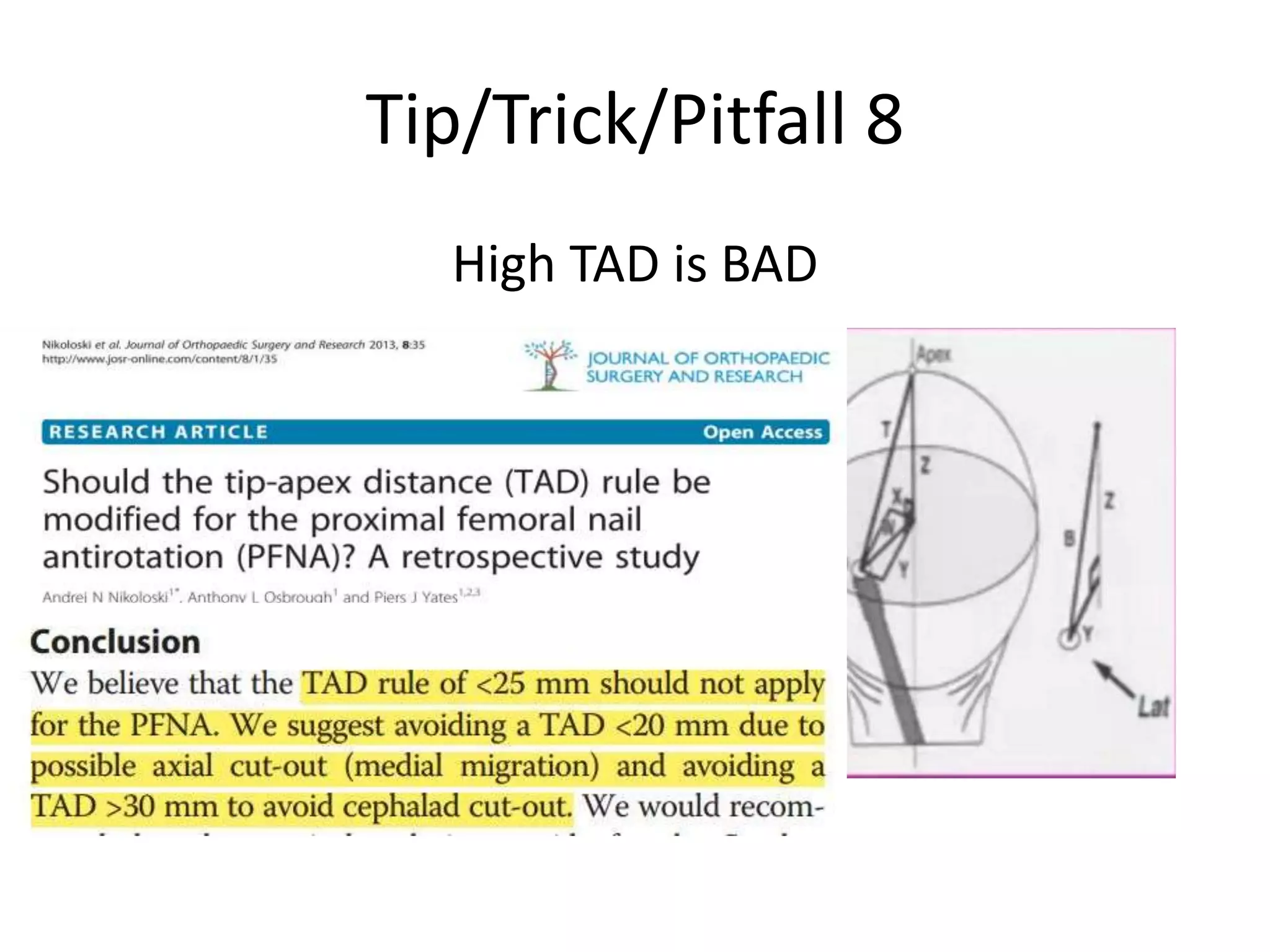
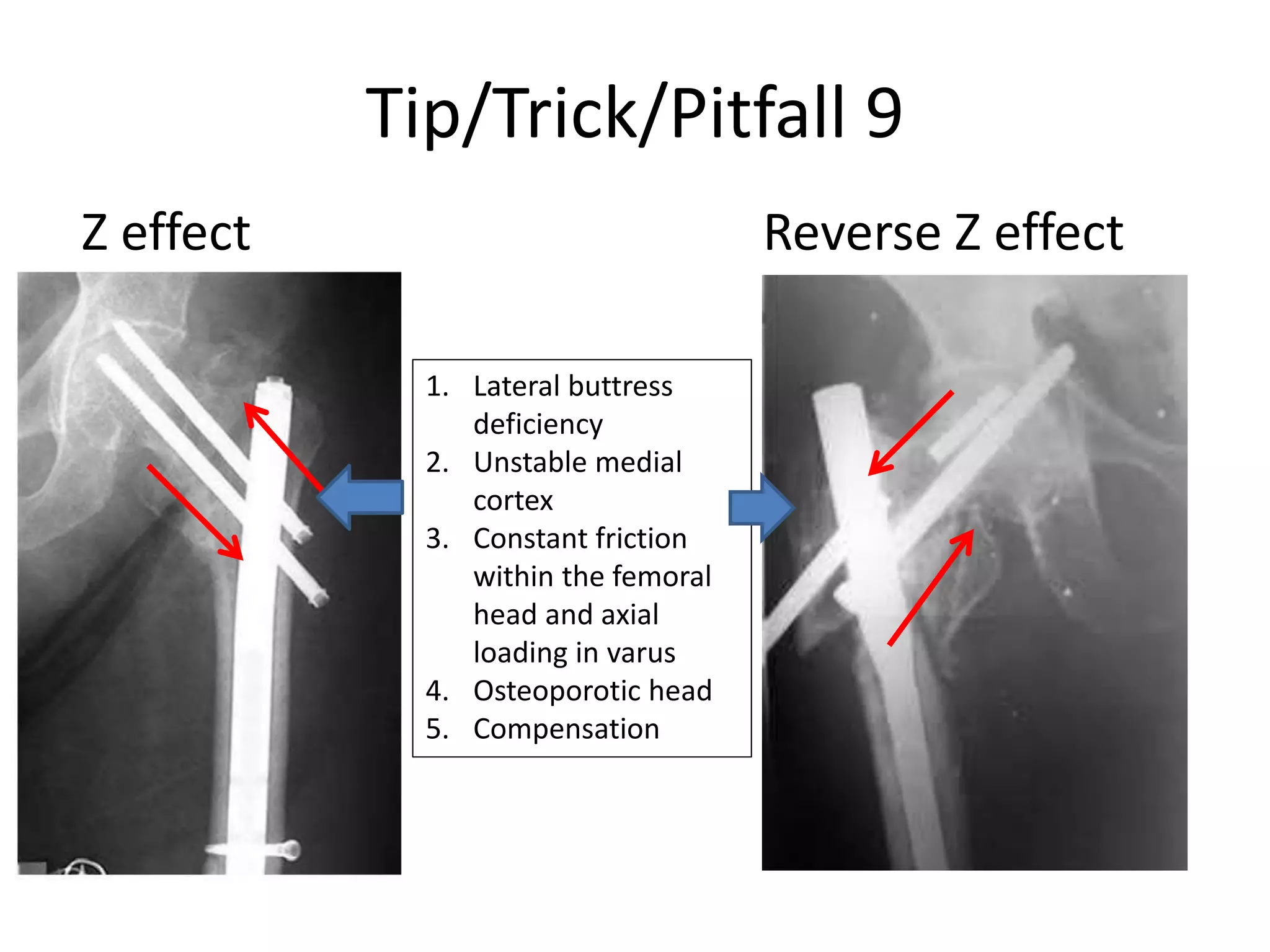
