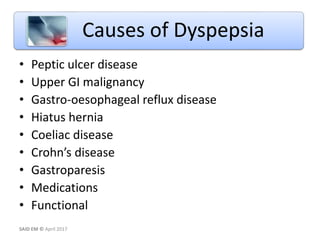
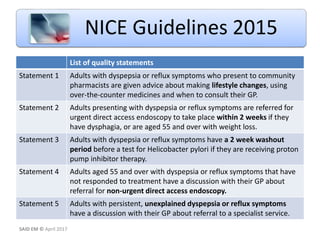
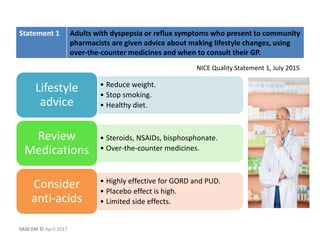
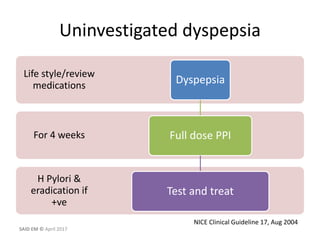
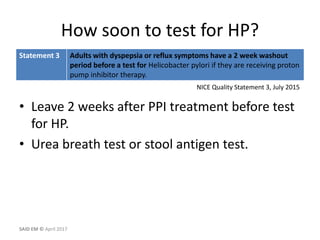
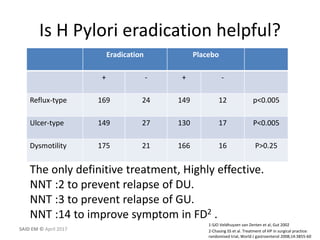
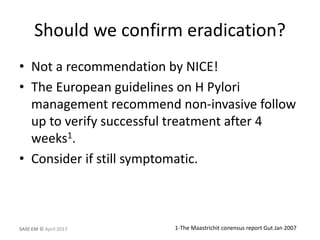
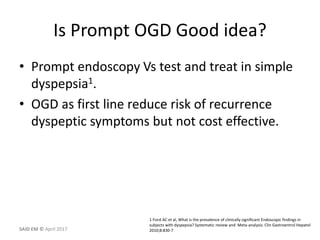
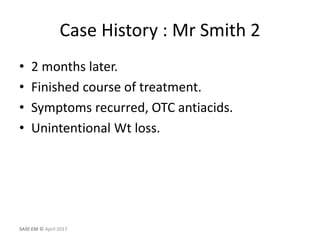
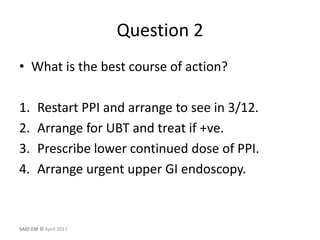
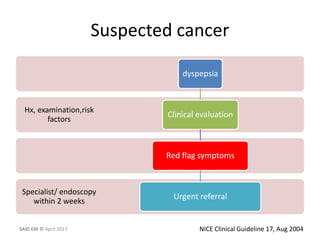
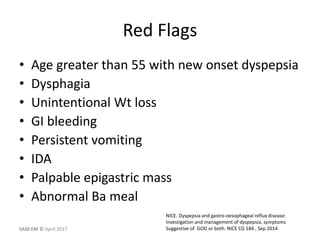
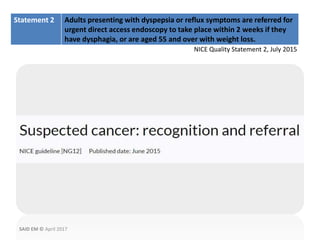
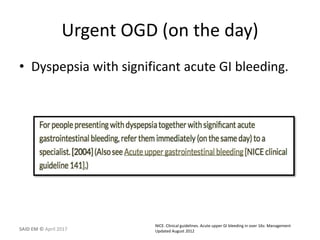
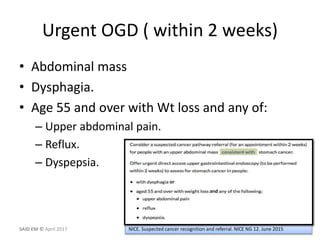
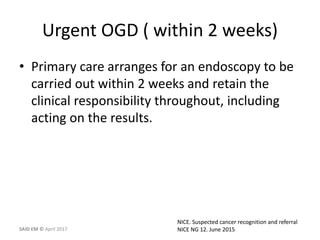
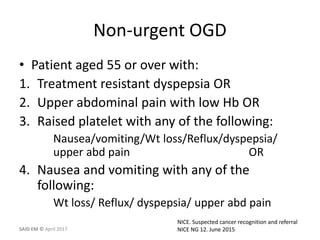
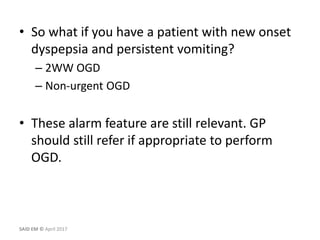
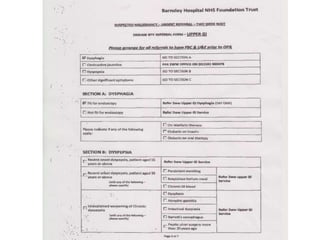
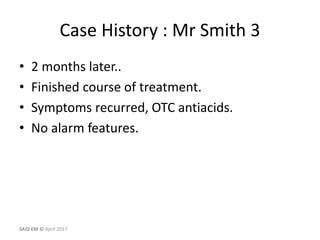
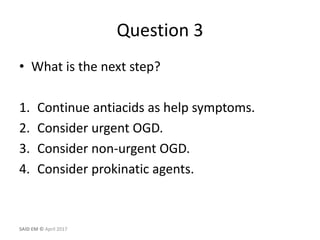
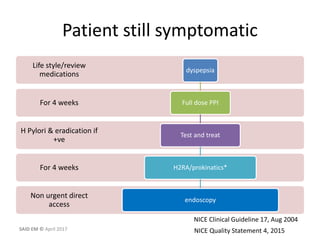
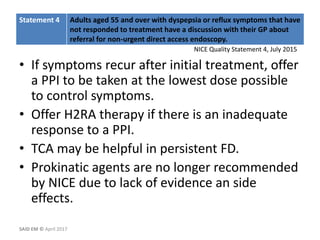
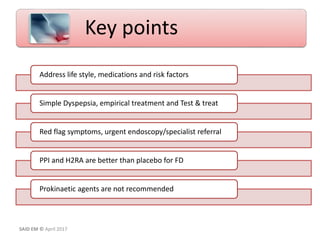
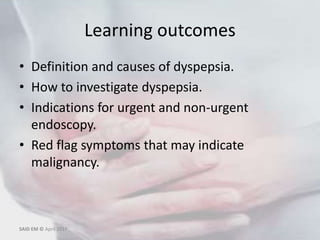
