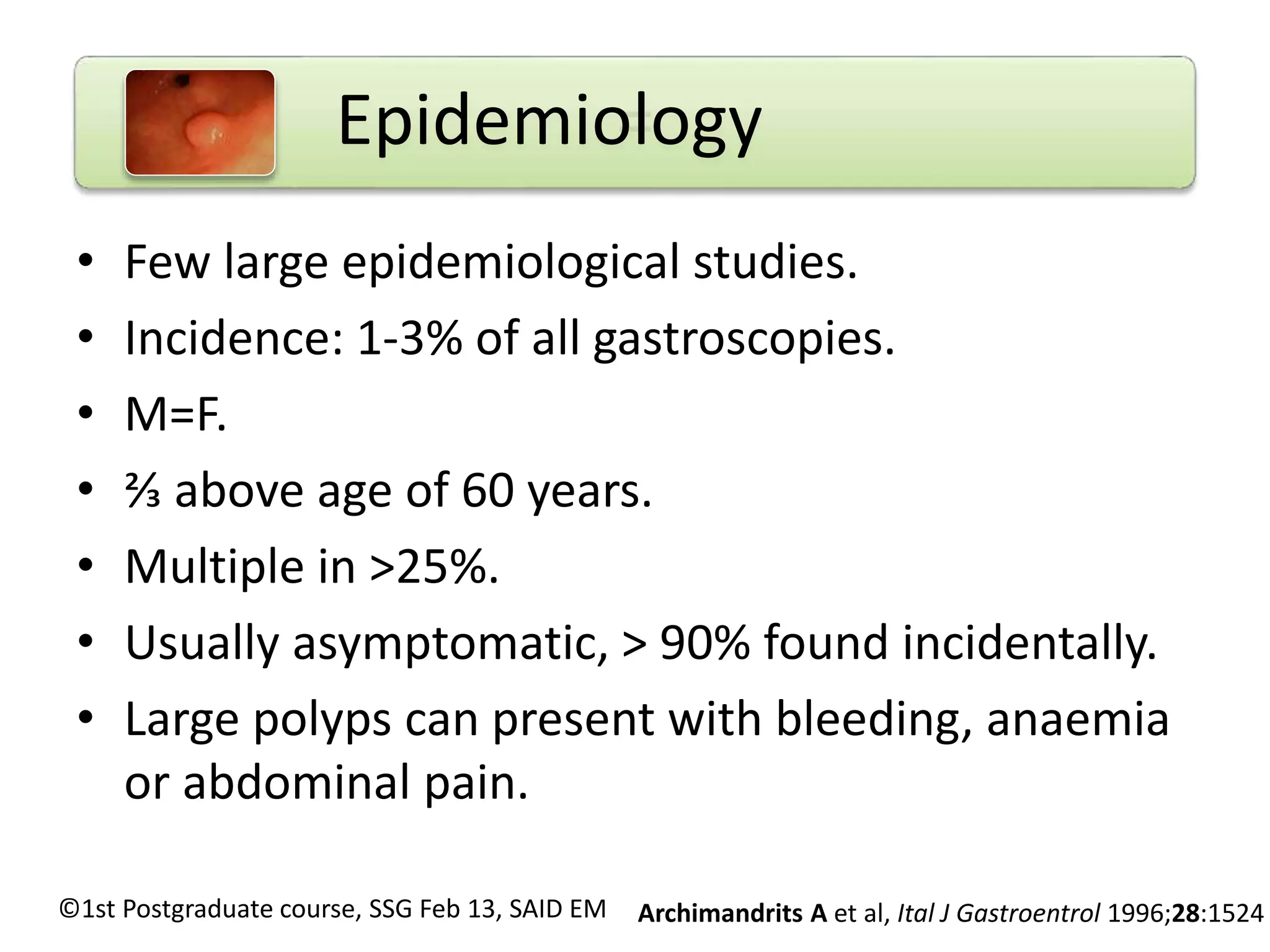
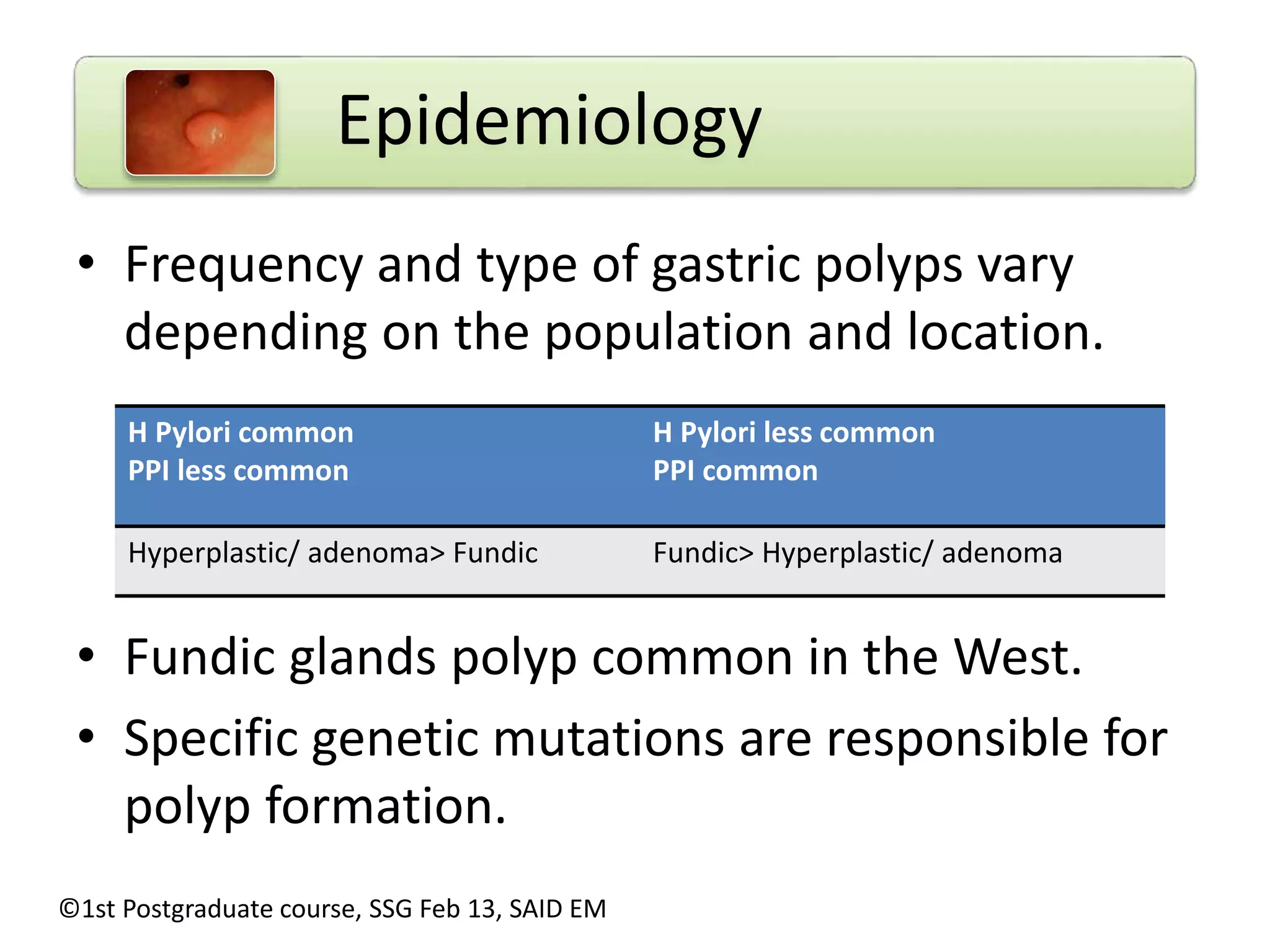
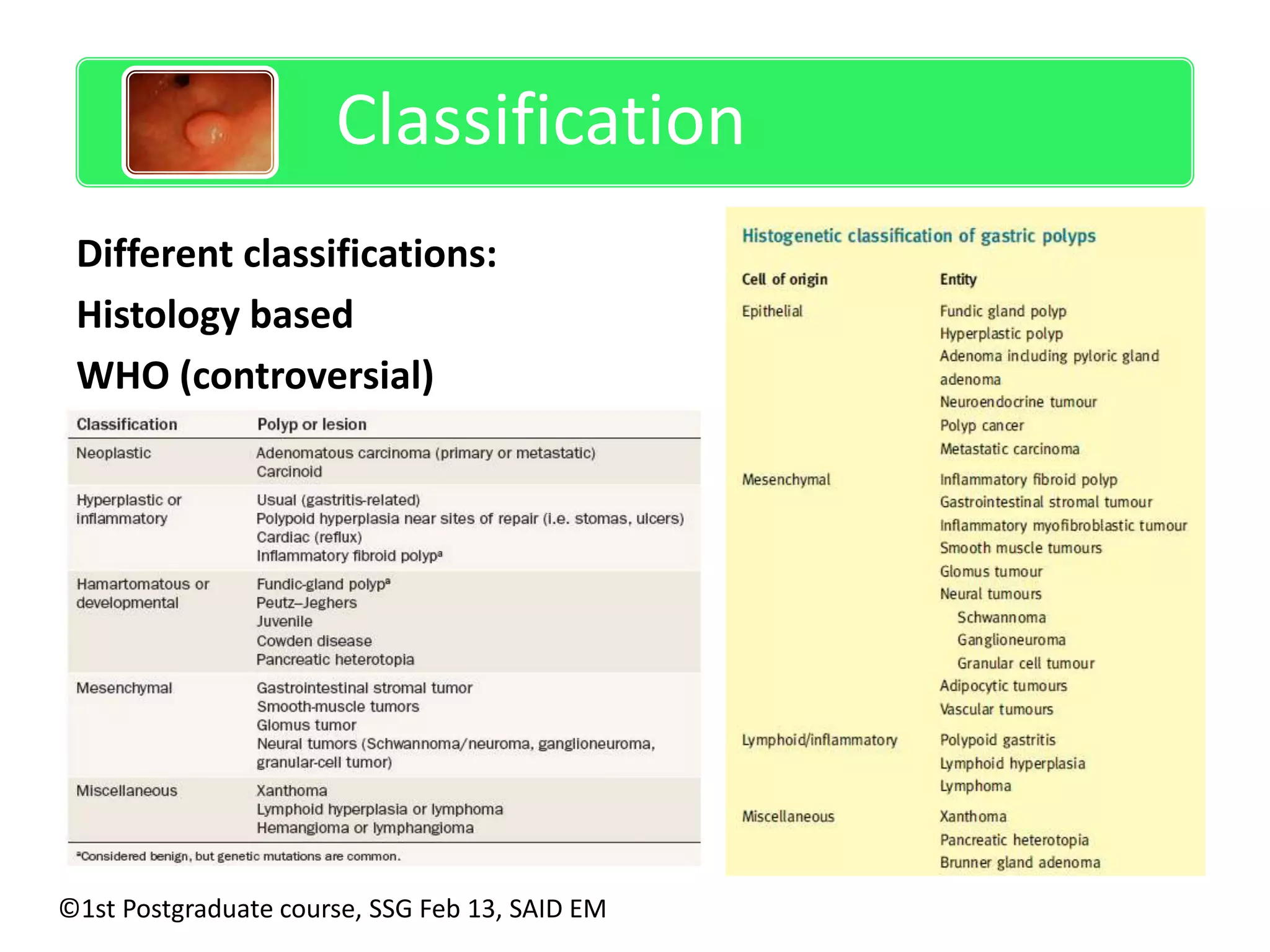
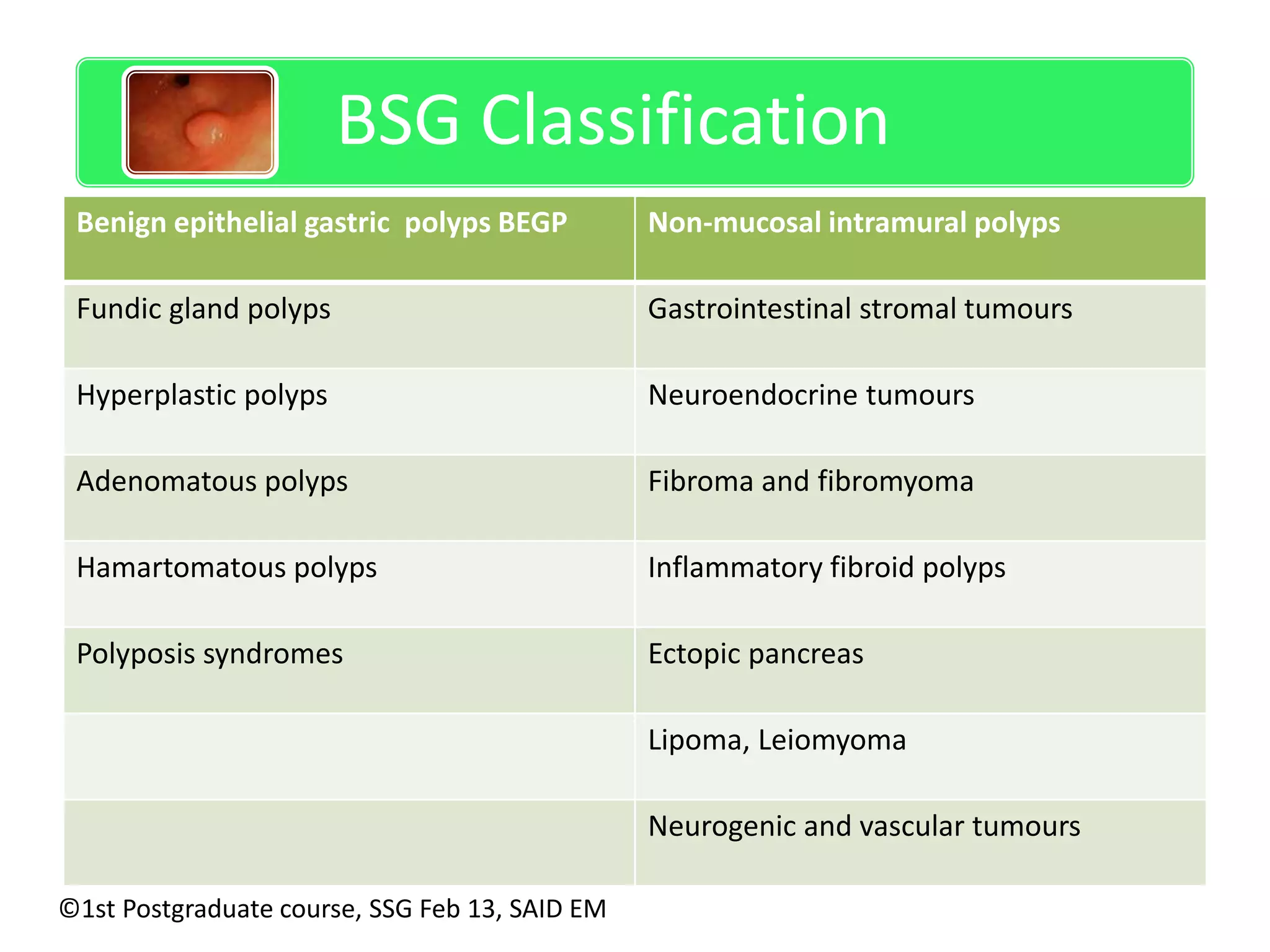
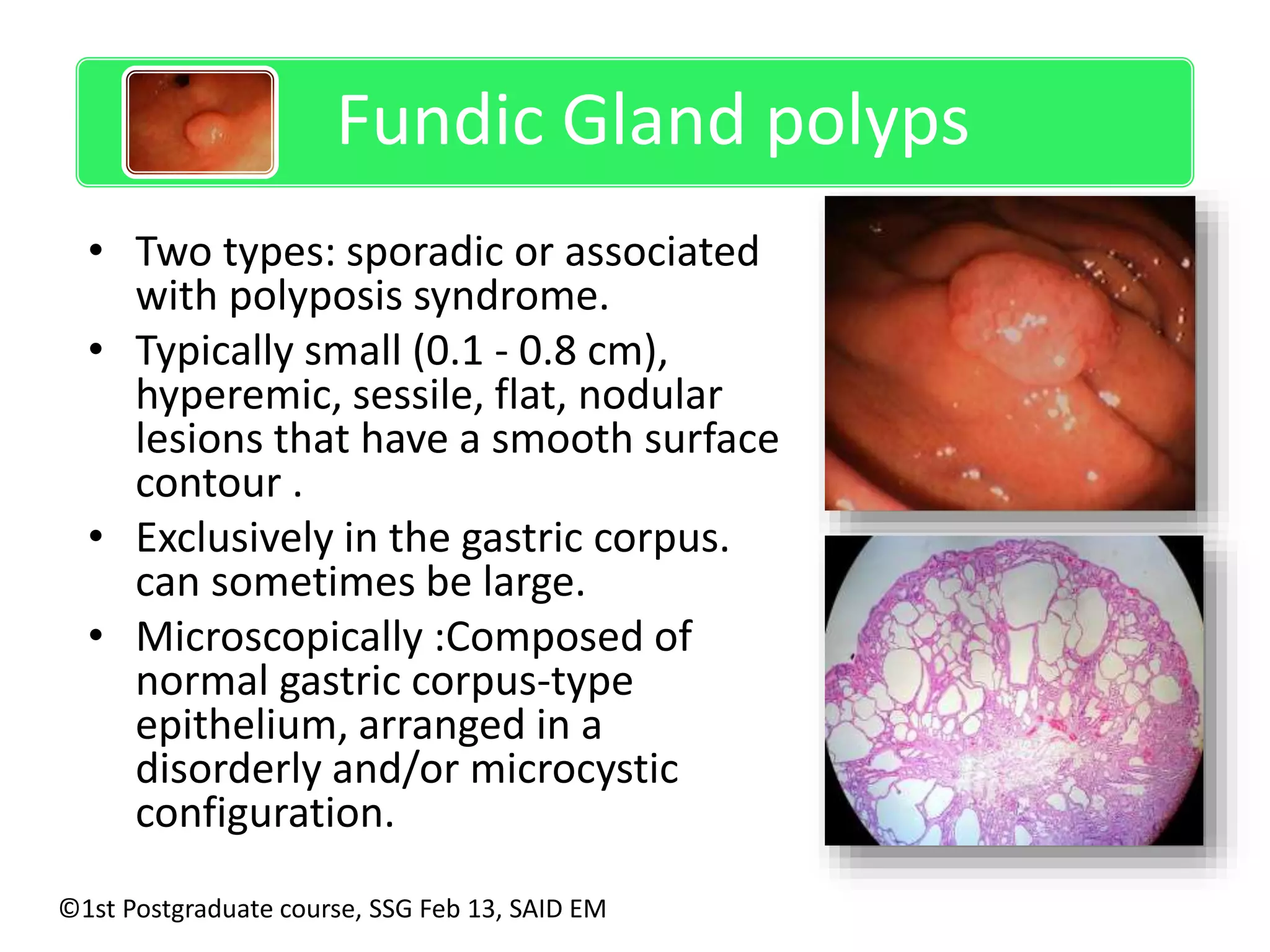
