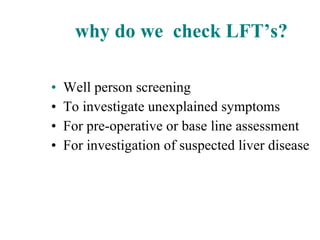
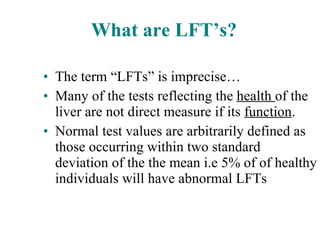
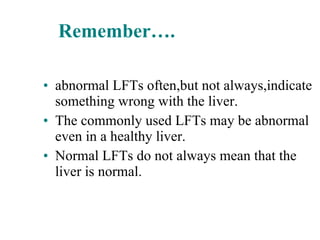
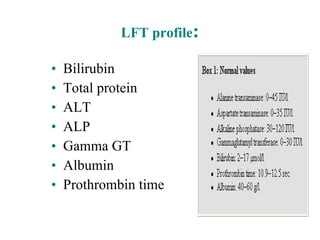
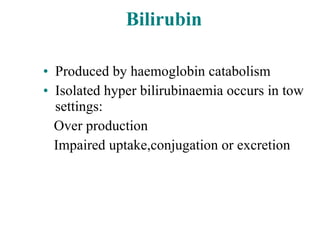
- Liver function tests (LFTs) are used to screen for and investigate liver disease, though they can be abnormal even in a healthy liver.
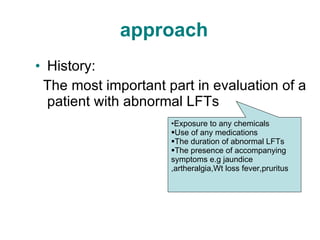
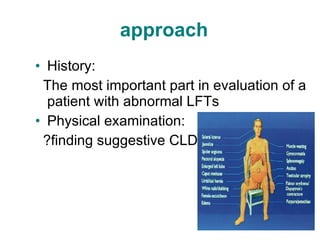
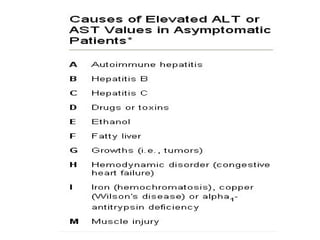
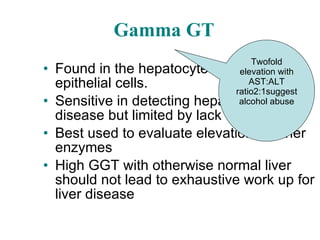
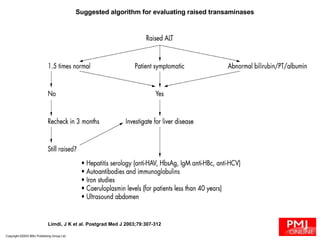
- The most important part of evaluating abnormal LFTs is obtaining a thorough medical history regarding medications, chemical exposures, and symptoms.
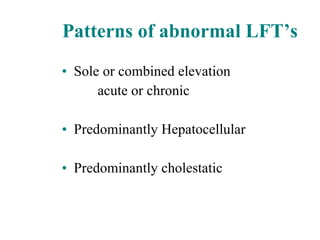
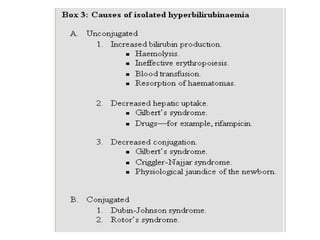
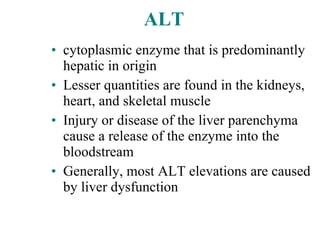
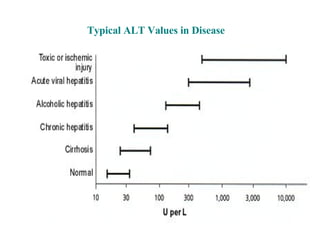
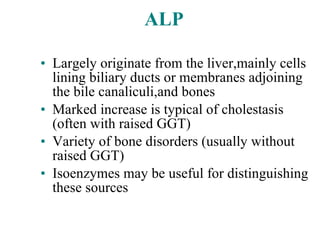
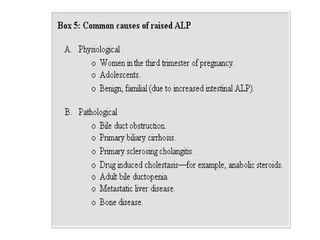
