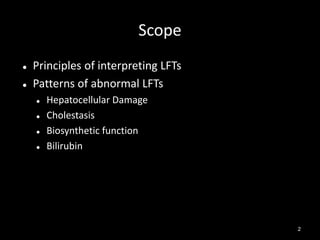
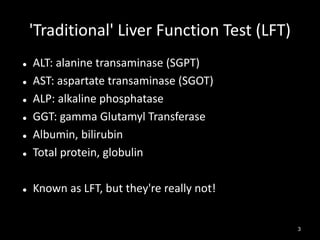
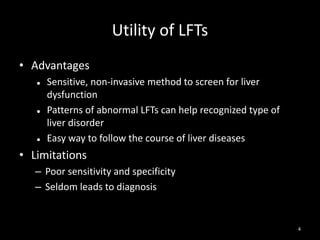
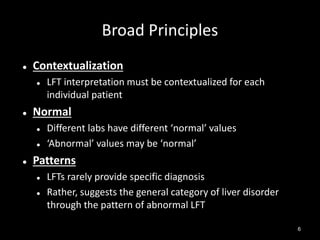
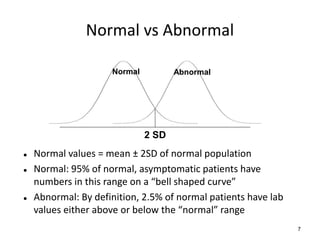
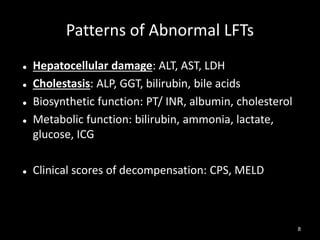
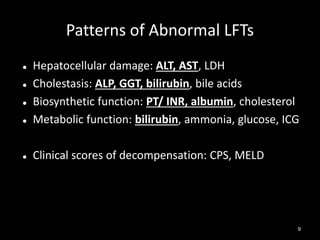
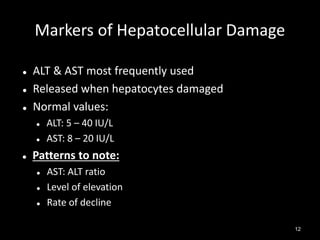
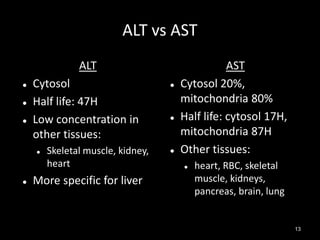
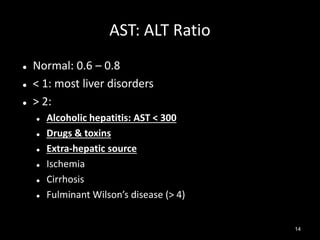
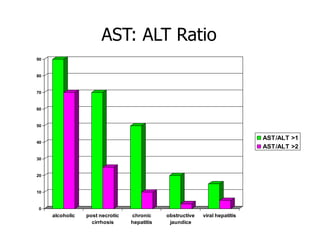
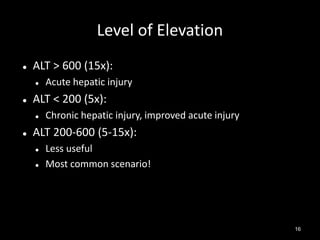
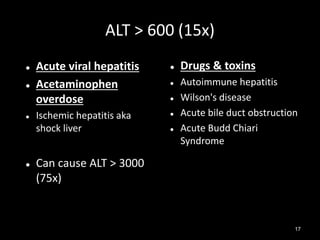
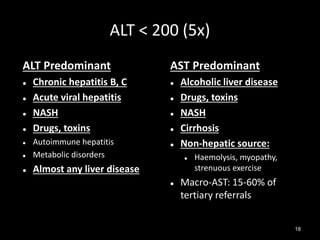
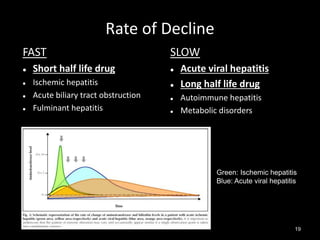
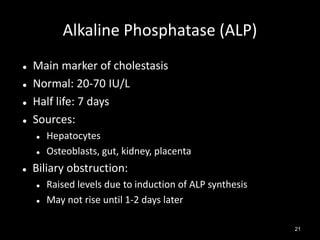
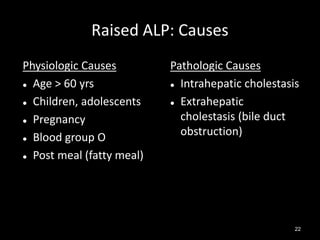
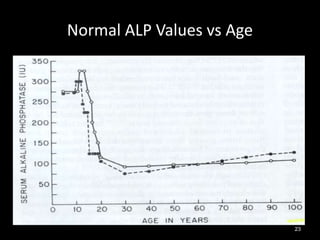
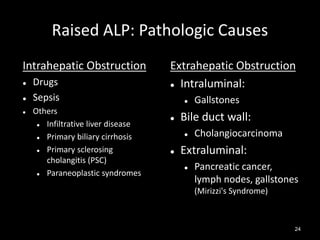
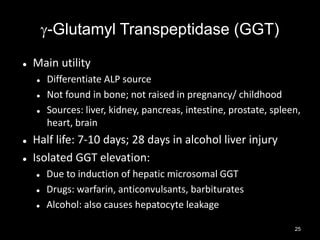