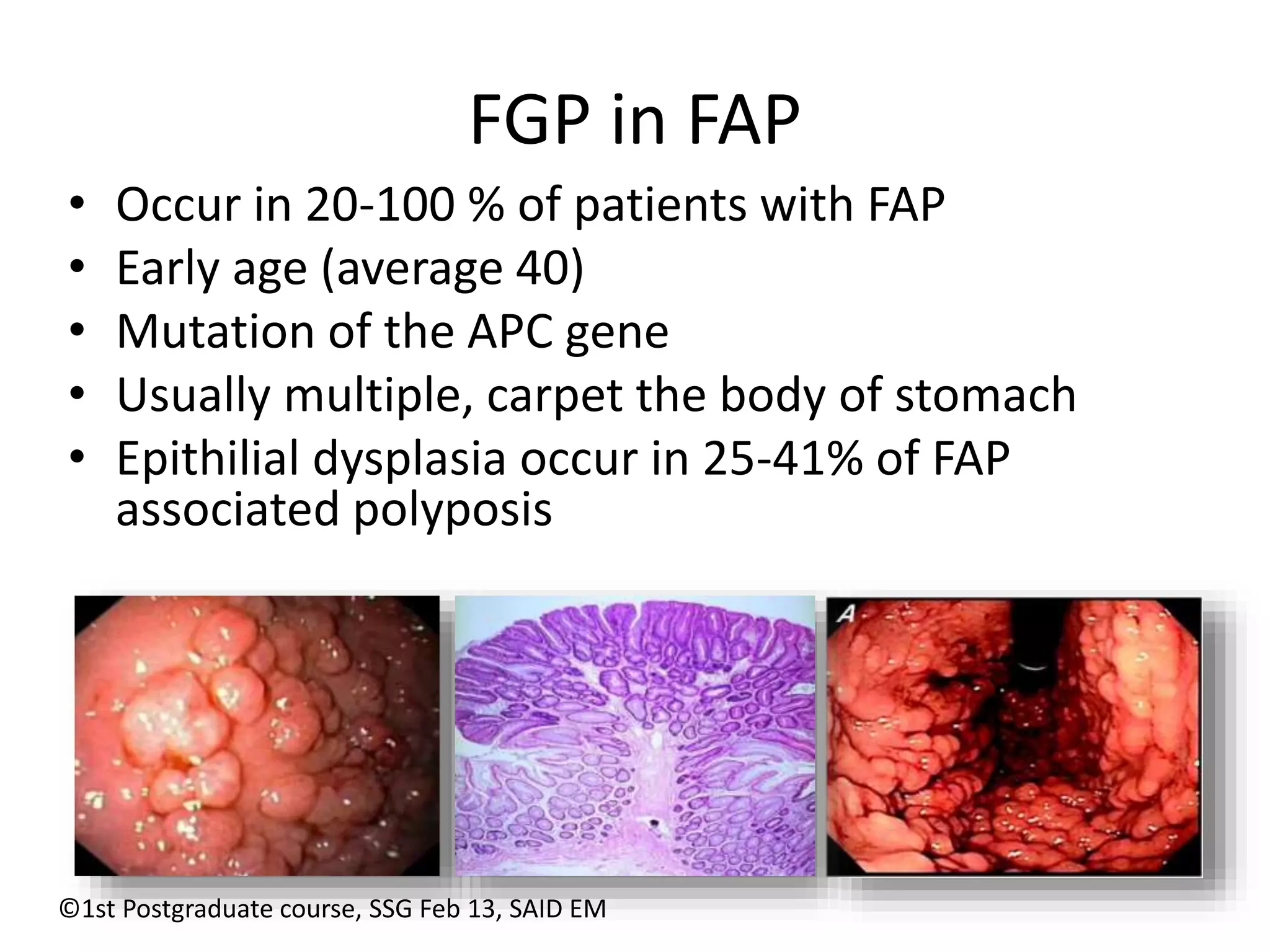
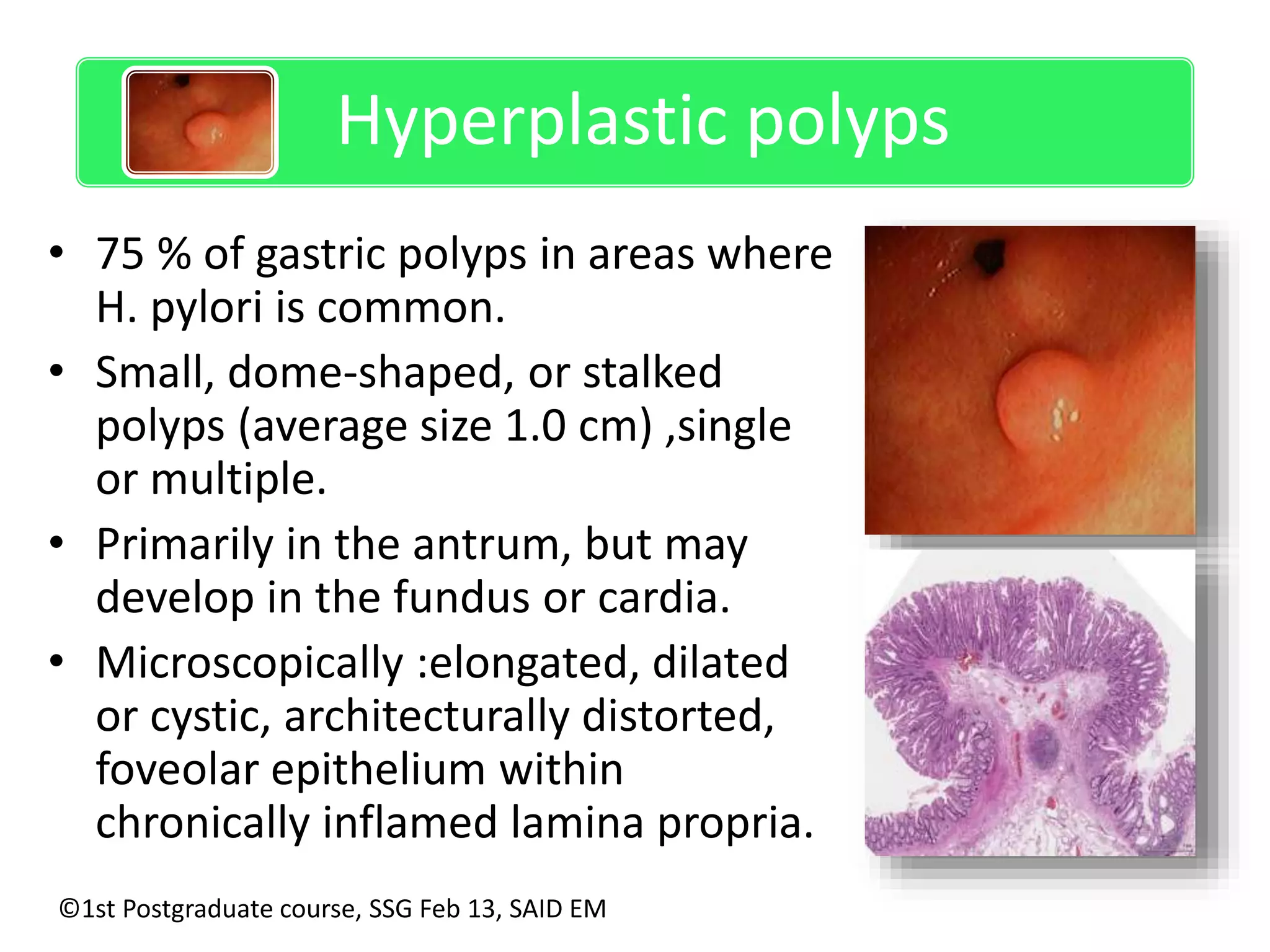
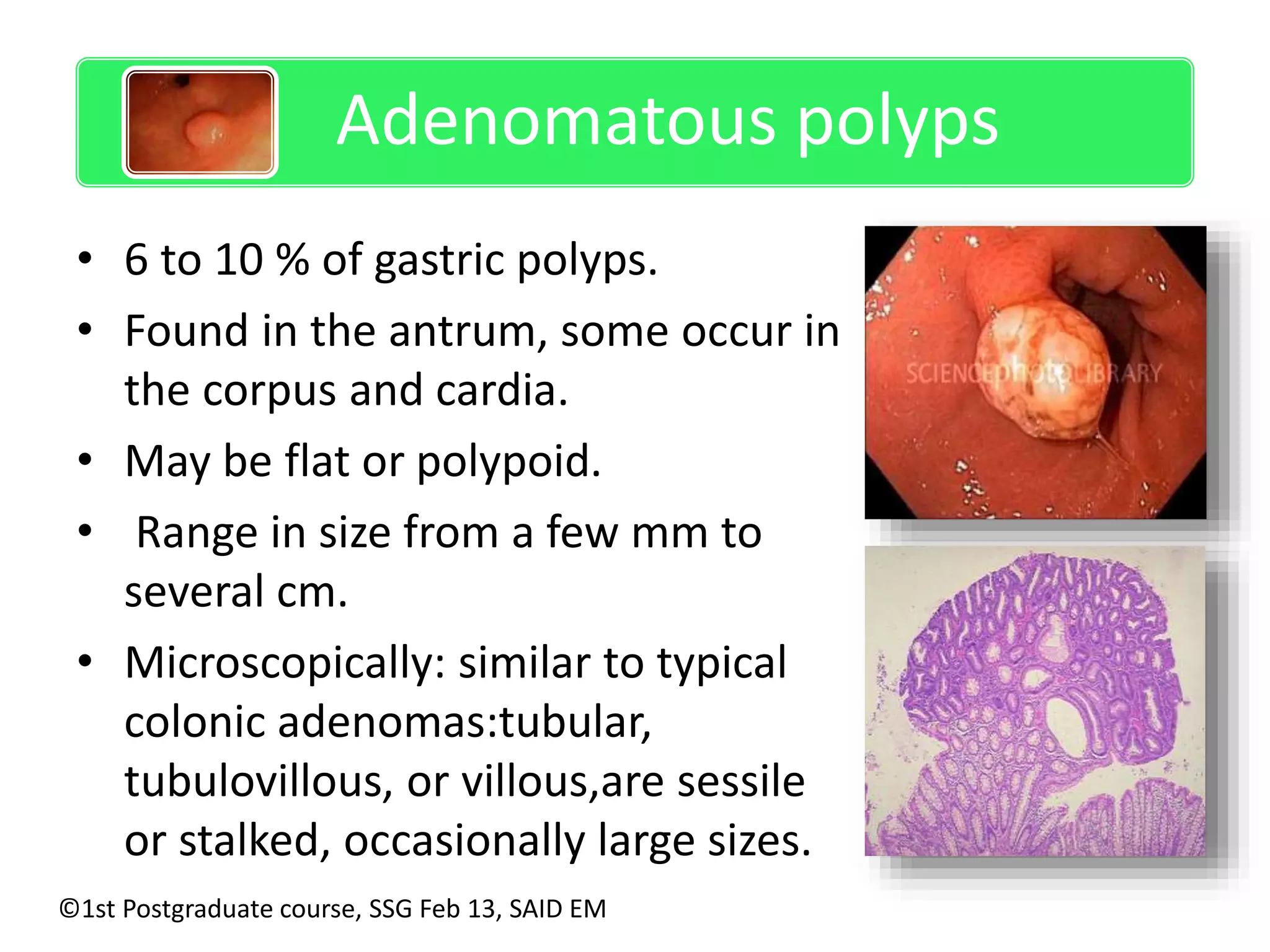
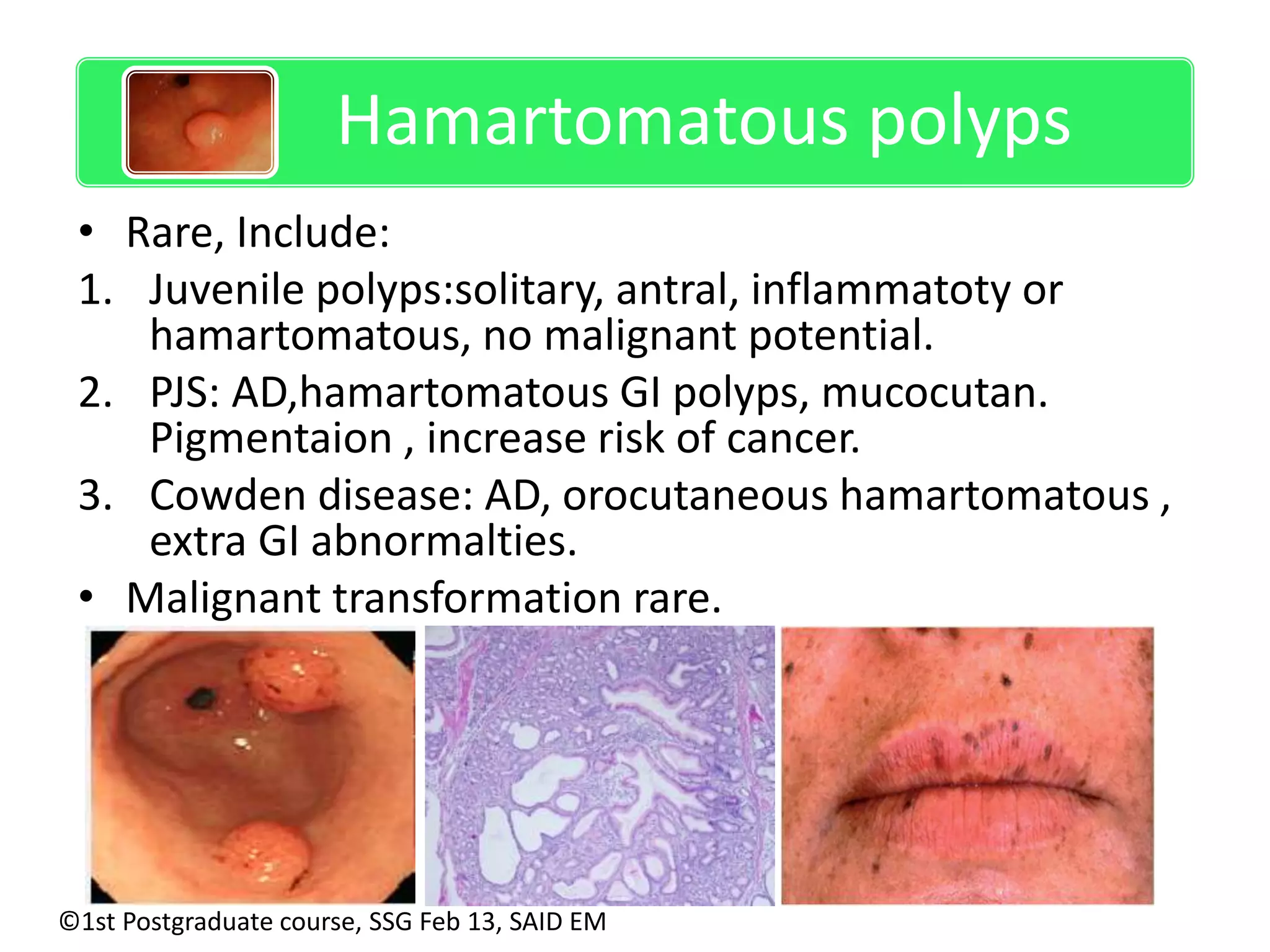
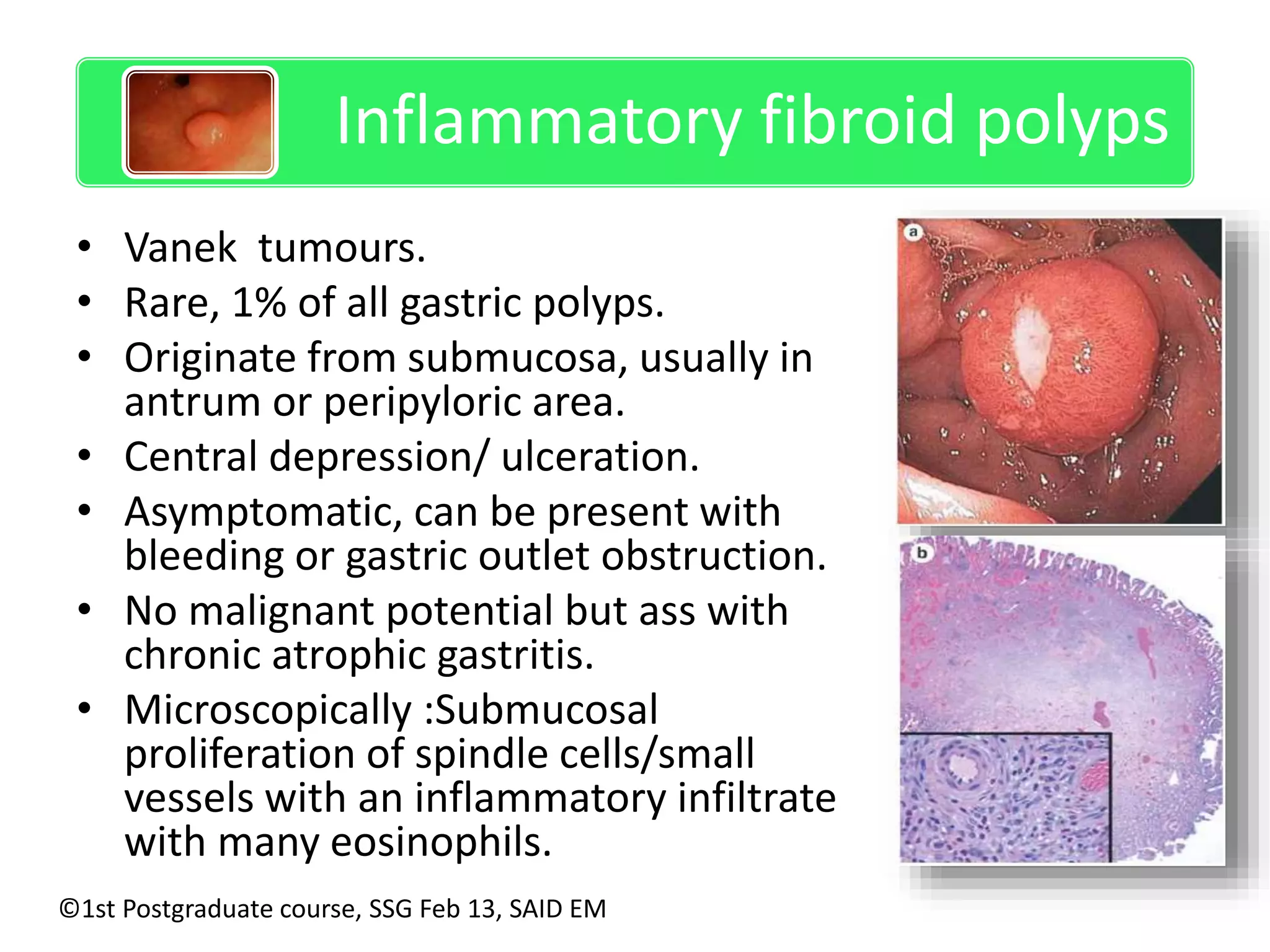
