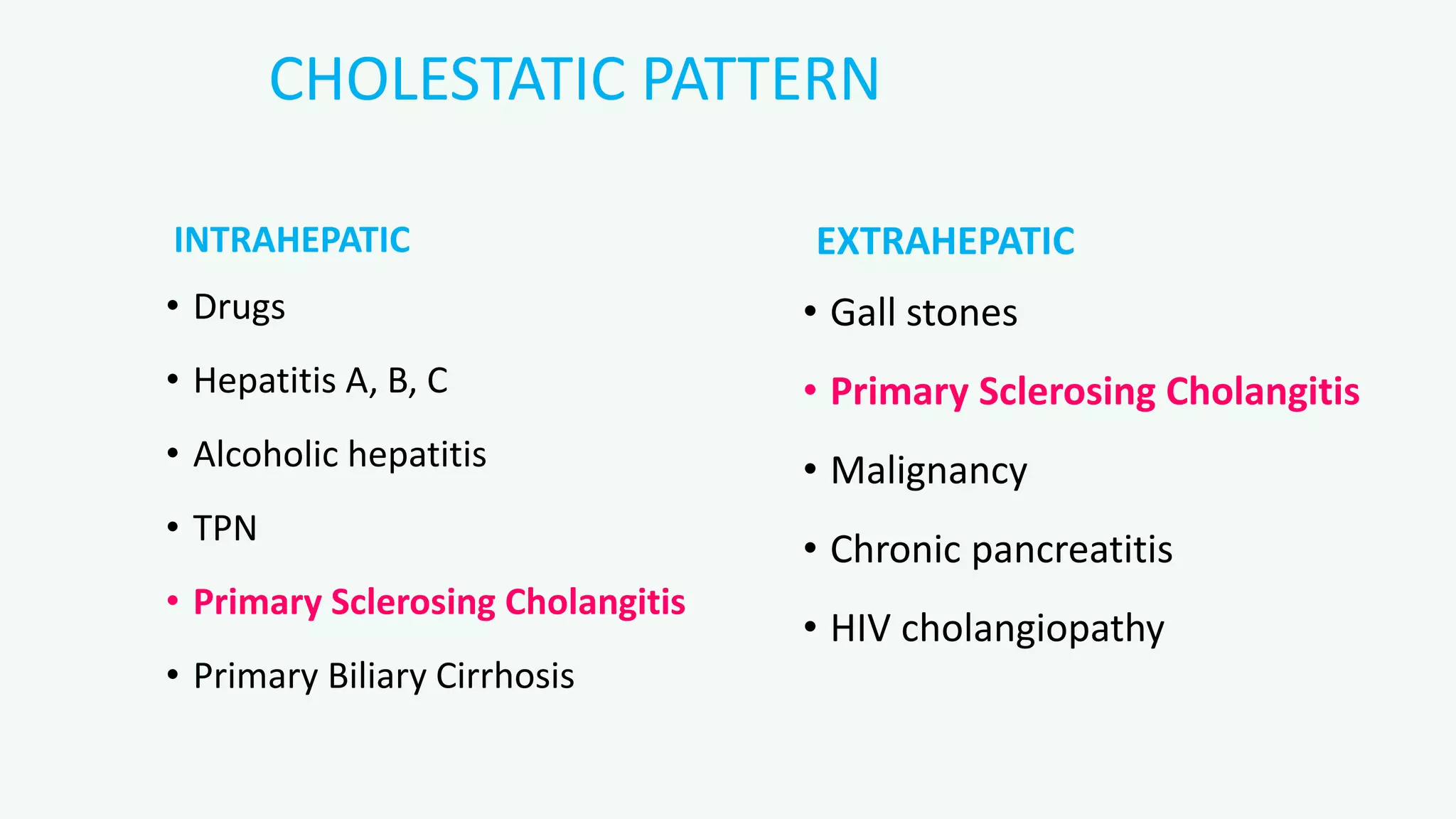
