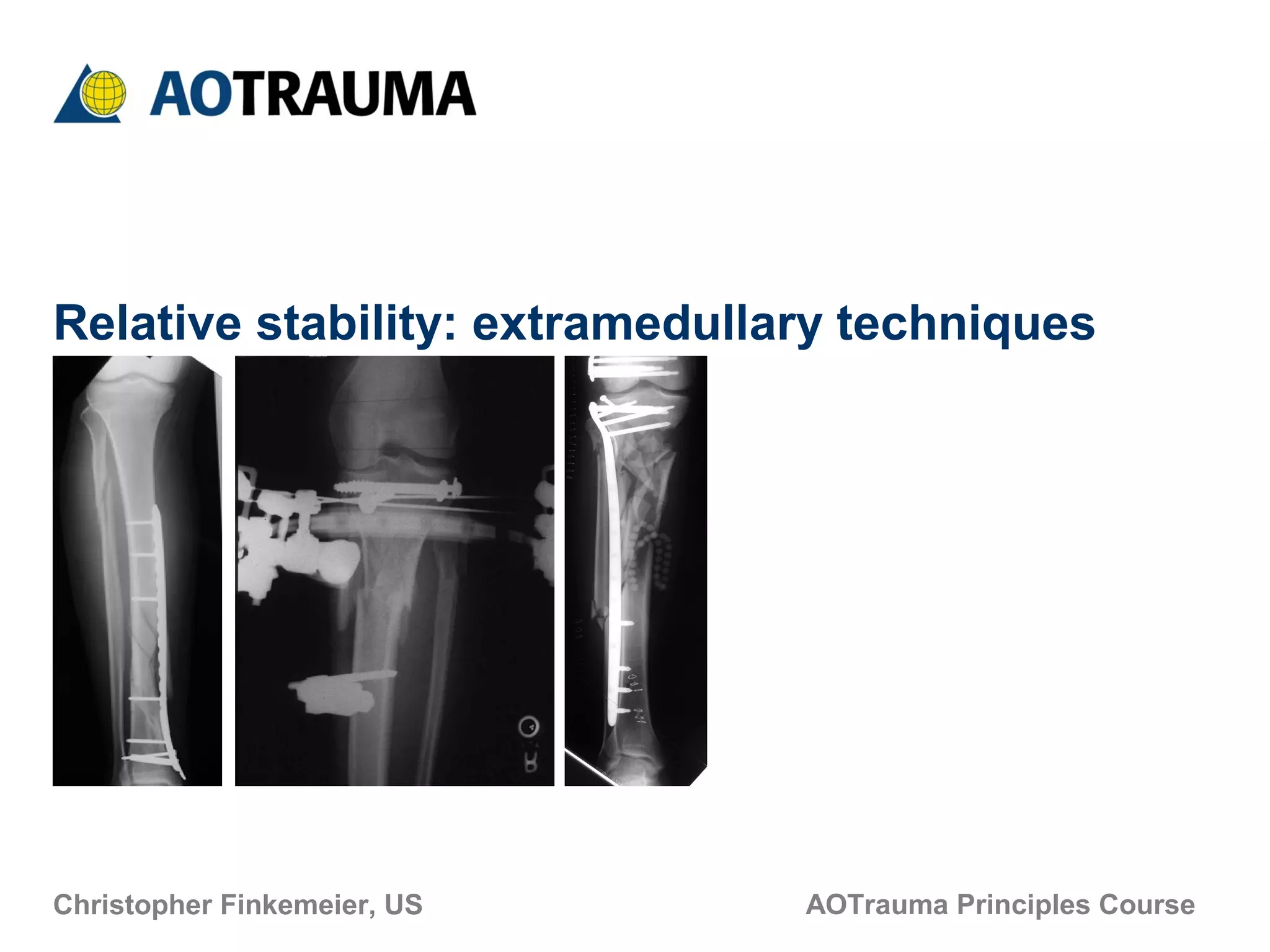
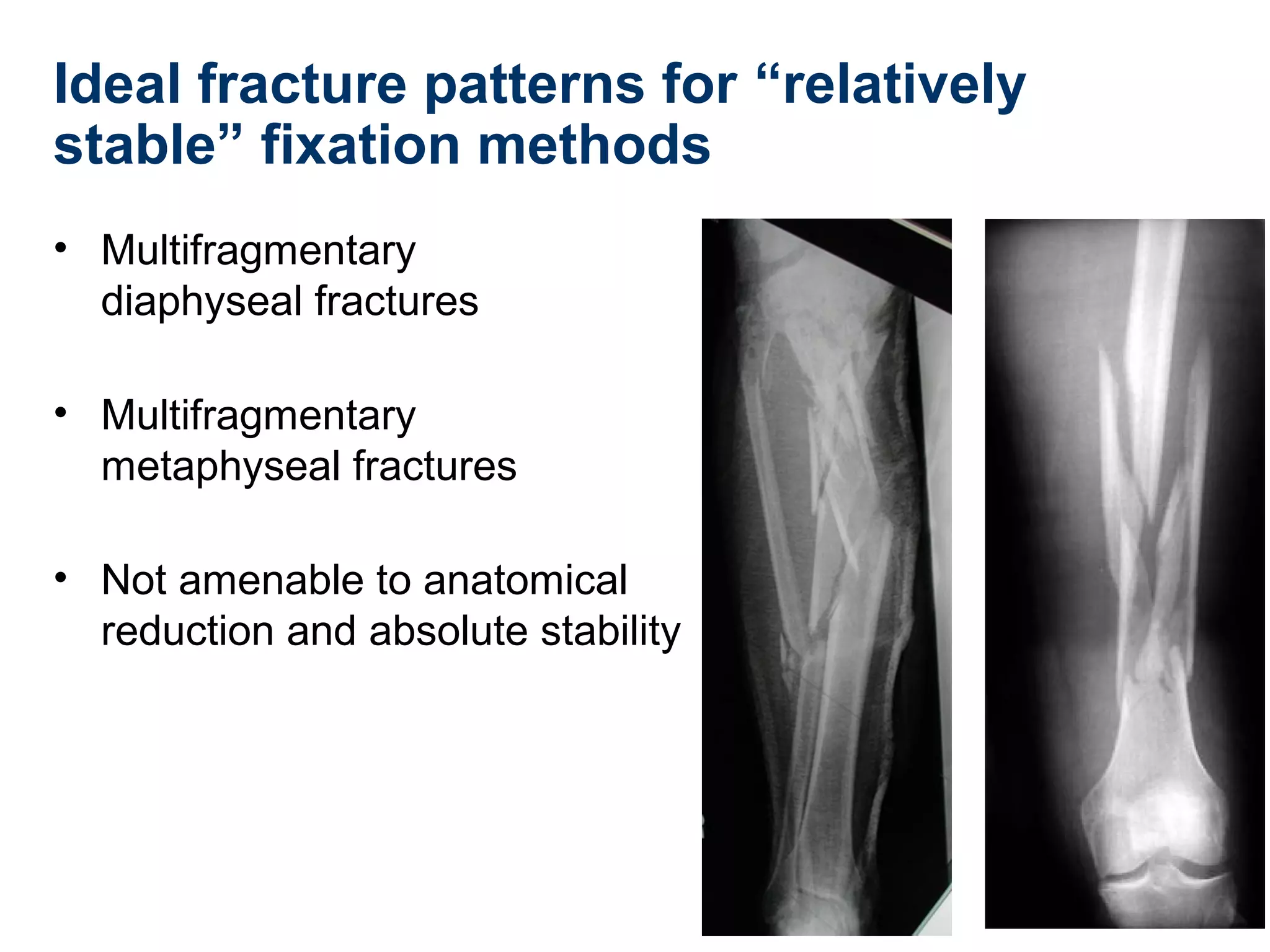
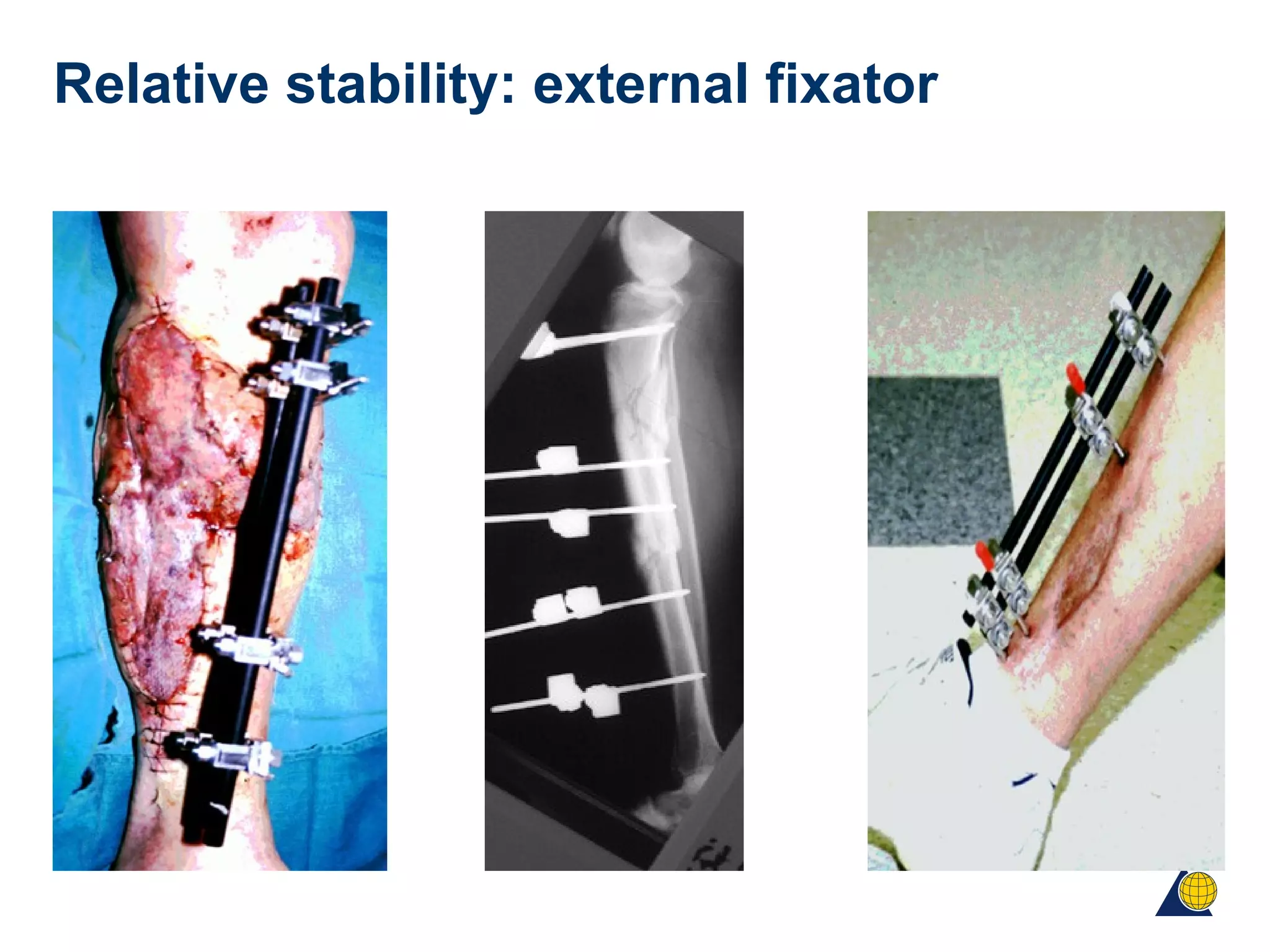
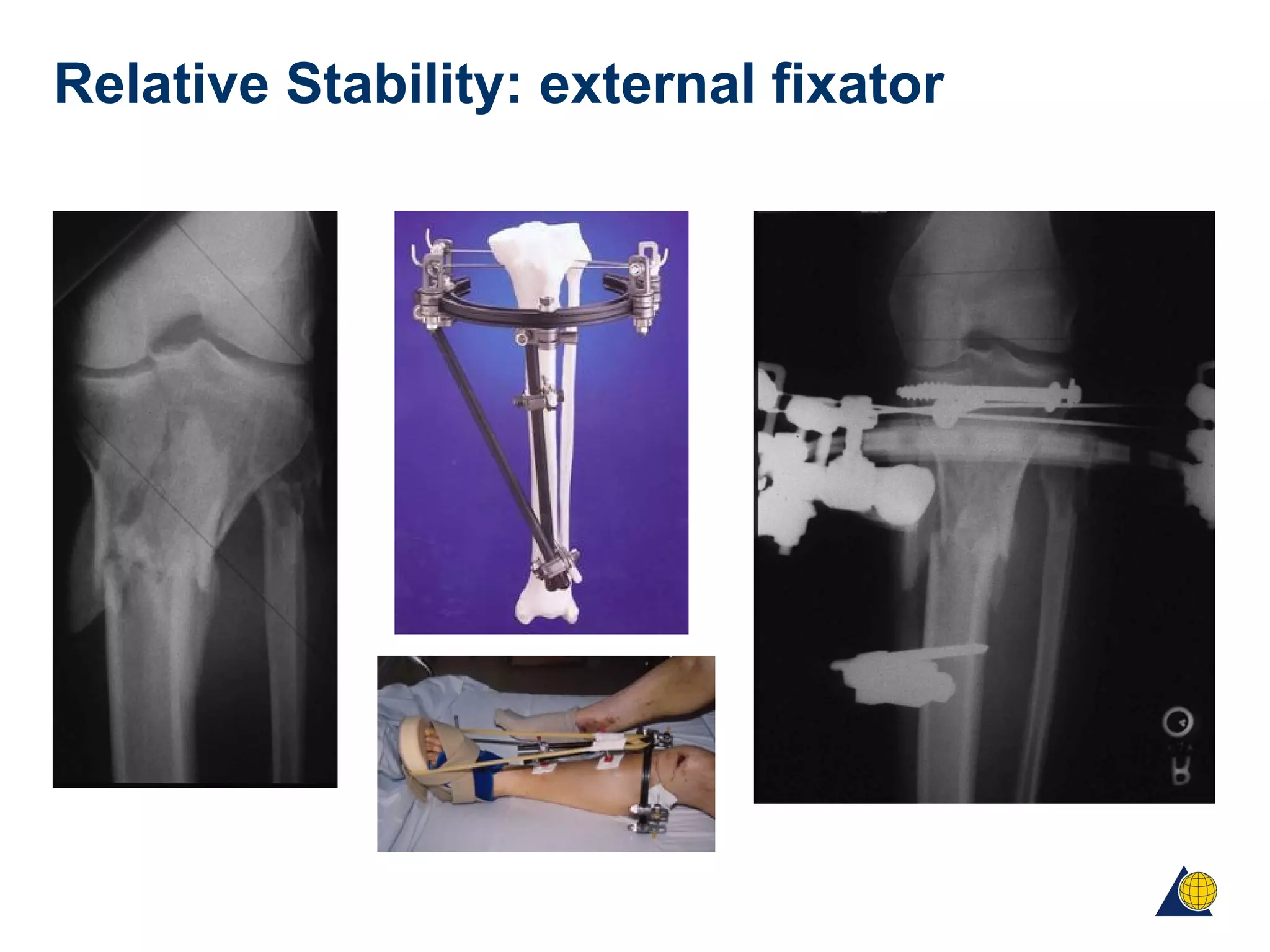