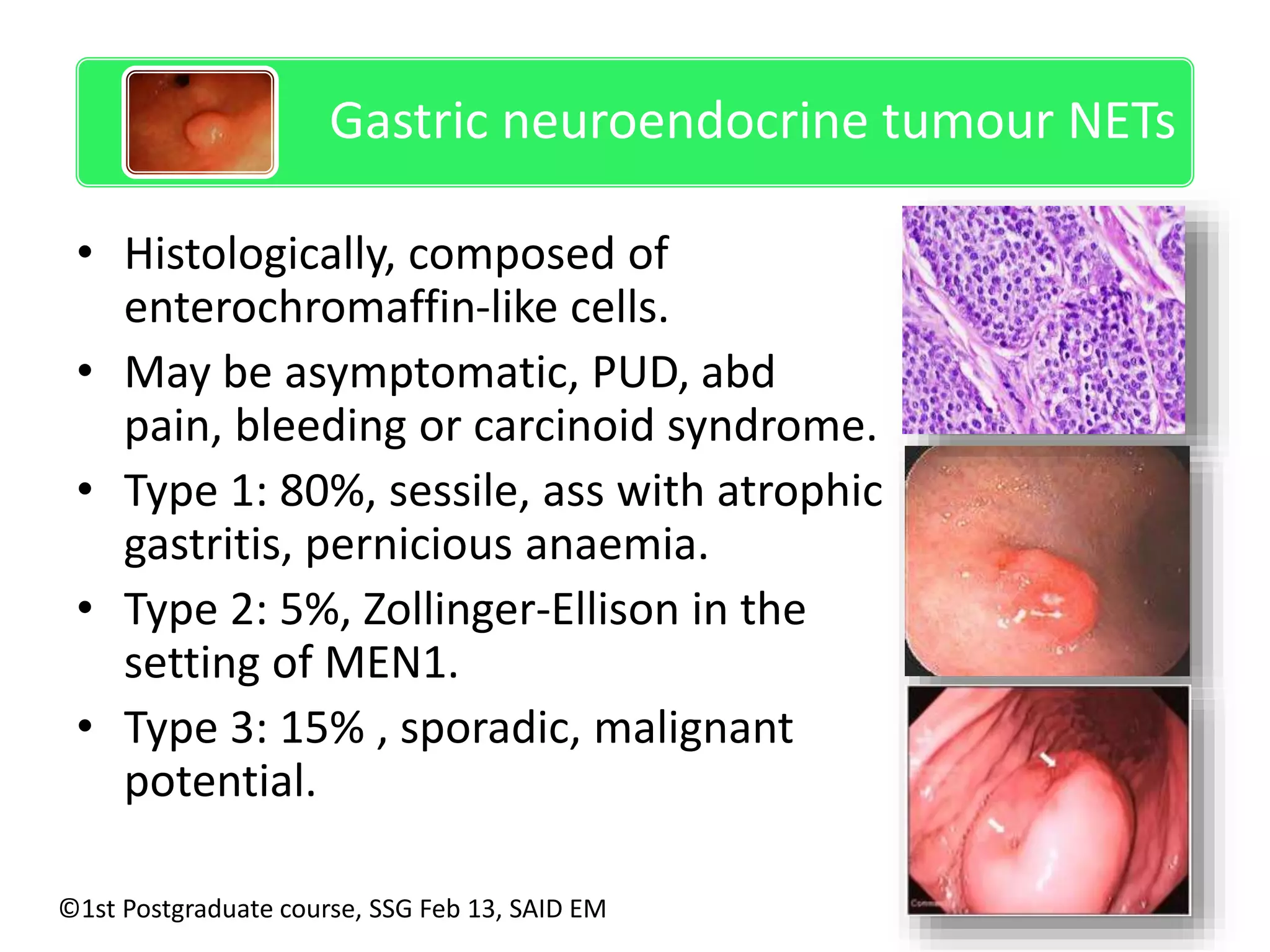
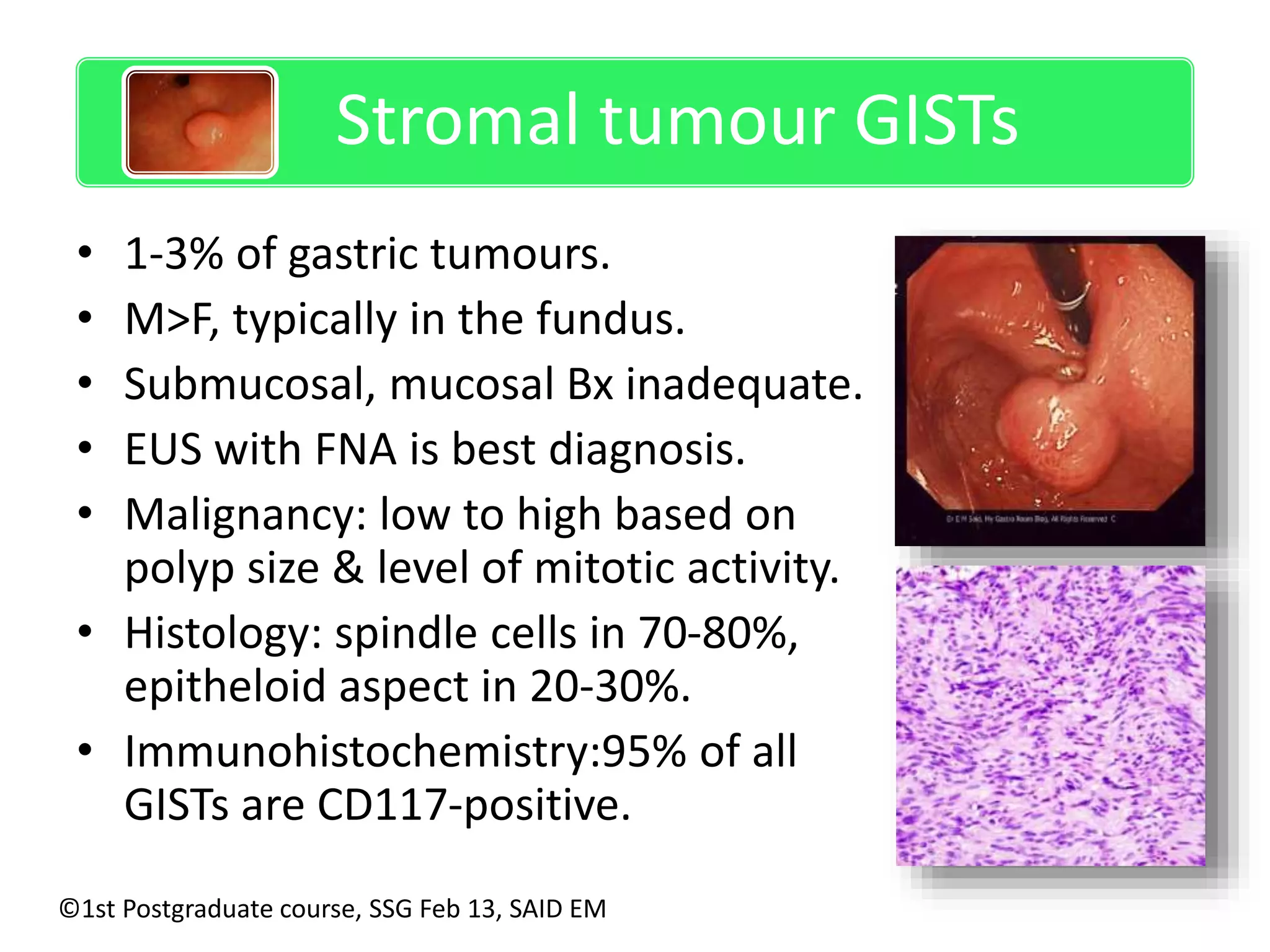
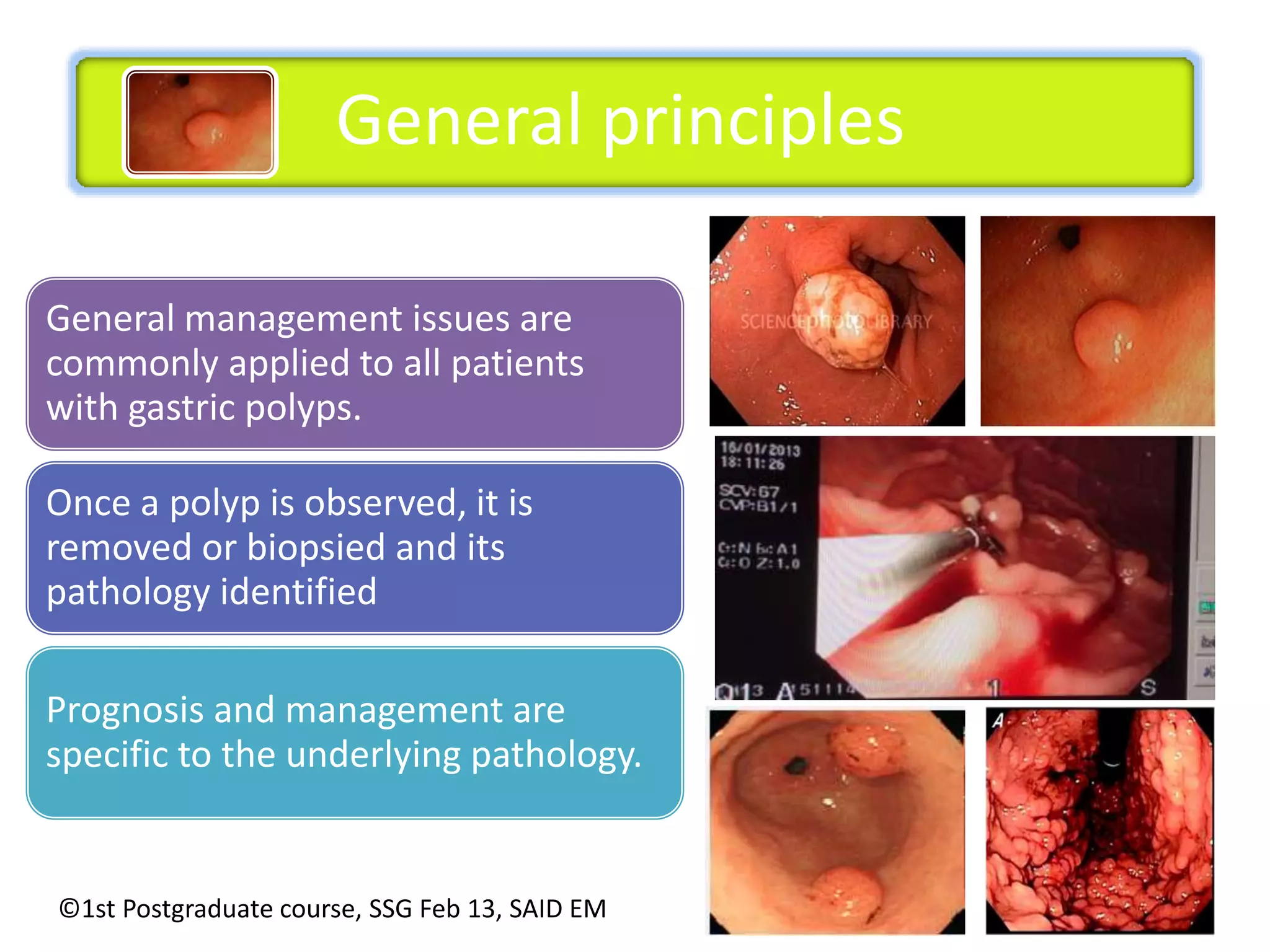
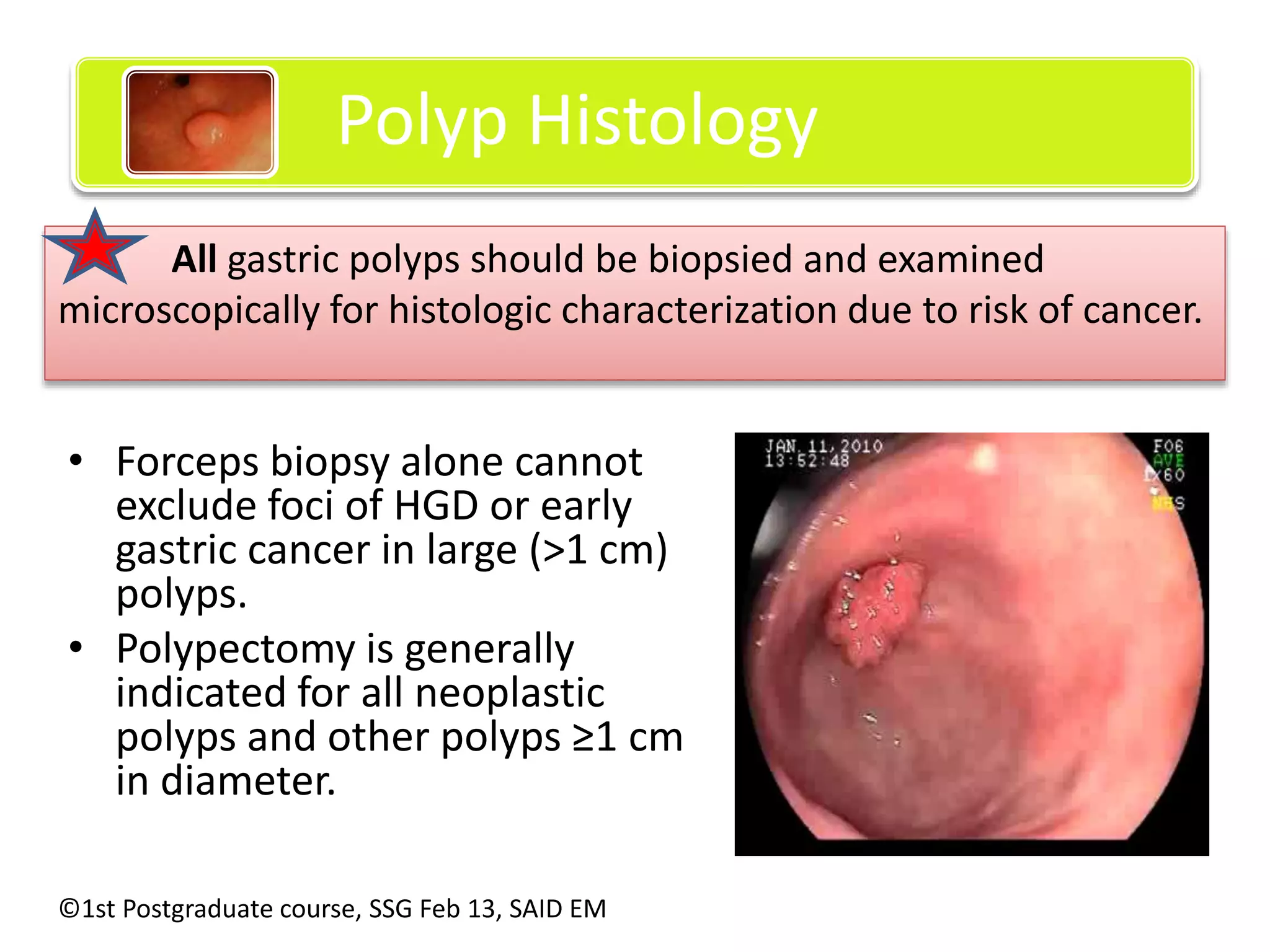
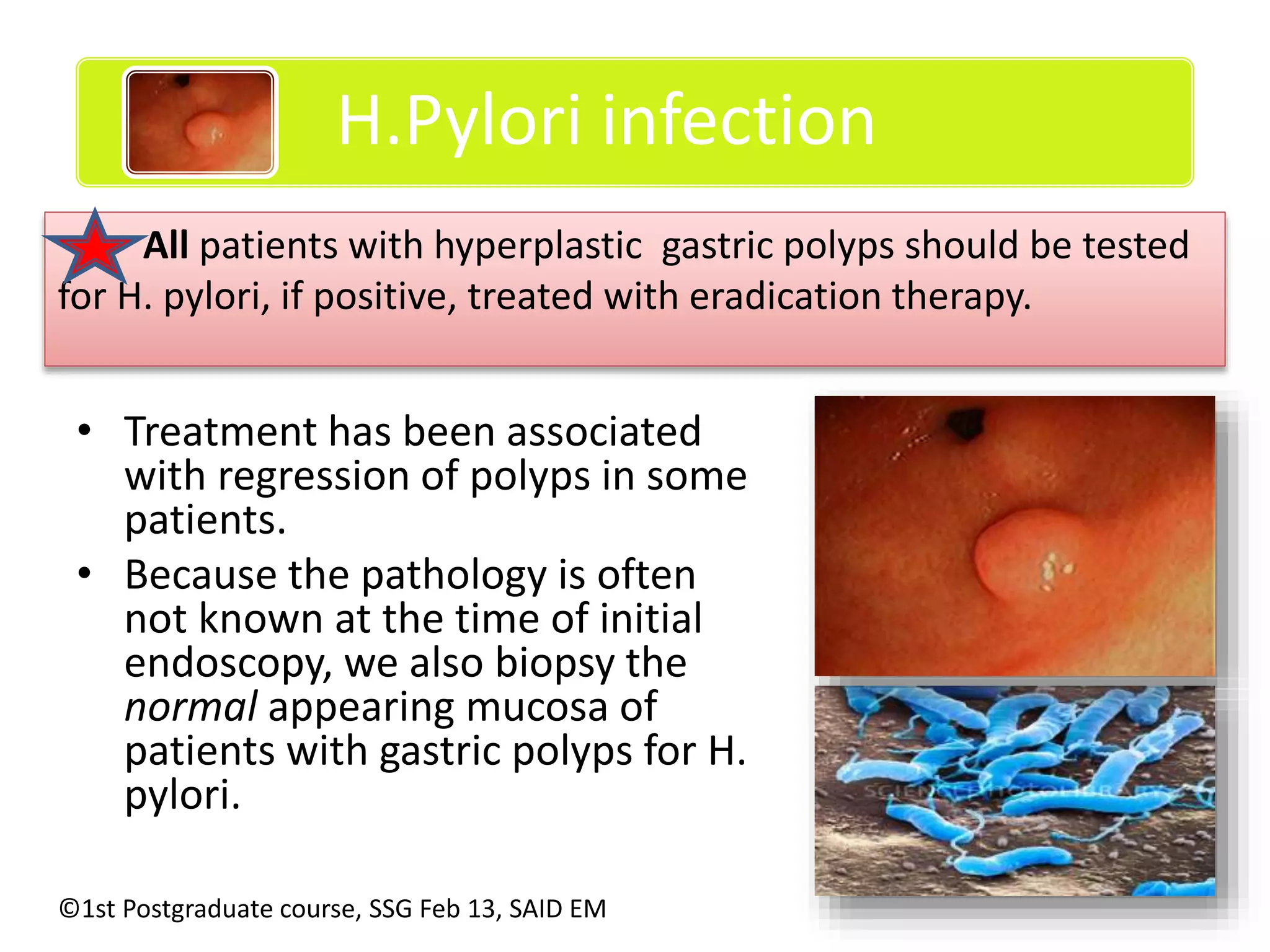
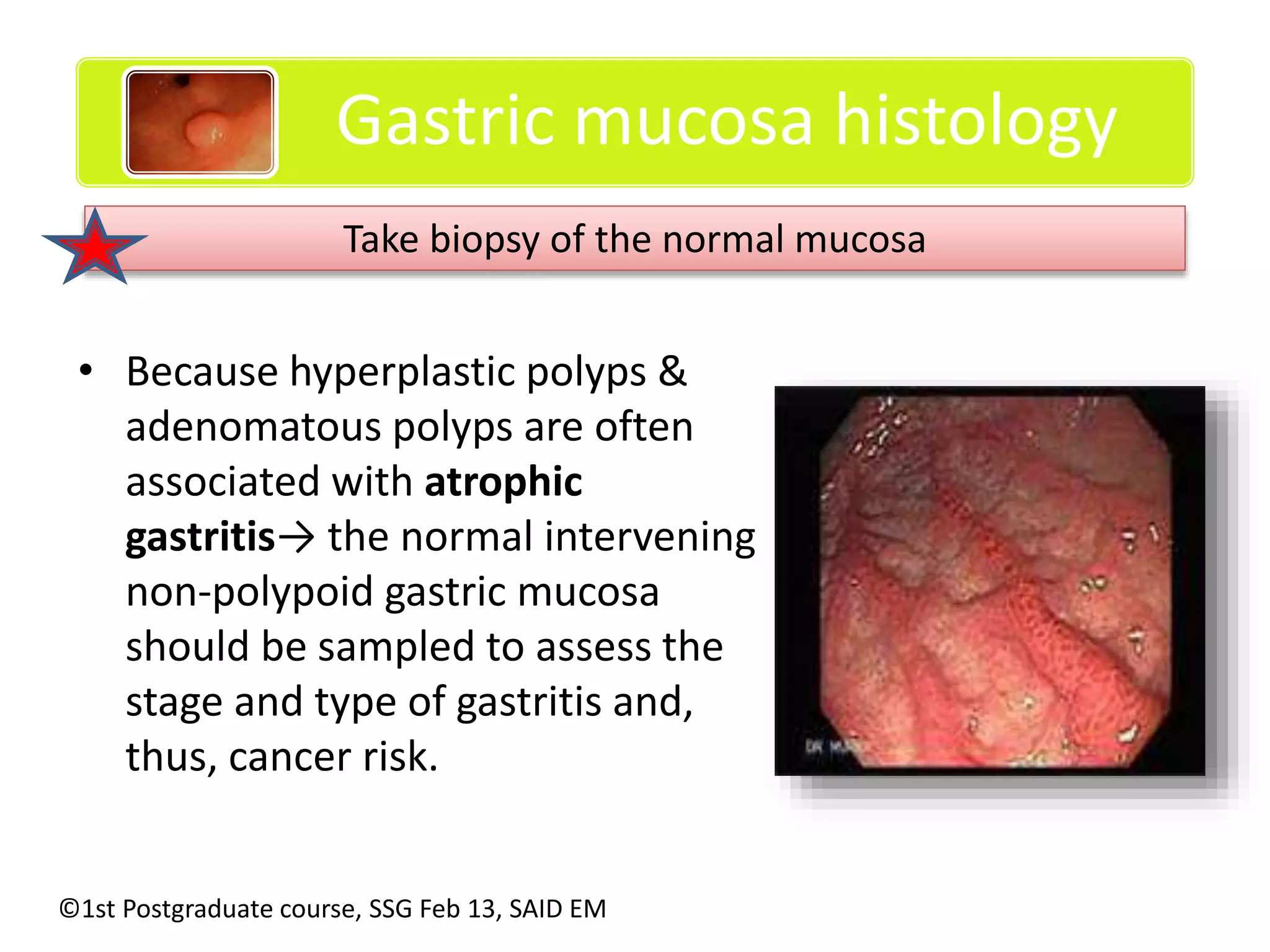