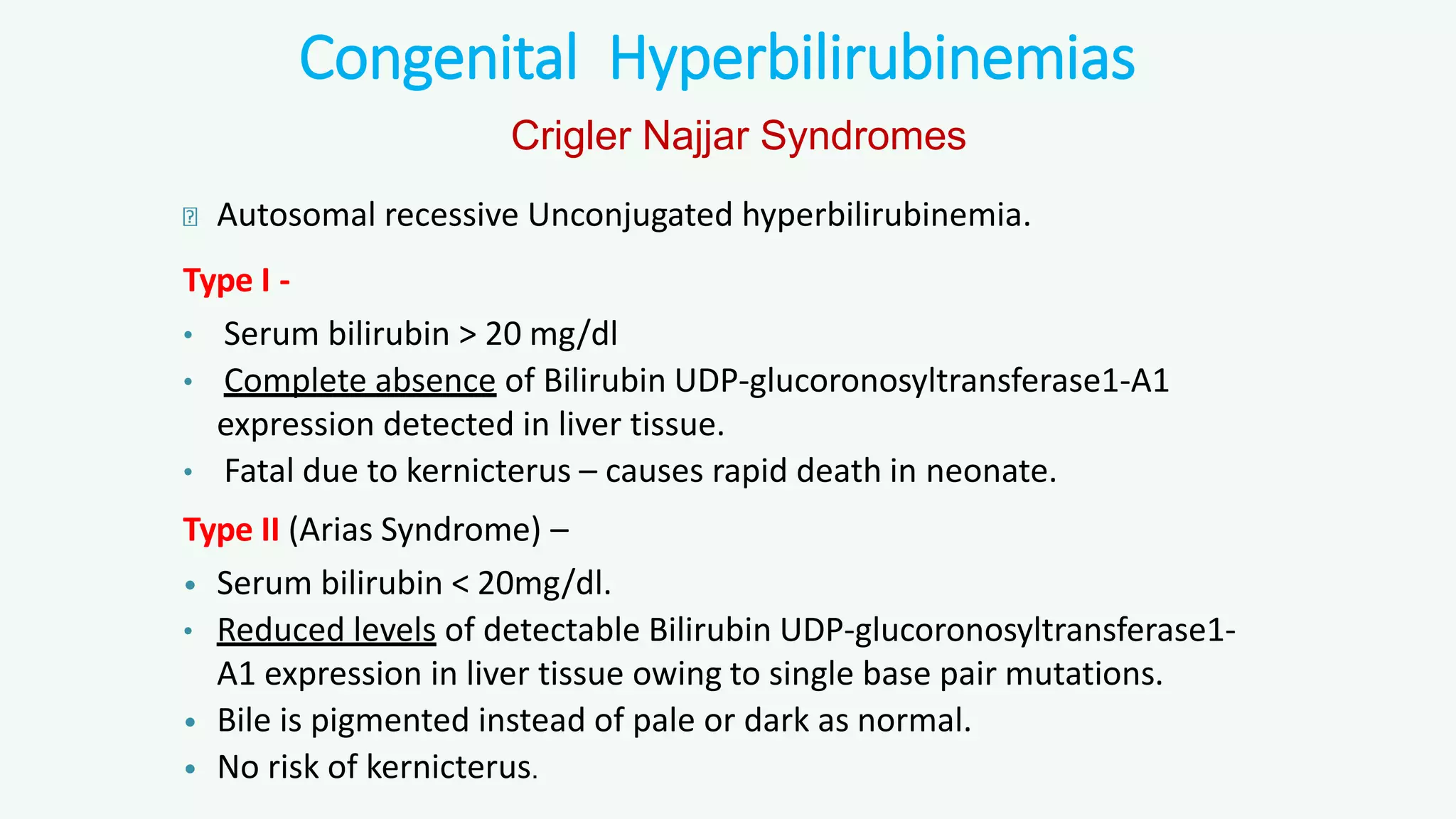