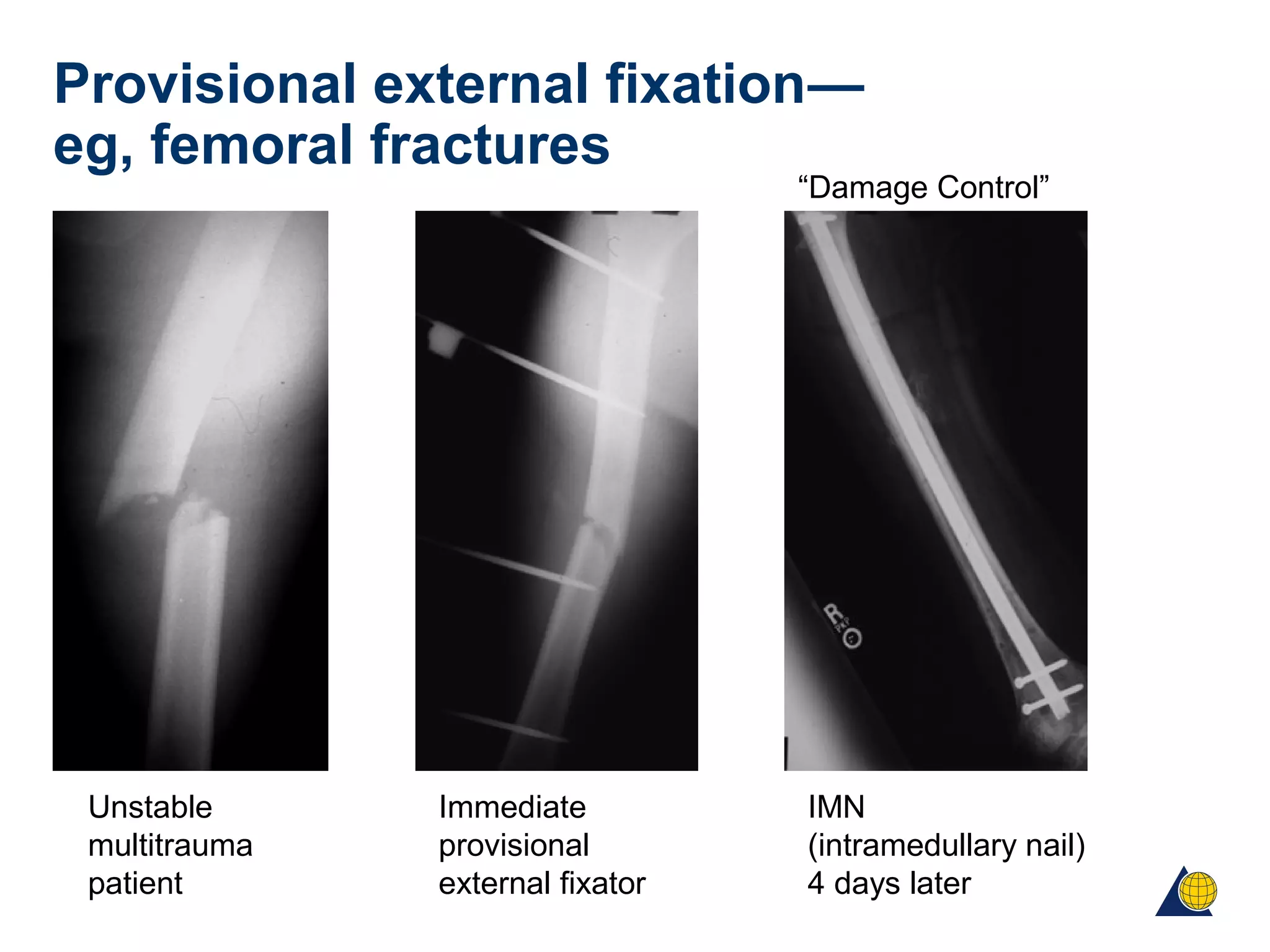
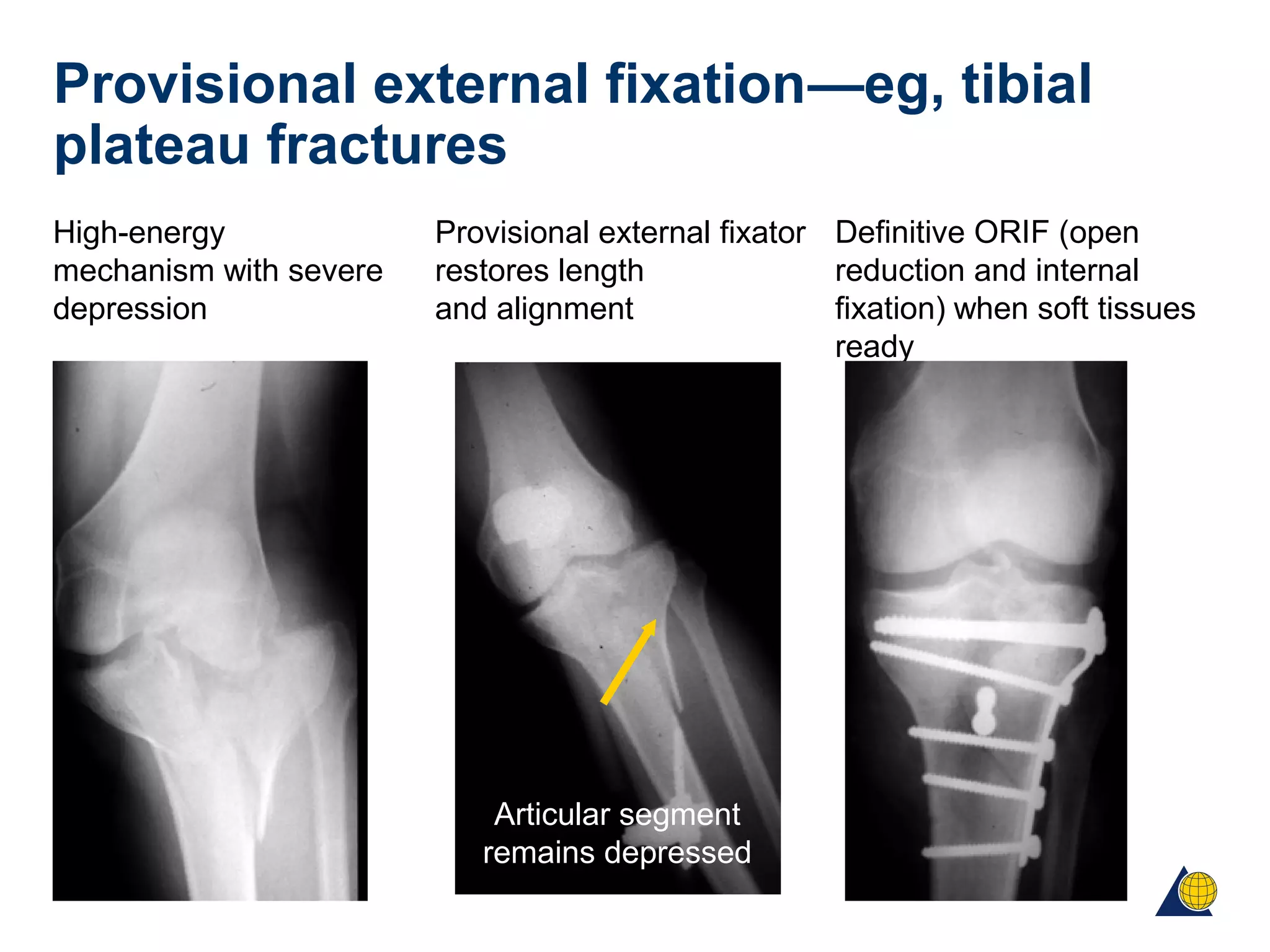
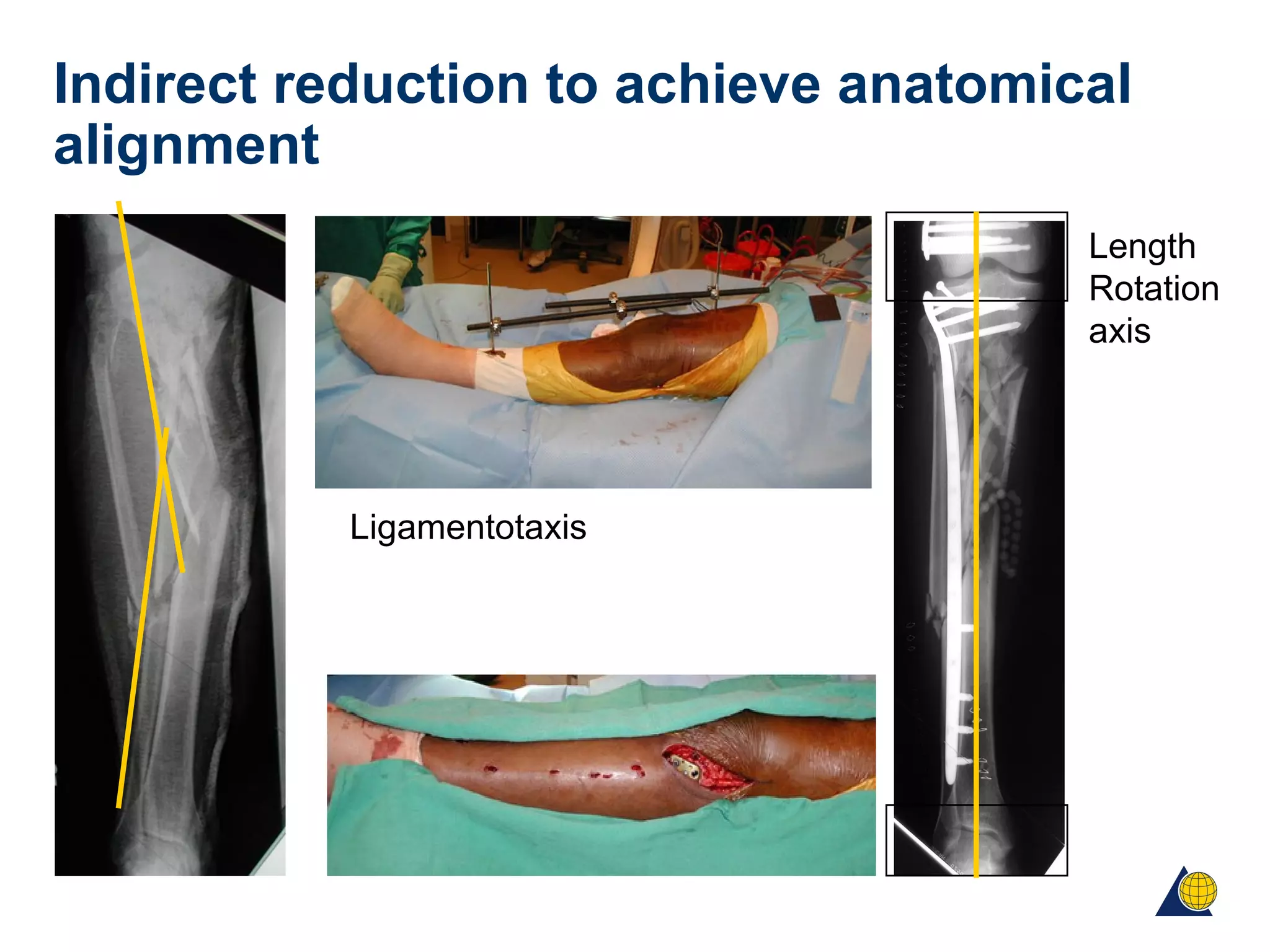