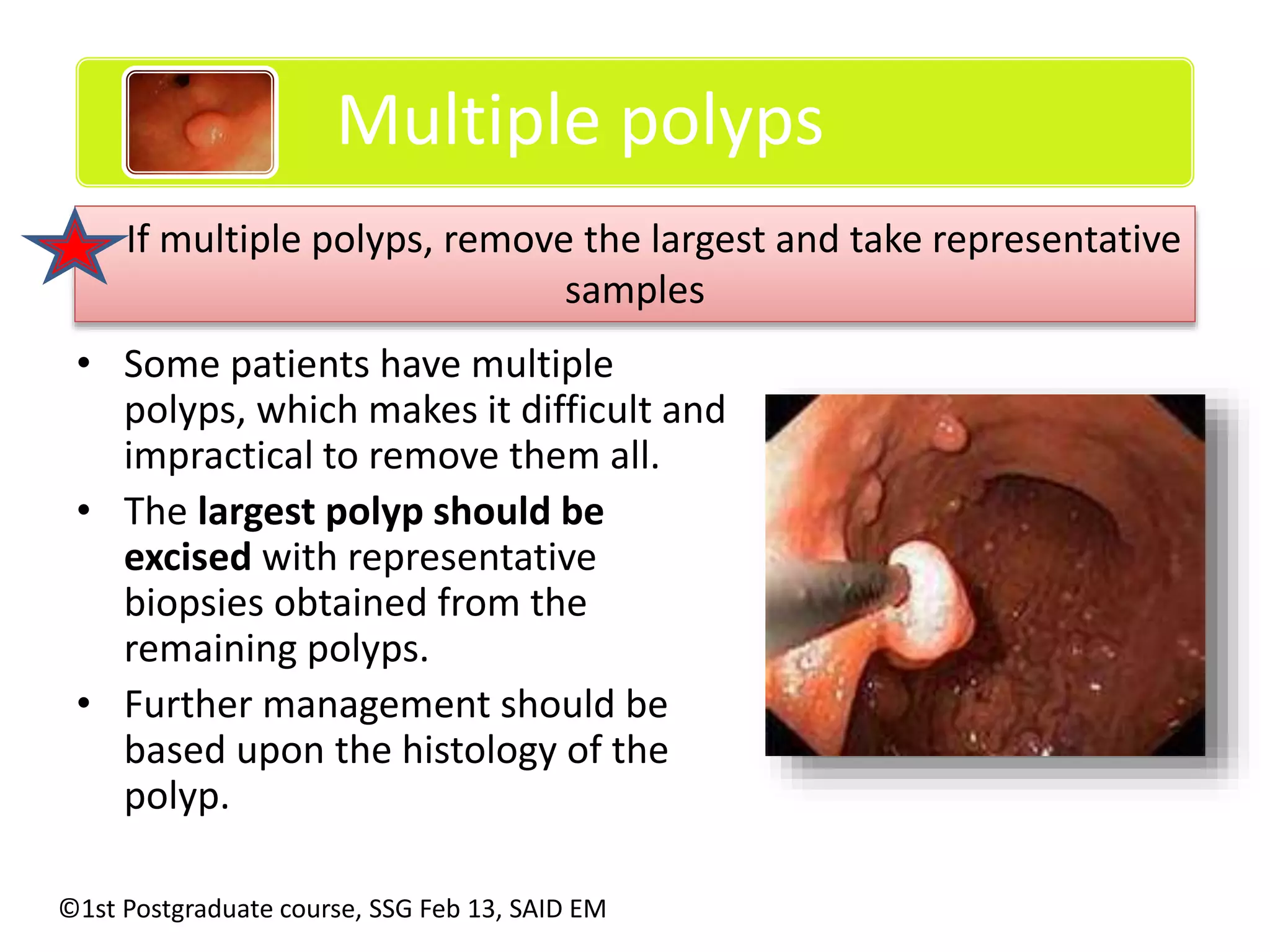
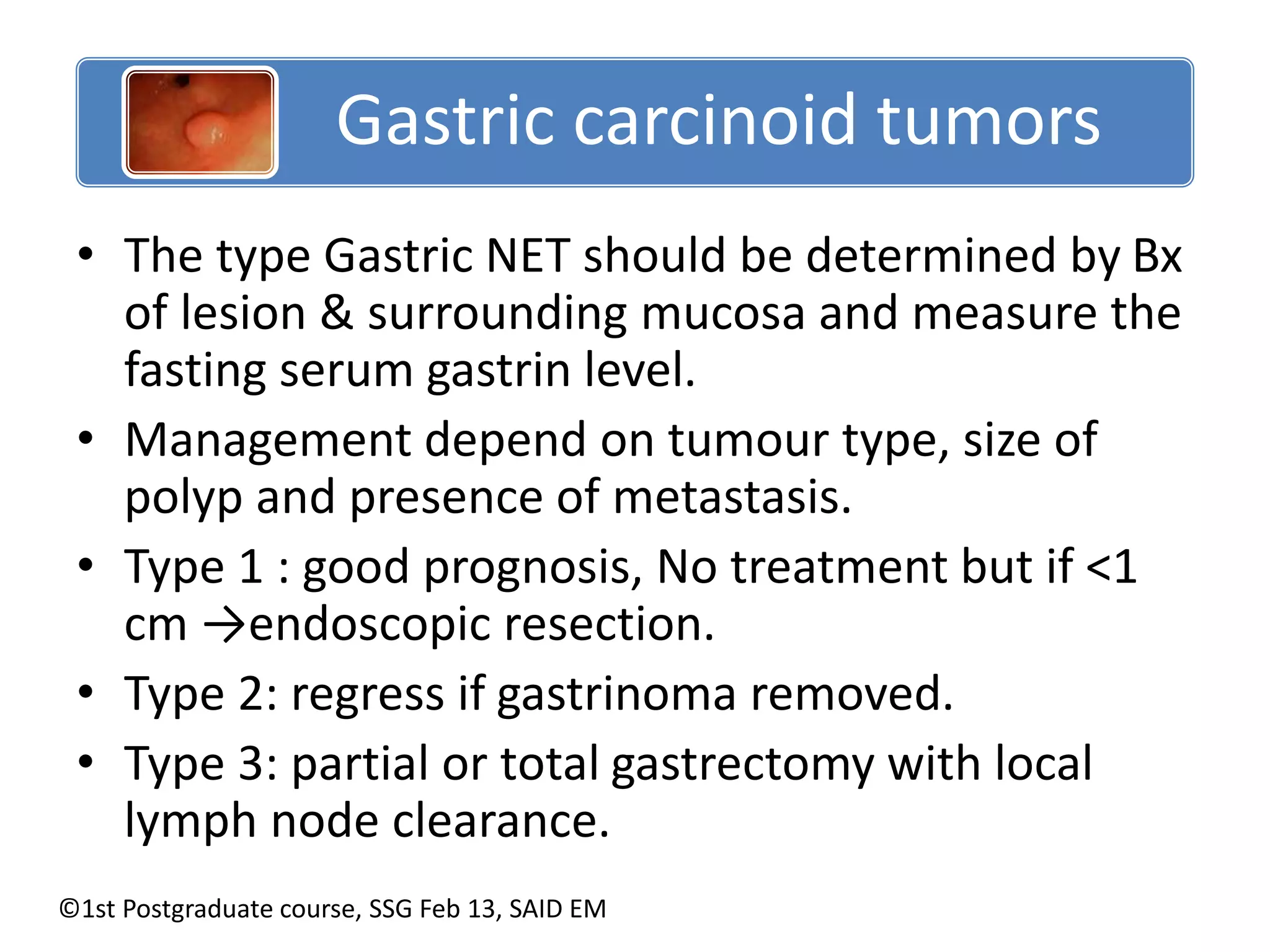
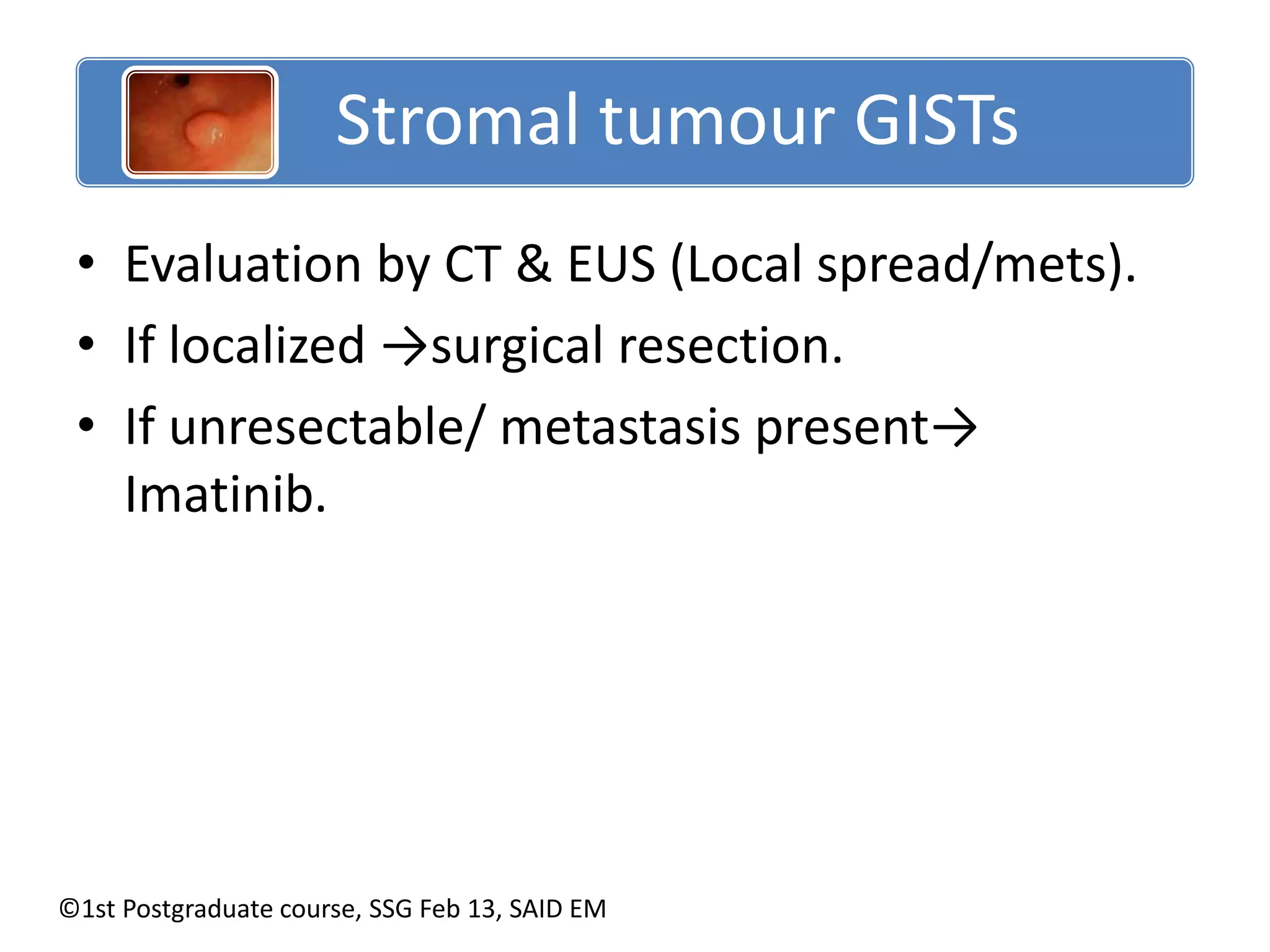
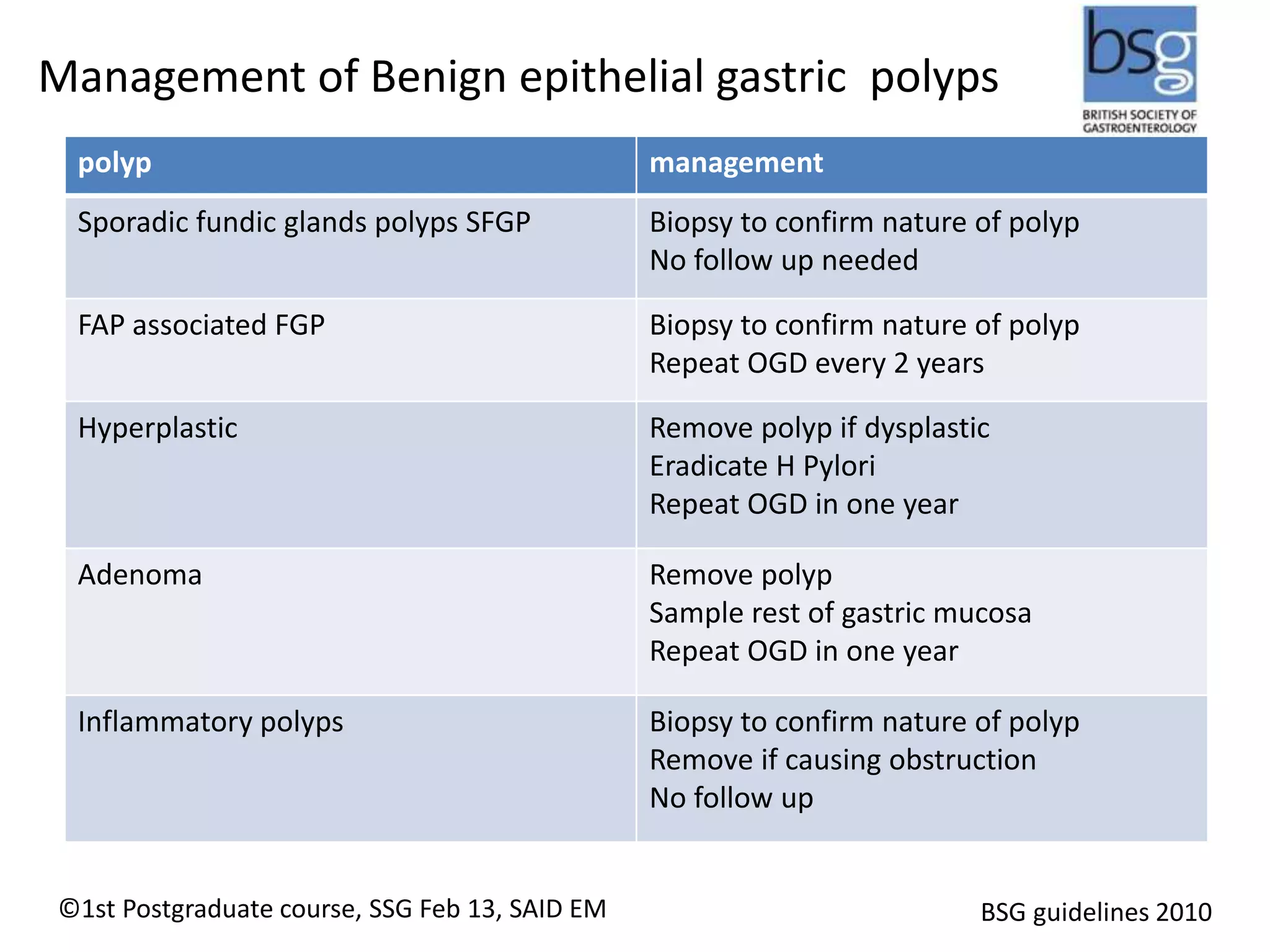
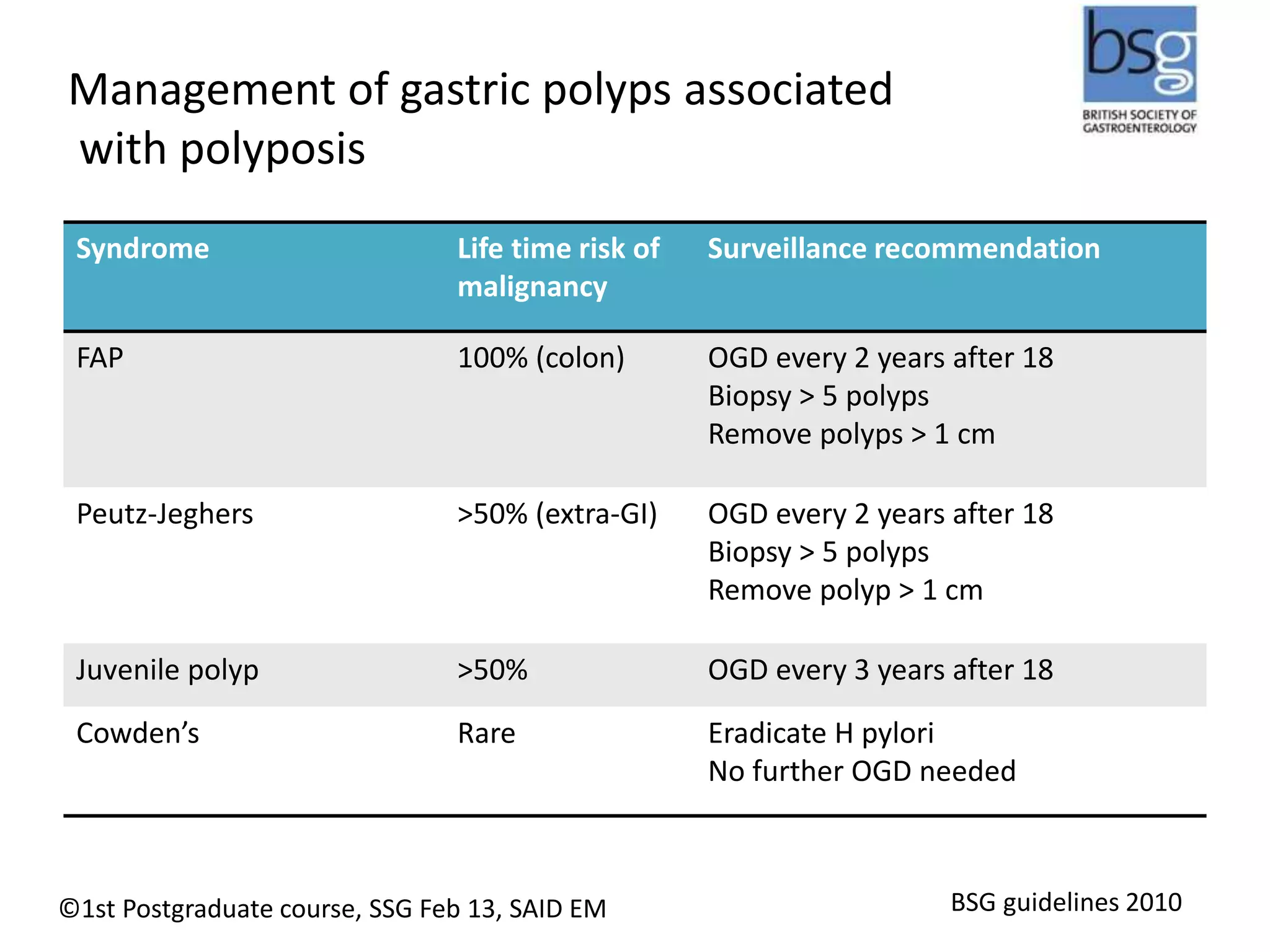
