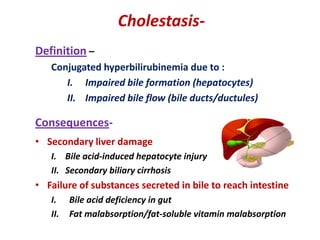
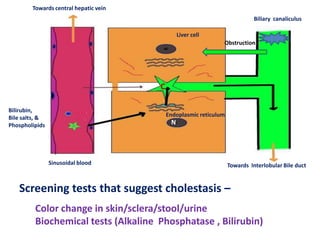
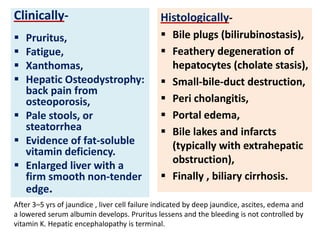
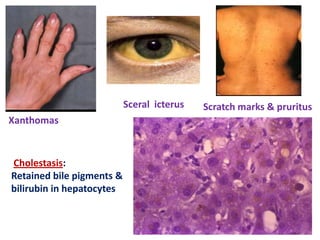
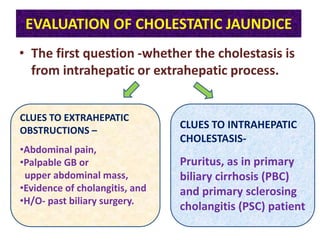
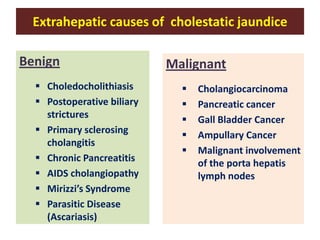
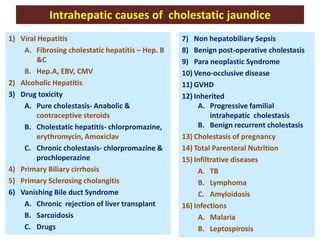
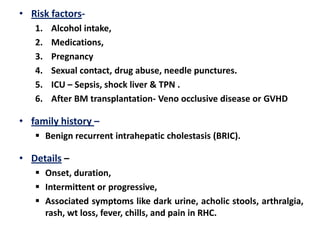
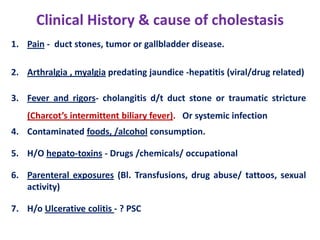
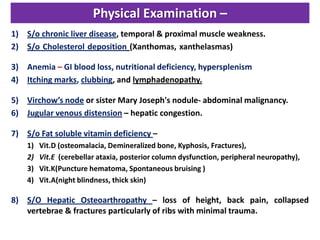
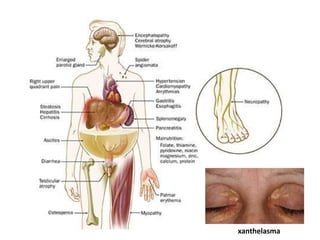
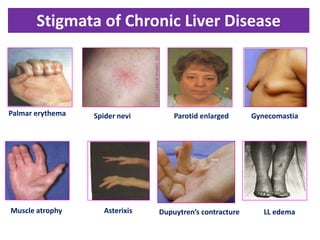
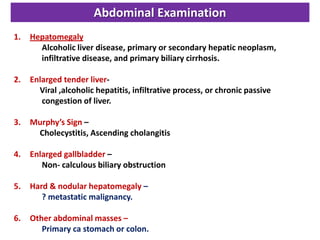
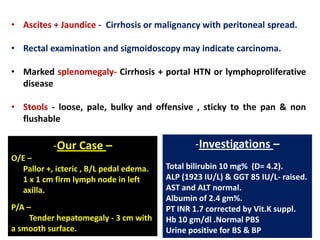
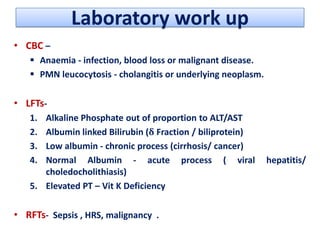
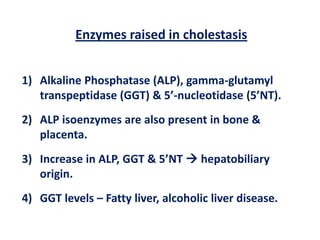
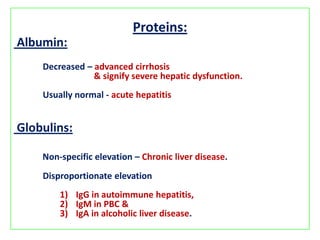
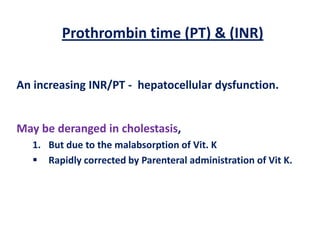