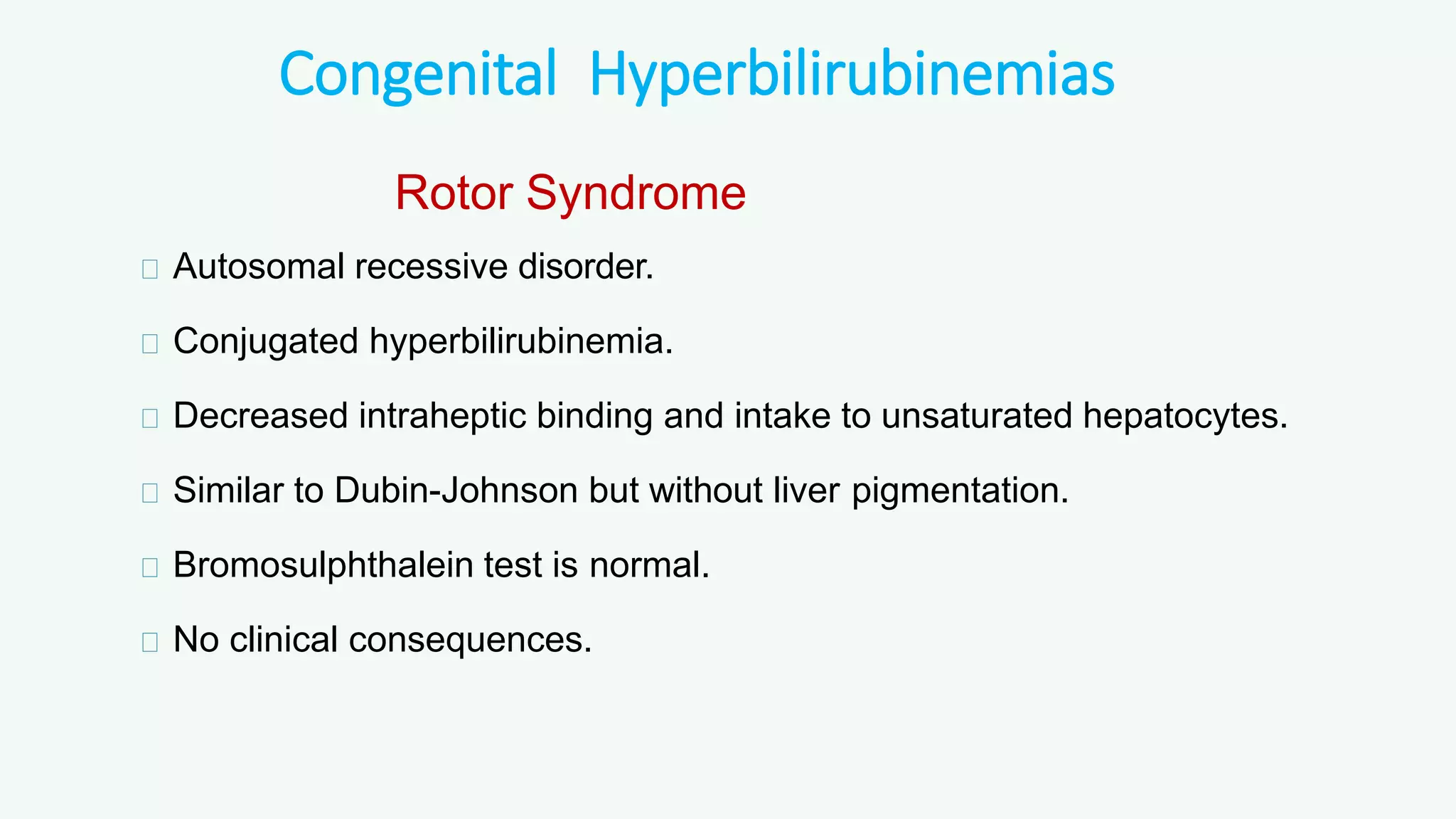