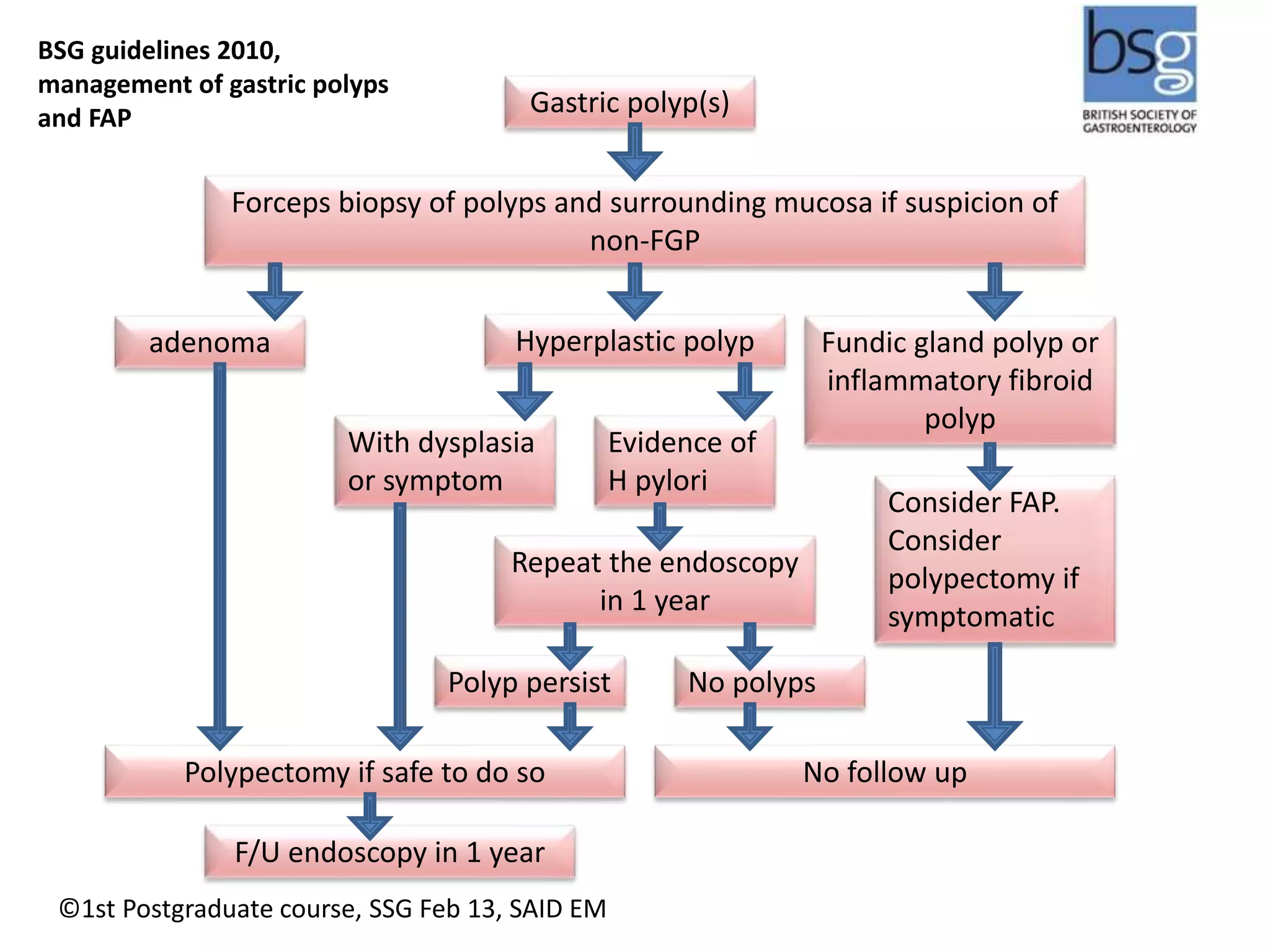
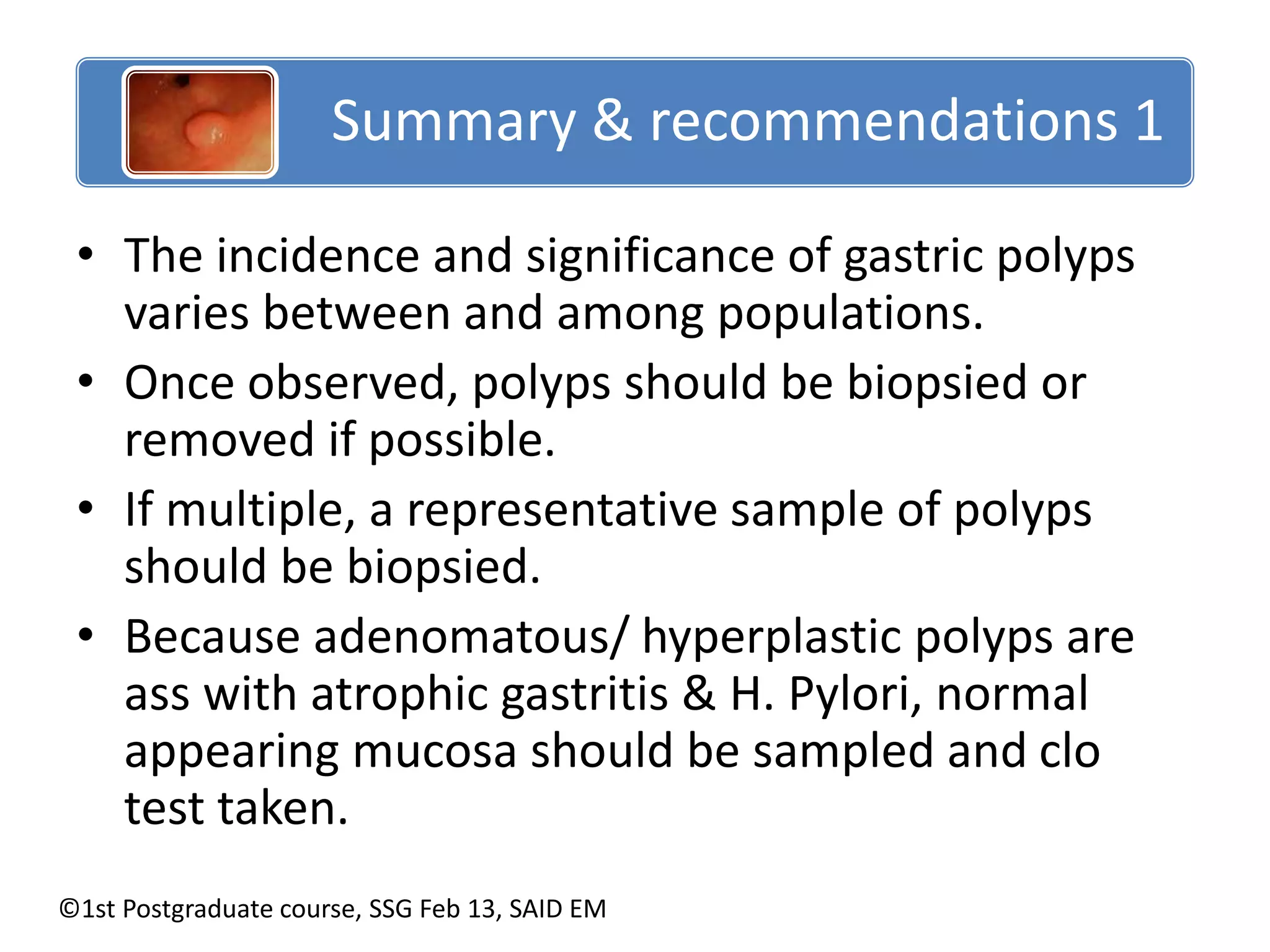
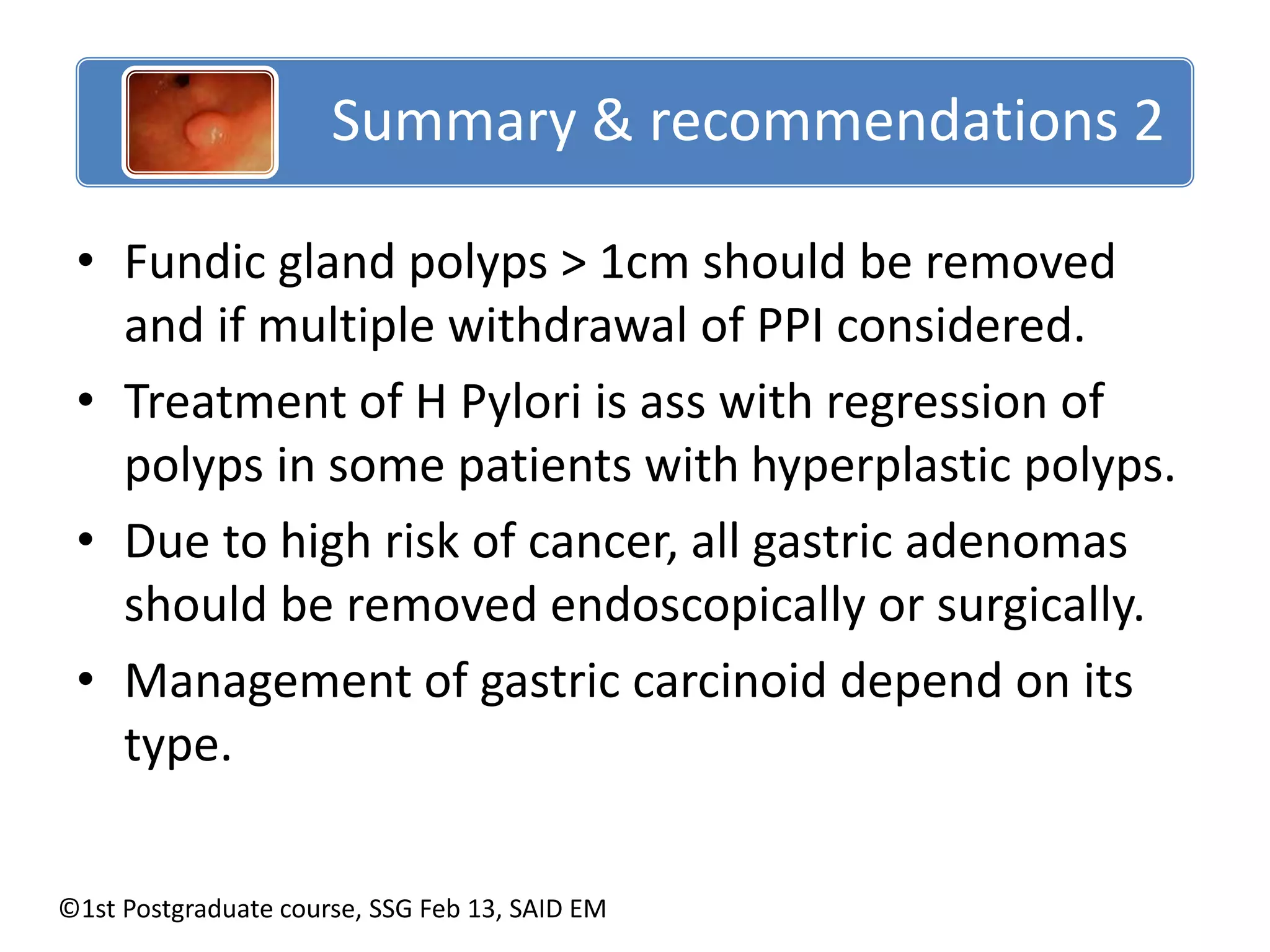
This document discusses the management of gastric polyps. It begins with an introduction to gastric polyps and their classification. It then discusses the epidemiology and histological classification of various polyp subtypes. General management principles are outlined, including biopsying polyps, checking for H. pylori infection, and surveillance based on polyp type and characteristics. Specific guidelines are provided for managing common polyp types such as hyperplastic, fundic gland, adenomatous and carcinoid polyps. The document concludes with recommendations that gastric polyps should be fully characterized, the stomach evaluated for atrophy or H. pylori, and management individualized based on polyp features and histology.