This document provides information on dyspepsia, including its definition, causes, investigations, and management guidelines. It begins by defining dyspepsia and outlining its prevalence in the UK population. It then discusses the common and rare causes of dyspepsia and how to investigate patients. The document reviews guidelines from NICE on investigating and managing dyspepsia. It provides examples of case histories and questions to help apply the guidelines. Key points are emphasized, such as addressing lifestyle factors, empirically treating dyspepsia, and referring patients with red flag symptoms urgently for endoscopy.

![NICE quality standard [QS96]
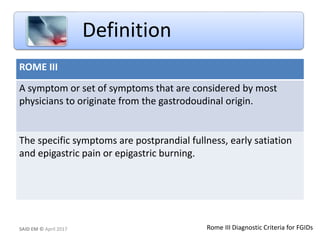
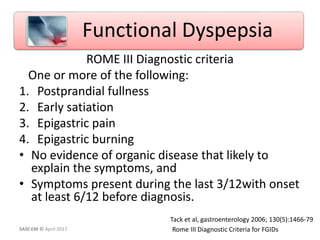
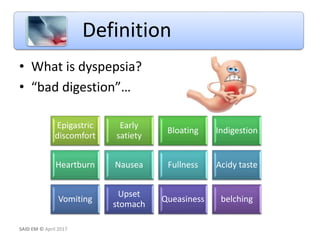
Dyspepsia pain or discomfort in the upper abdomen, including
upper abdominal fullness, early satiety, belching, bloating, and
nausea and/or vomiting
Functional presence of gastroduodenal symptoms in the
absence of any organic, metabolic, or systemic disease to explain
them.
Definition
Dyspepsia and gastro-oesophageal reflux disease
in adults: investigation and management July 2015SAID EM © April 2017](https://image.slidesharecdn.com/dyspepsiabestversion1-170512212658/85/Dyspepsia-6-320.jpg)