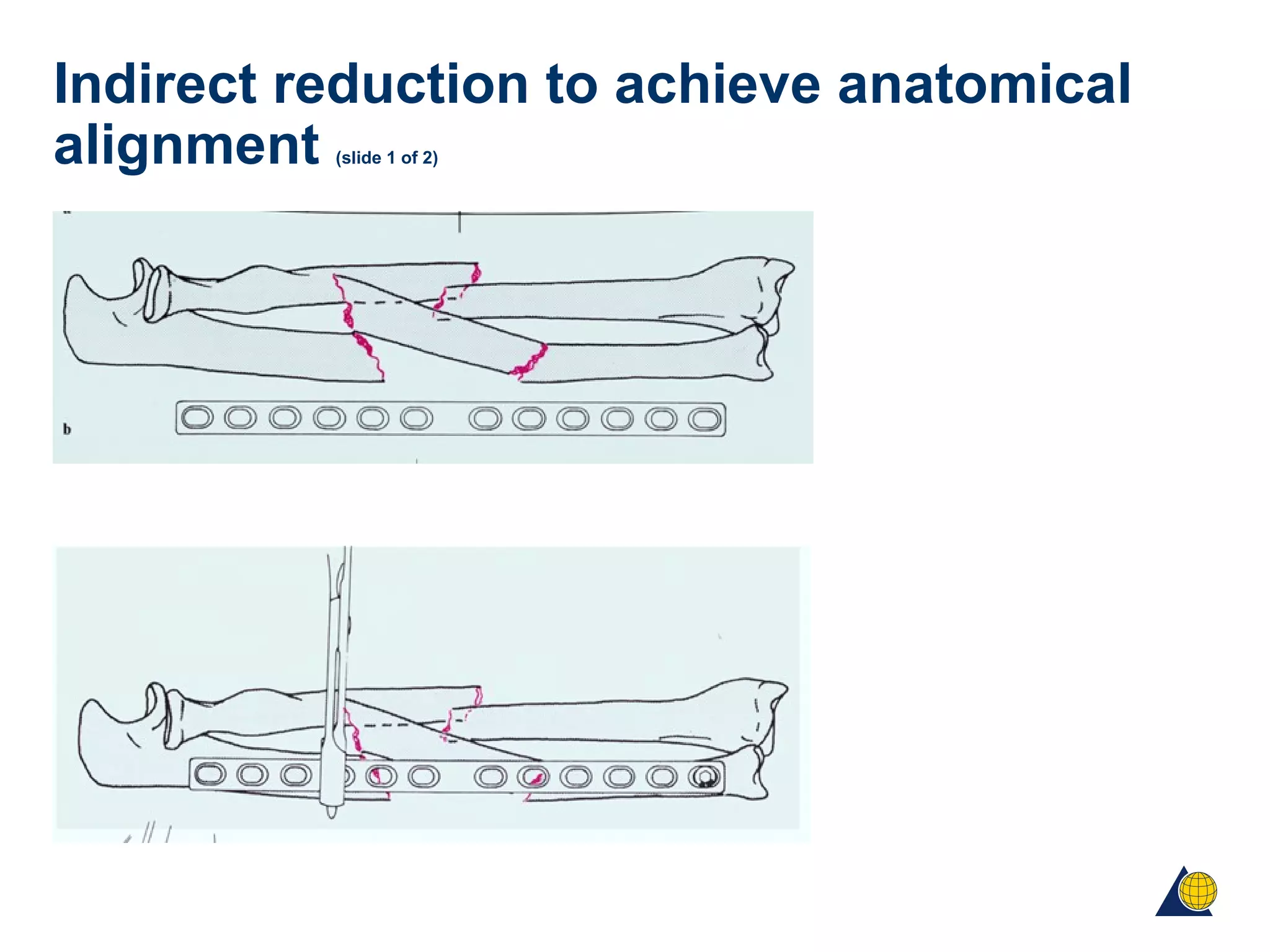
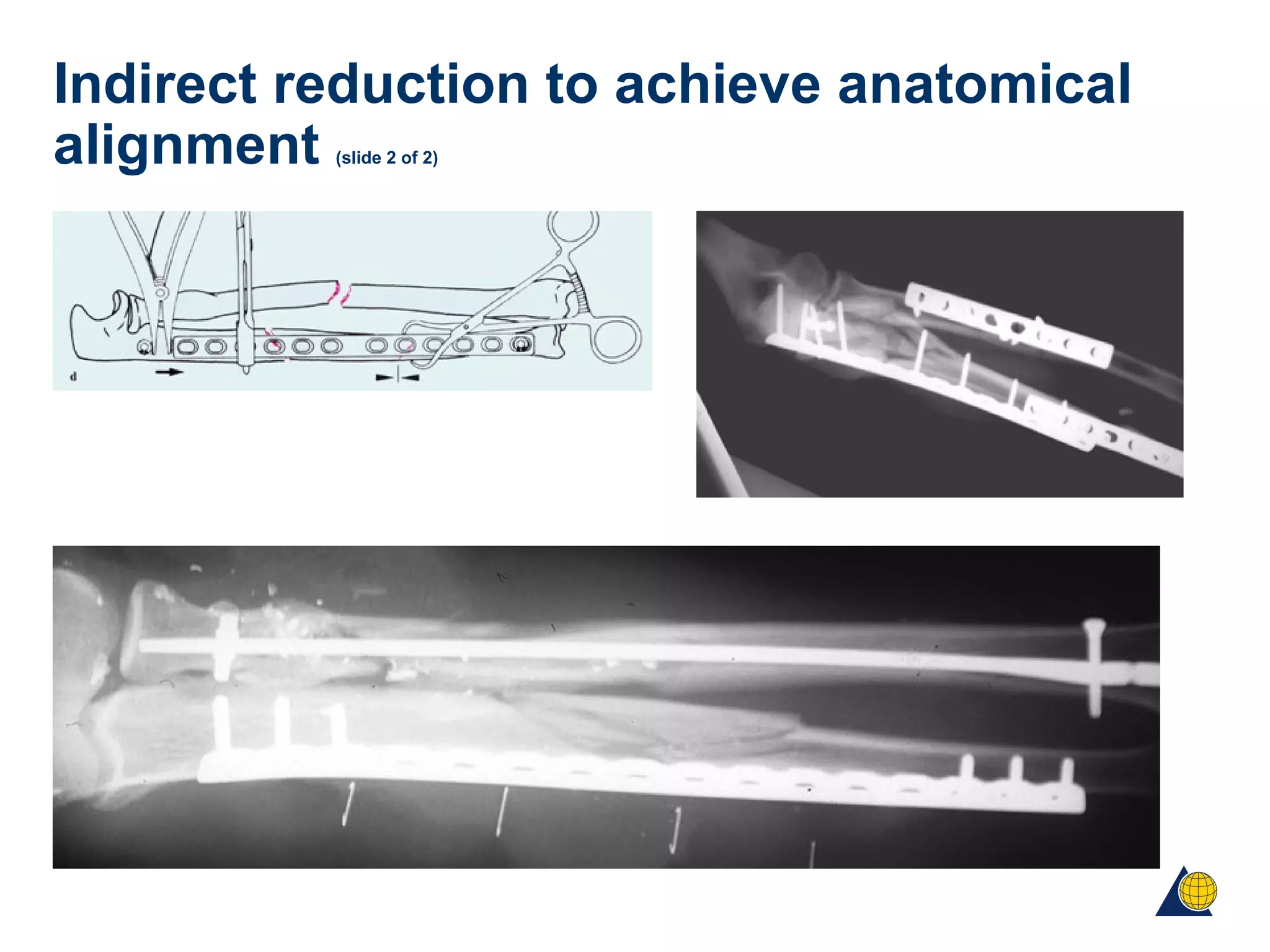
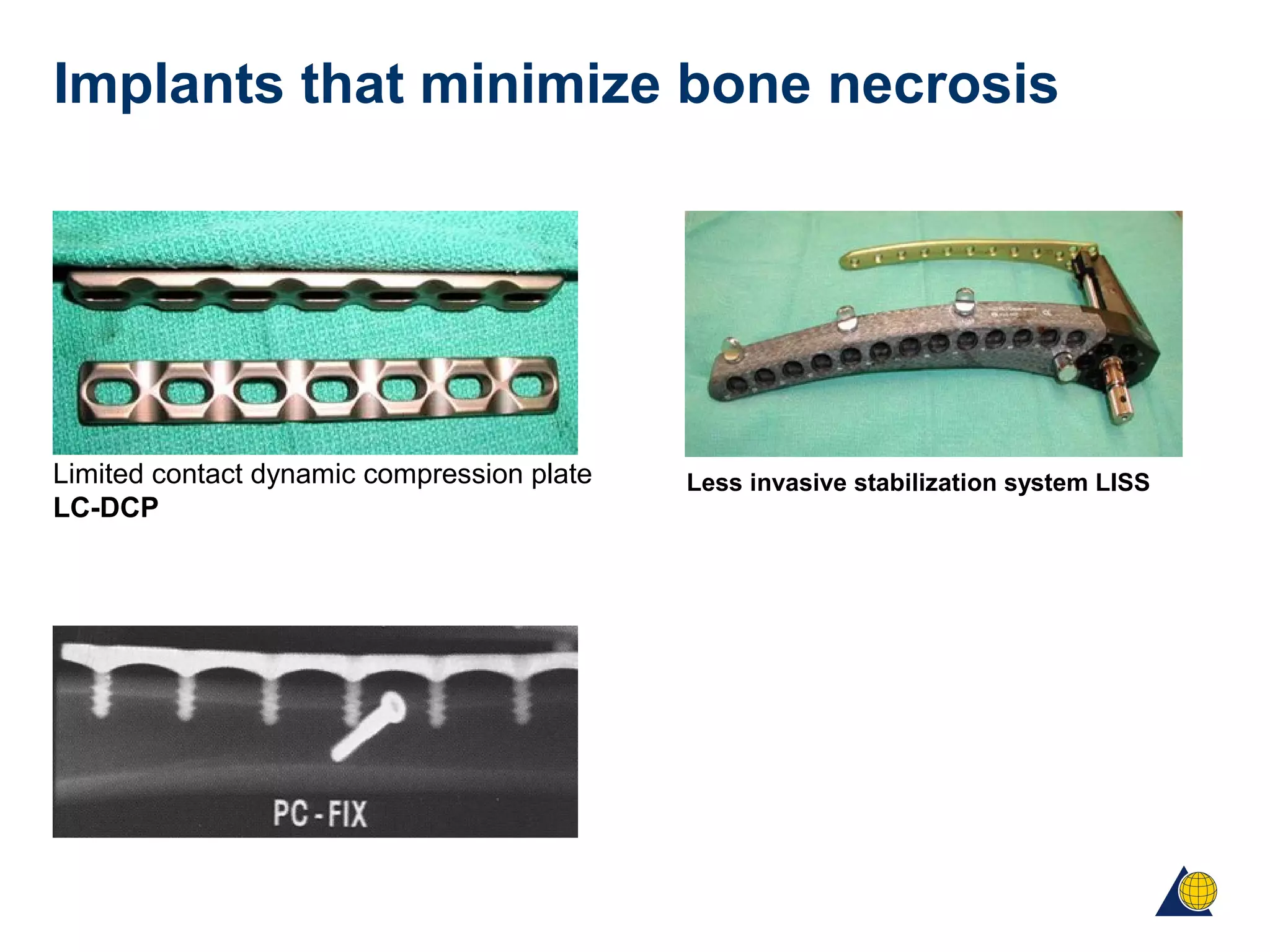
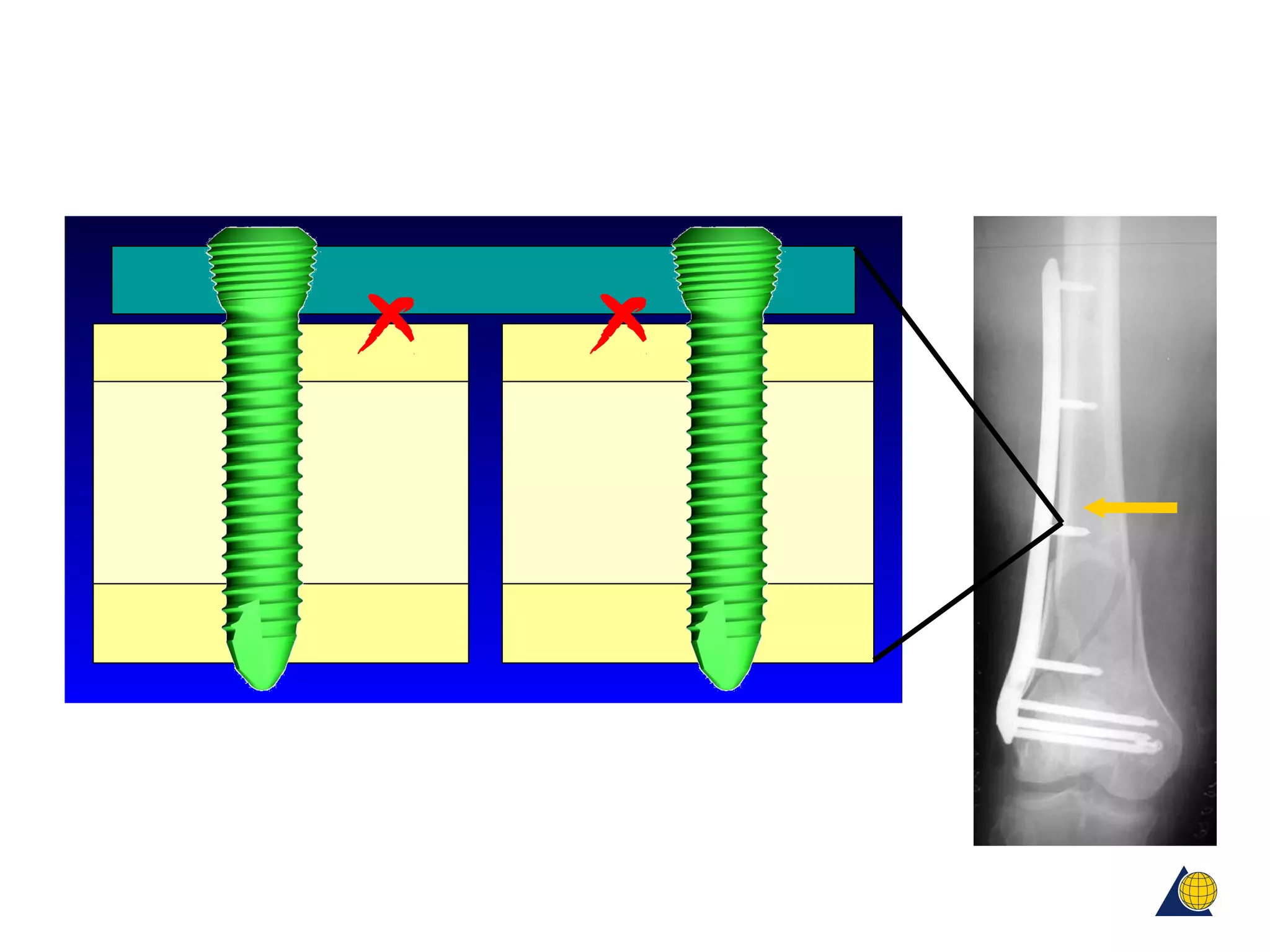
