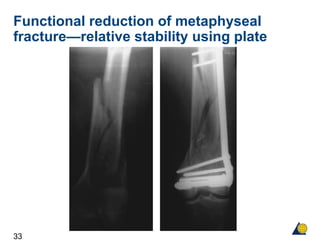
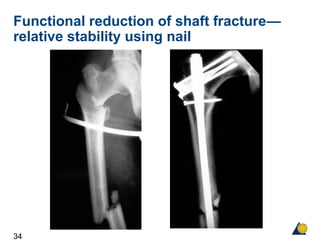
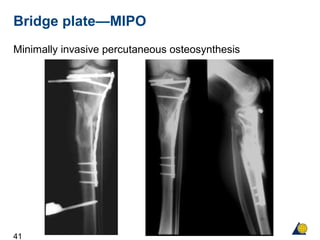
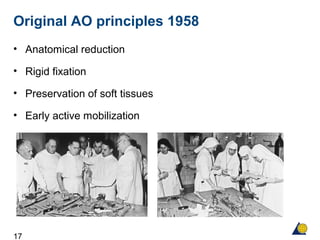
The document outlines the evolution of AO principles from their founding in 1958 to present day. The original principles emphasized anatomical reduction, rigid fixation, and preservation of soft tissues. However, over time the principles shifted to emphasize functional reduction, stable fixation, and preservation of blood supply as it was realized this approach better supported biological healing. The document traces this evolution from the original AO pioneers to modern techniques like minimally invasive plating that further the goal of improving patient outcomes.



![30
Improve the biology—change the
mechanics
“Callus is like sex— it’s natural, it joins two things
together and it requires a bit of movement”
[A Apley]](https://image.slidesharecdn.com/aophilosophy-160422012235/85/Ao-philosophy-30-320.jpg)