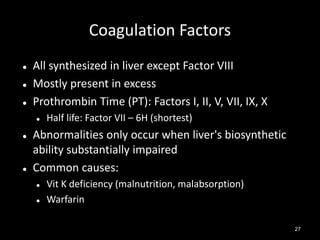
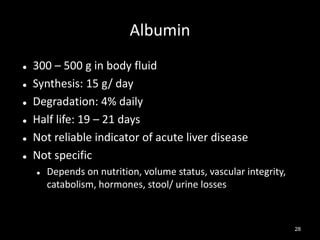
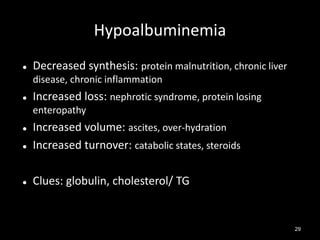
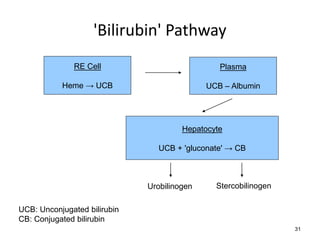
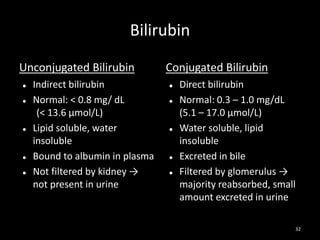
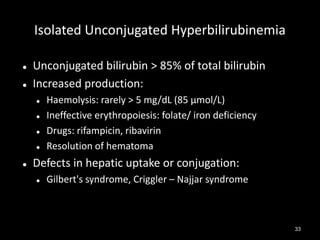
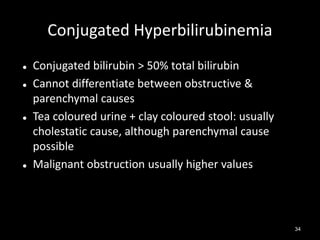
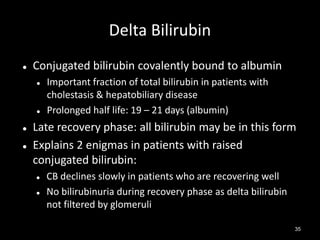
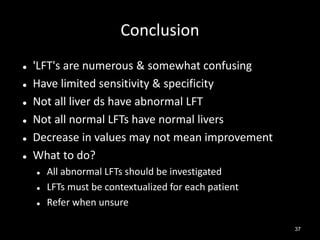
The document discusses liver function tests (LFTs), emphasizing their principles, types of abnormalities, and interpretation. It outlines key markers for hepatocellular damage, cholestasis, and biosynthetic function, as well as the importance of contextualizing test results for individual patients. Additionally, it highlights the limitations of LFTs in diagnosing liver diseases, recommending further investigation when abnormalities are detected.