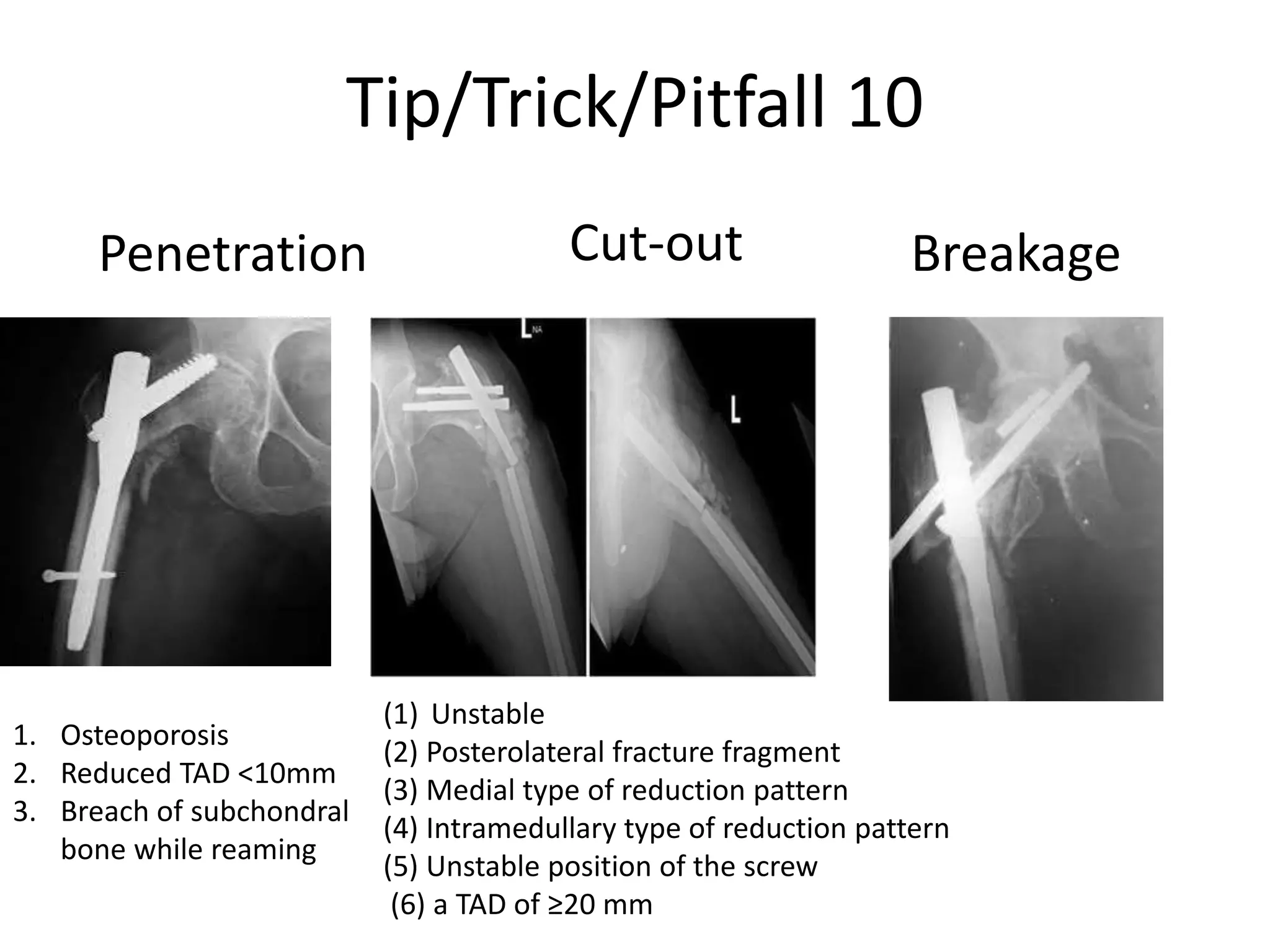
3. Factors such as varus reduction, medializing the shaft, high tip-apex distance, and penetration of the femoral head can lead to poor outcomes like nonunion.