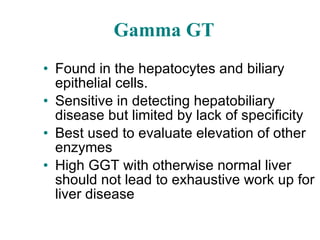
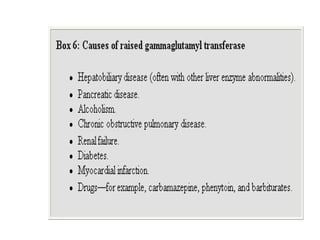
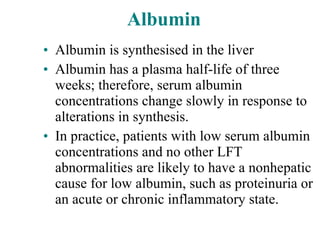
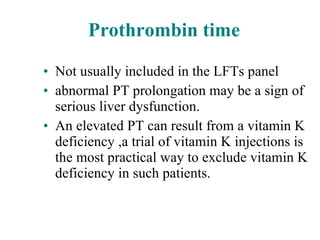
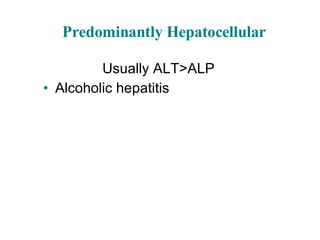
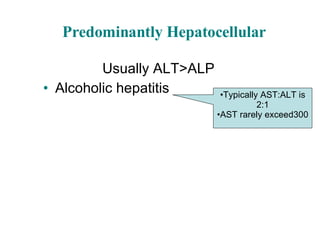
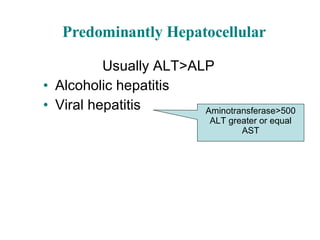
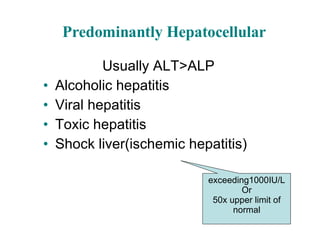
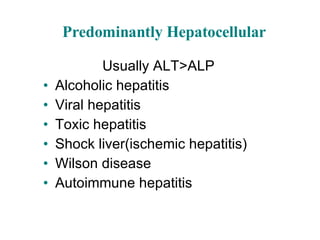
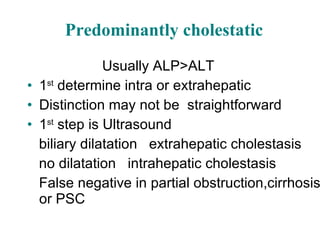
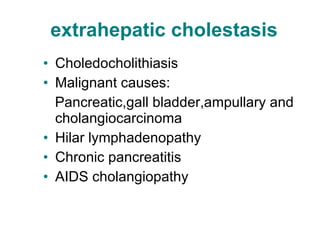
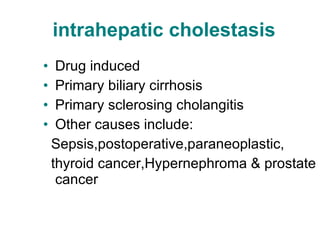
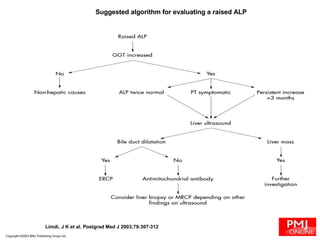
- Physical examination and additional lab tests can help determine if the abnormal LFT pattern is predominantly hepatocellular or cholestatic and suggest possible etiologies like viral hepatitis, alcohol use, or drug toxicity.
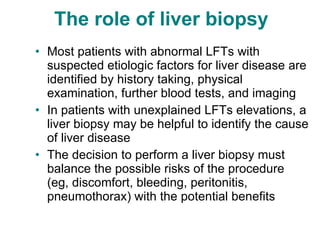
- A liver biopsy may be necessary when the cause of abnormal LFTs remains unexplained after history, exams and other testing to identify the underlying liver disease.