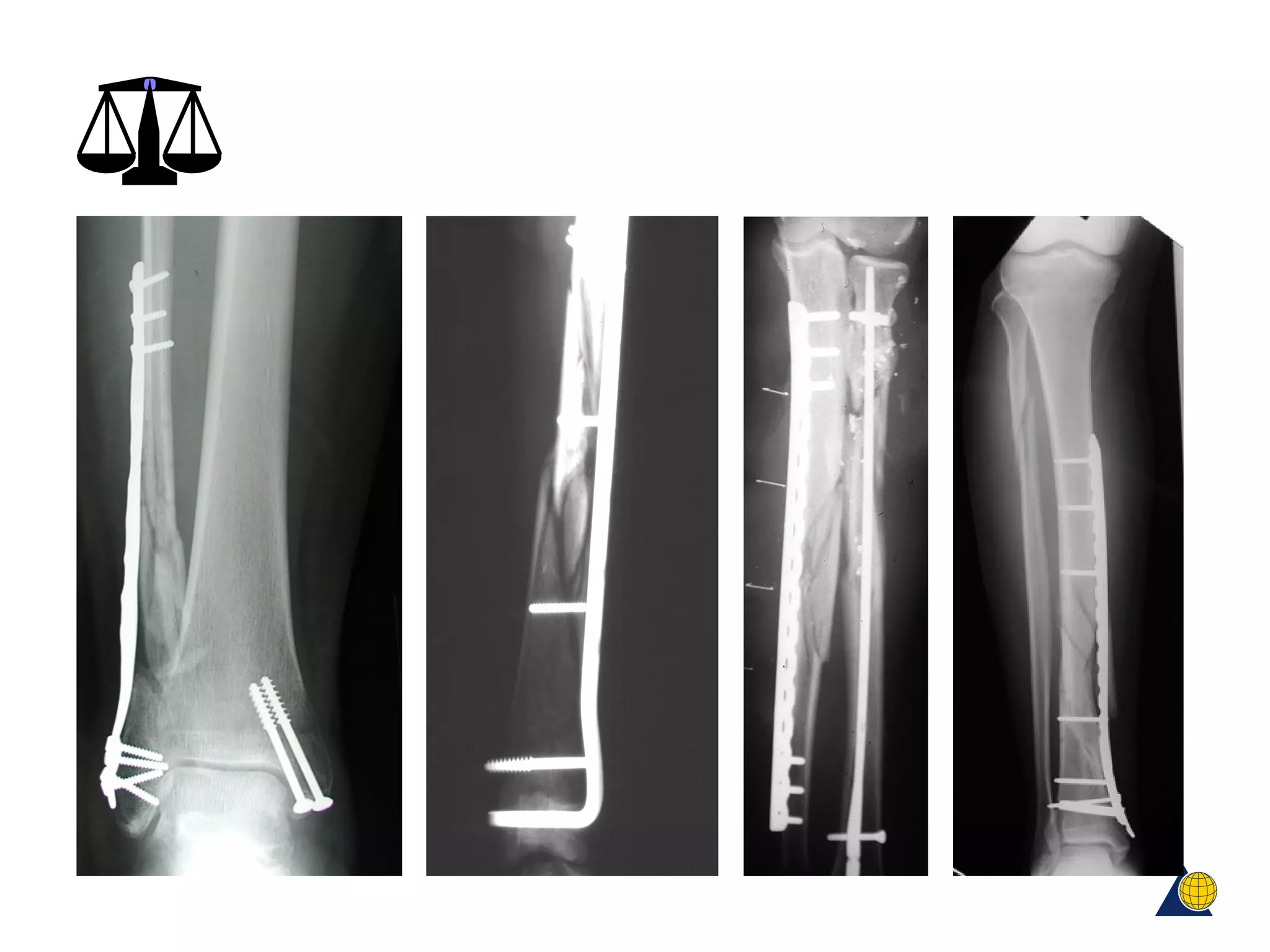
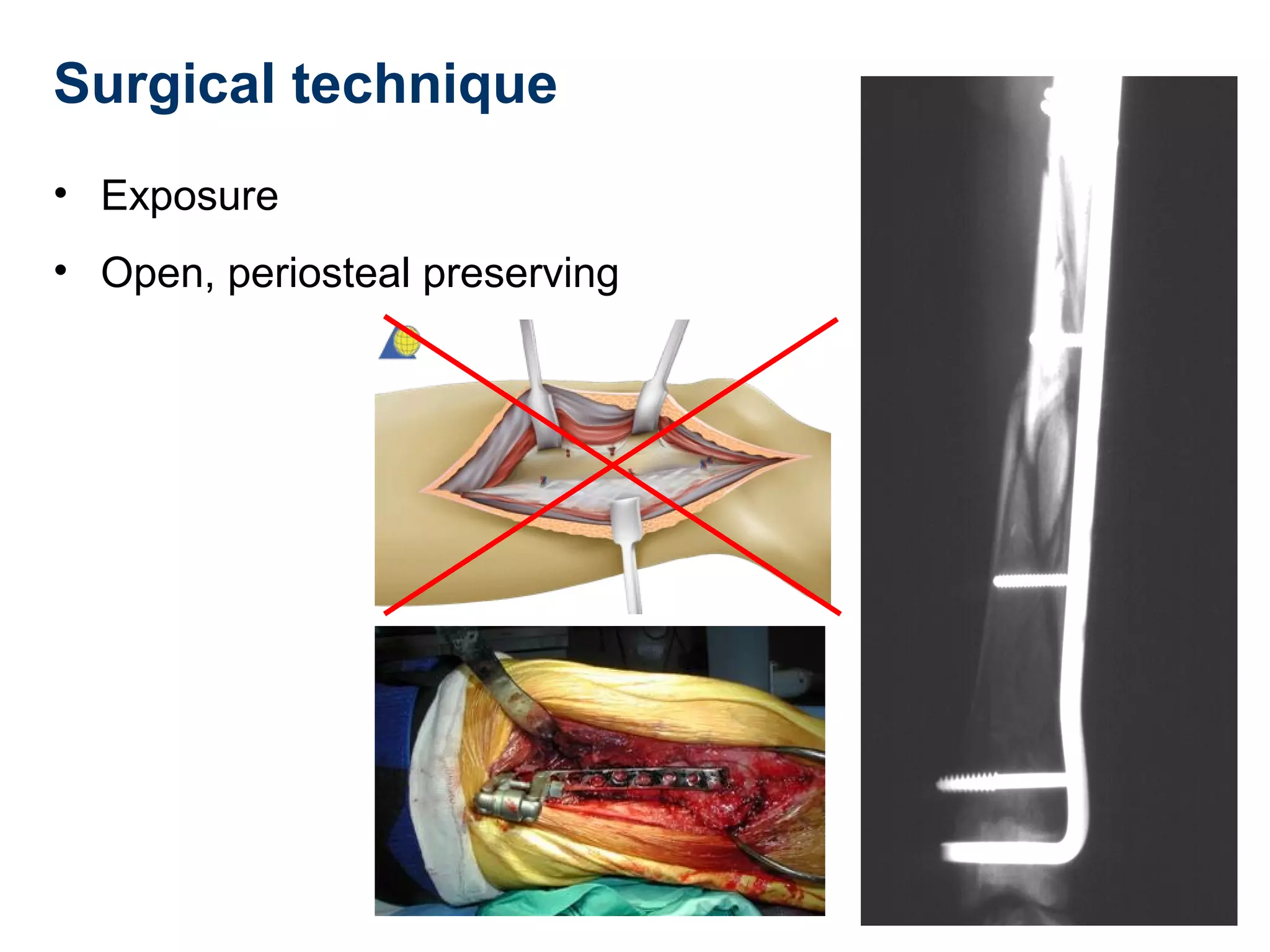
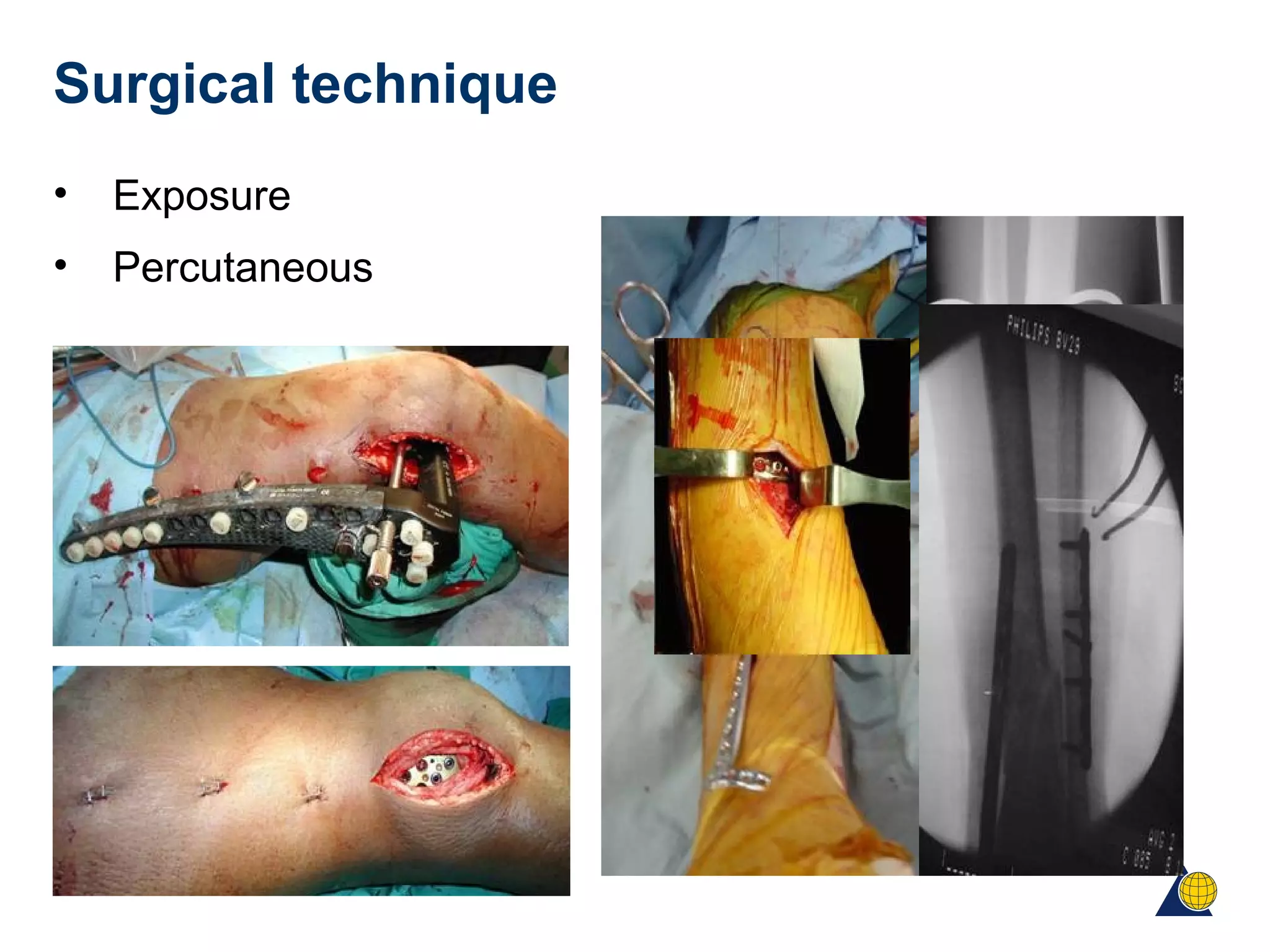
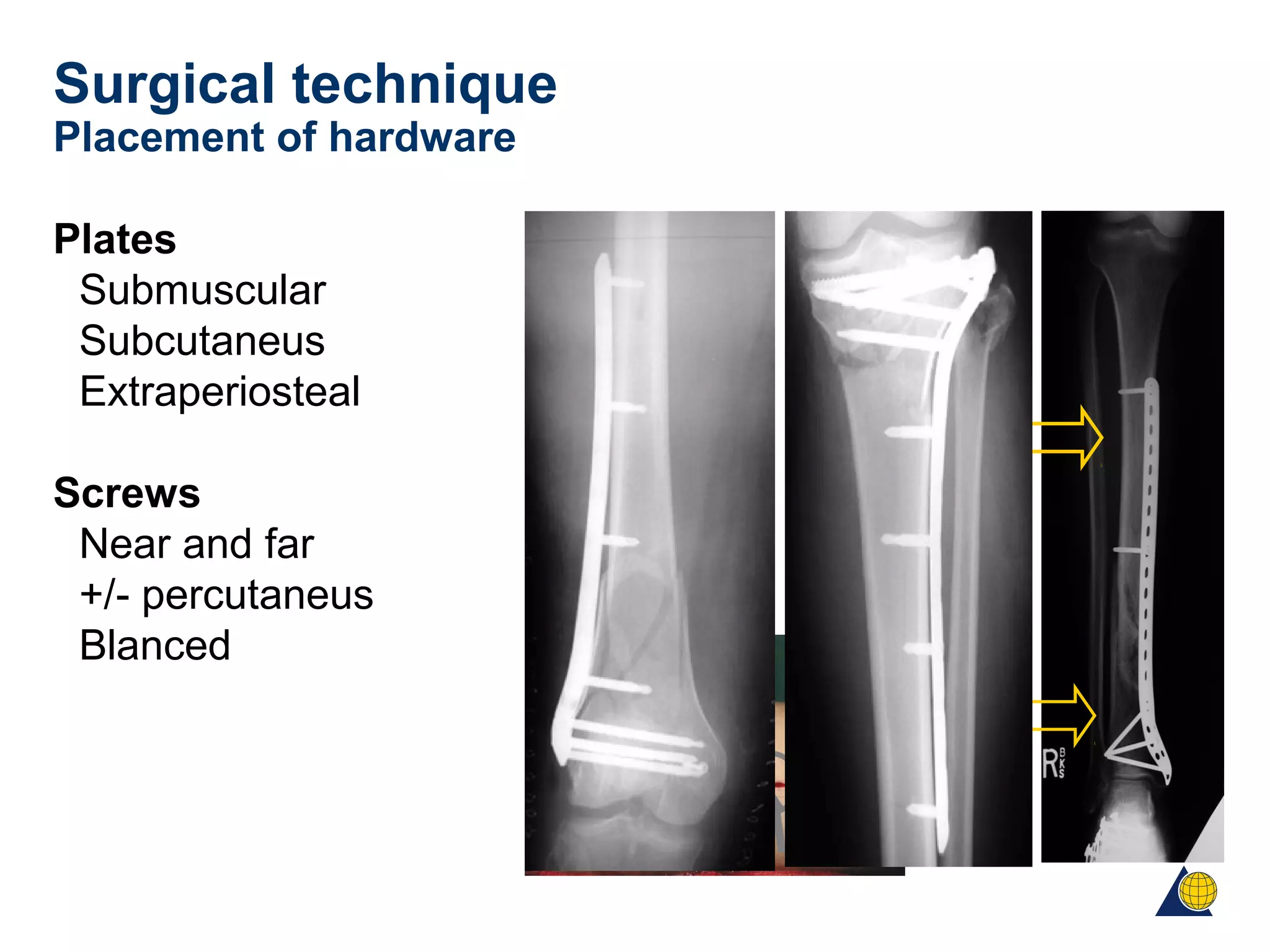