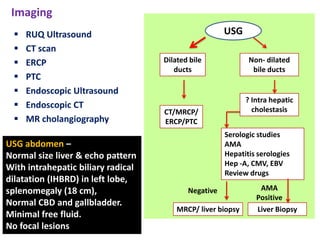
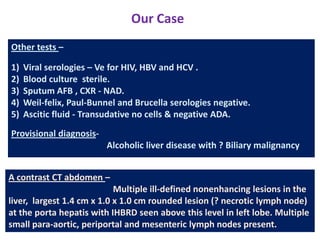
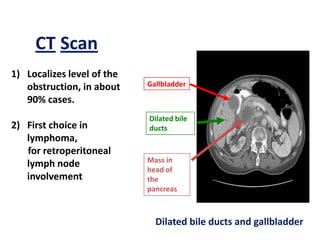
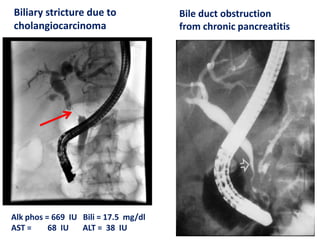
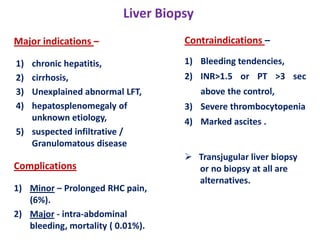
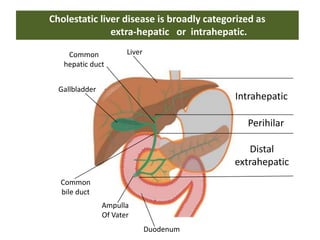
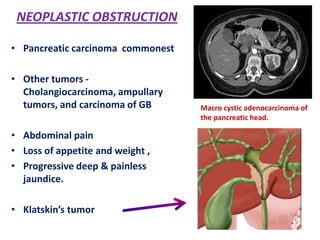
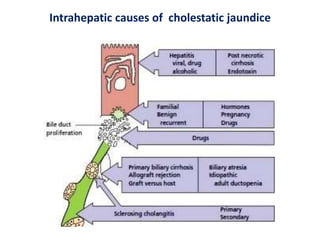
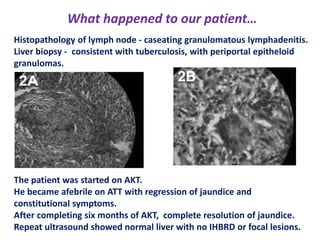
A 45-year-old male presented with jaundice, abdominal distension, and pain. Imaging found intrahepatic biliary radical dilatation and lymphadenopathy. Liver biopsy was recommended to determine the underlying cause of cholestatic jaundice and evaluate for possible malignancy given concerning findings on CT scan and clinical presentation.