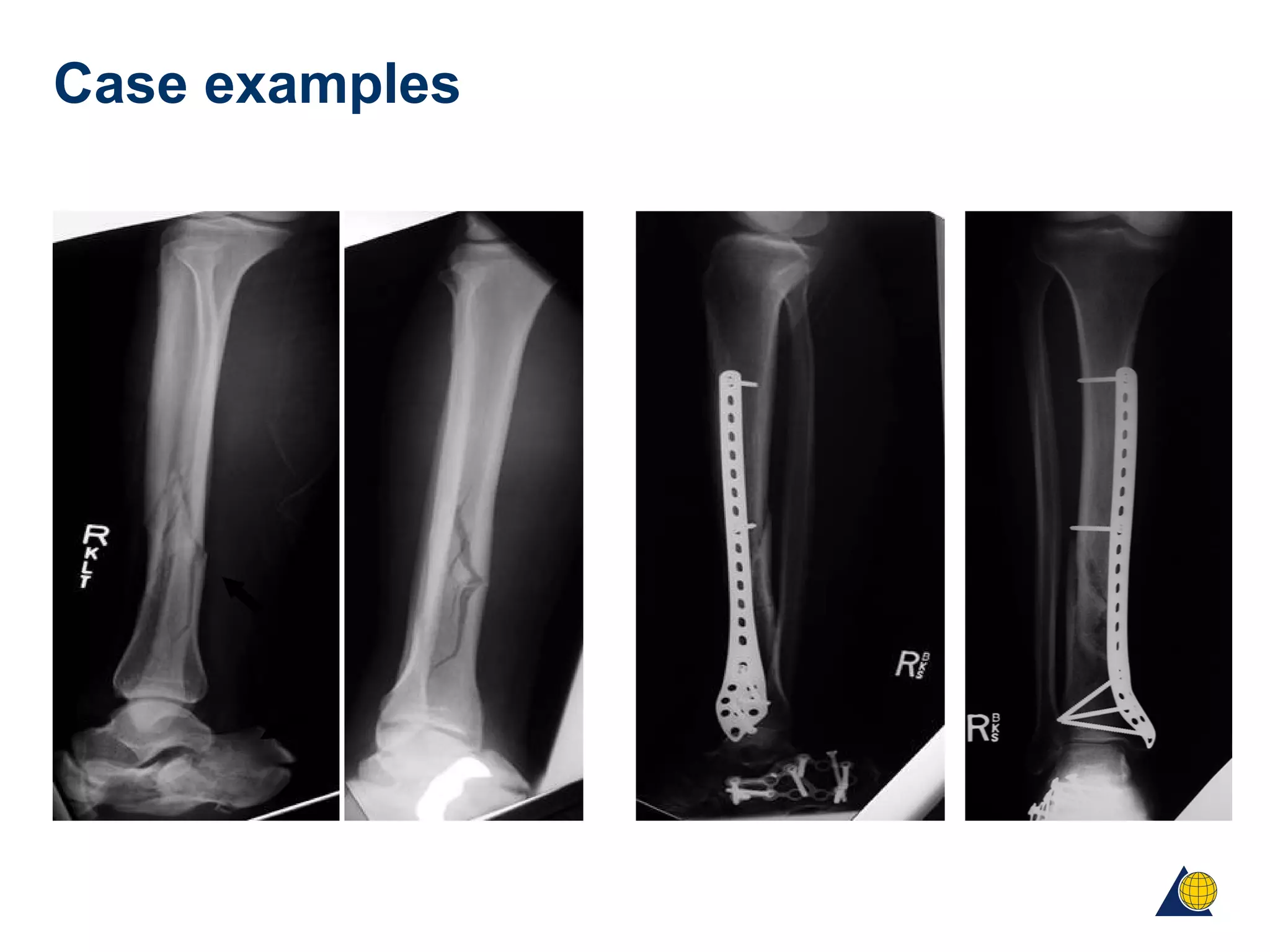
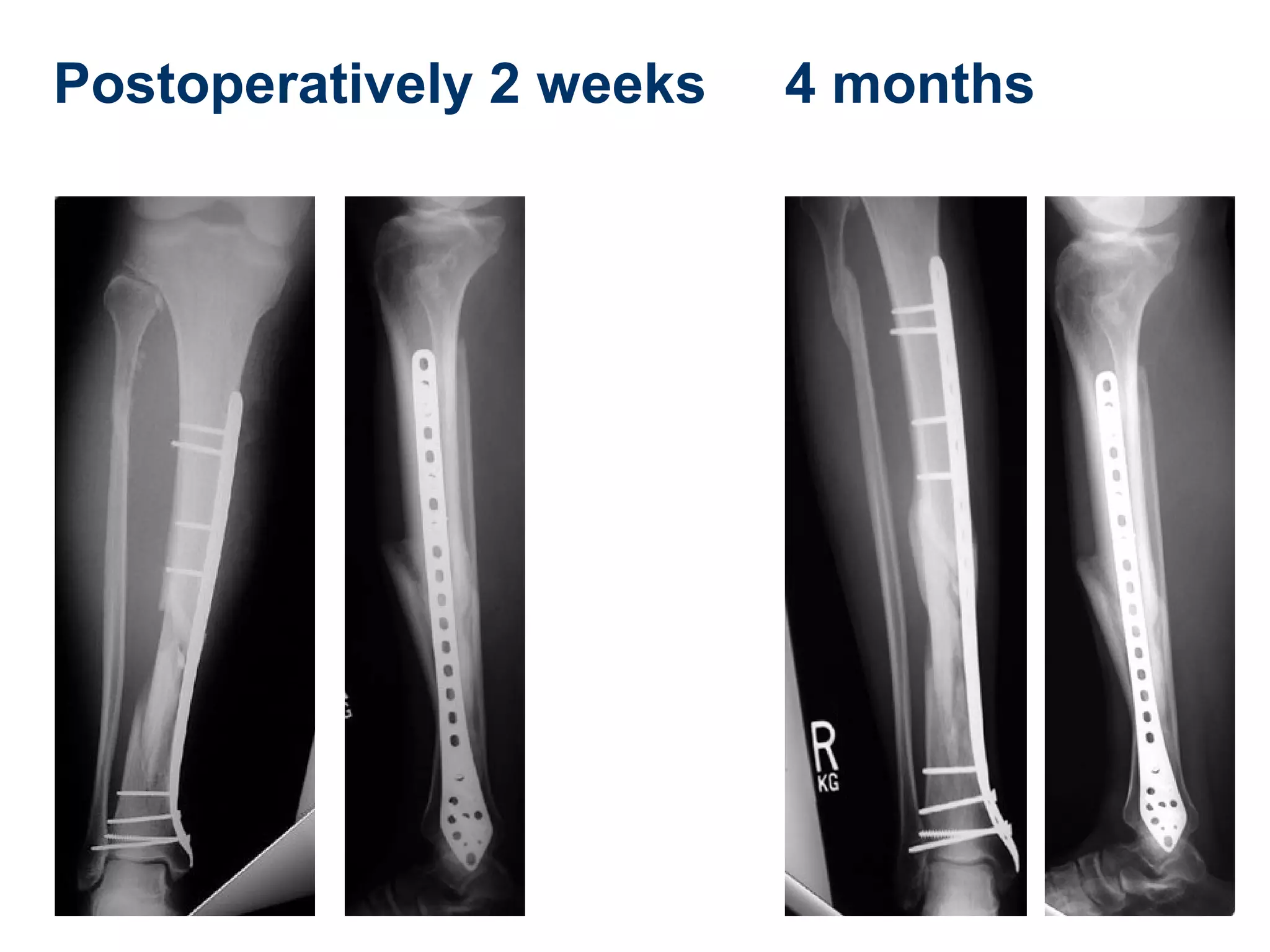
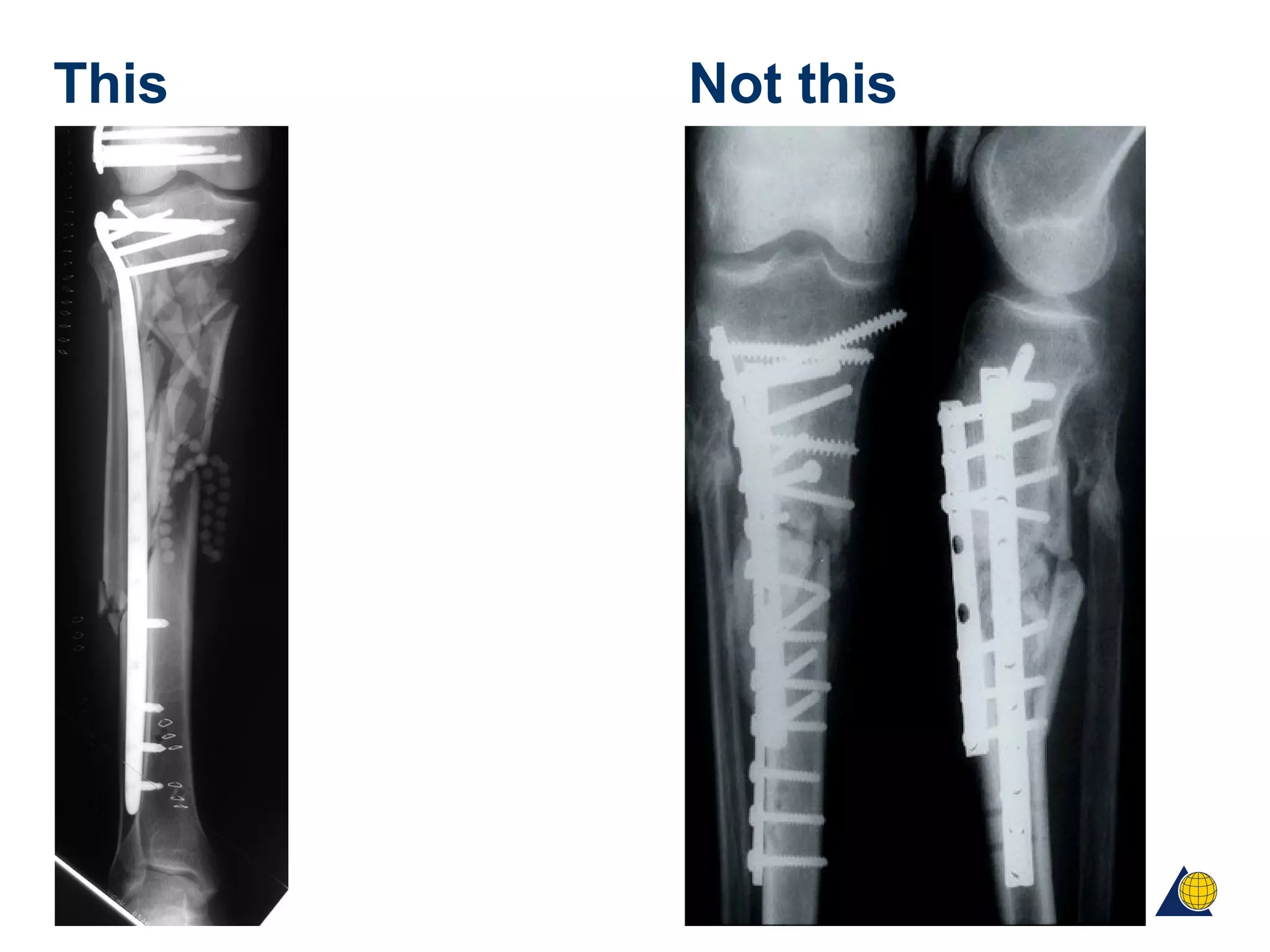
This document discusses techniques for obtaining relative stability in fractures using extramedullary fixation methods. It describes ideal fracture patterns for relatively stable fixation, such as multifragmentary diaphyseal and metaphyseal fractures. Two common extramedullary techniques are discussed: external fixation and bridge plating. The aim of these techniques is to preserve fracture site vascularity and provide sufficient stabilization for union.