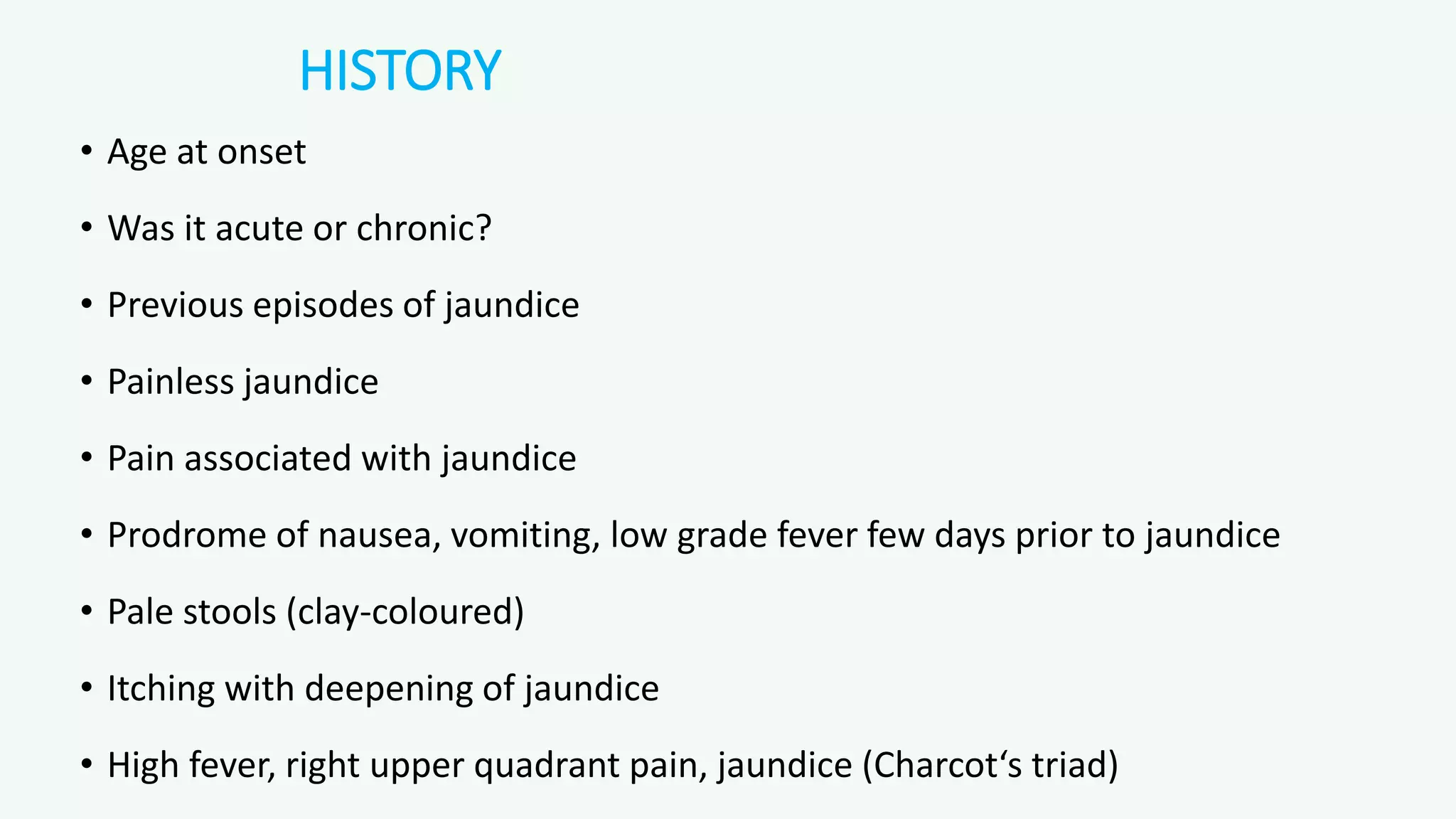
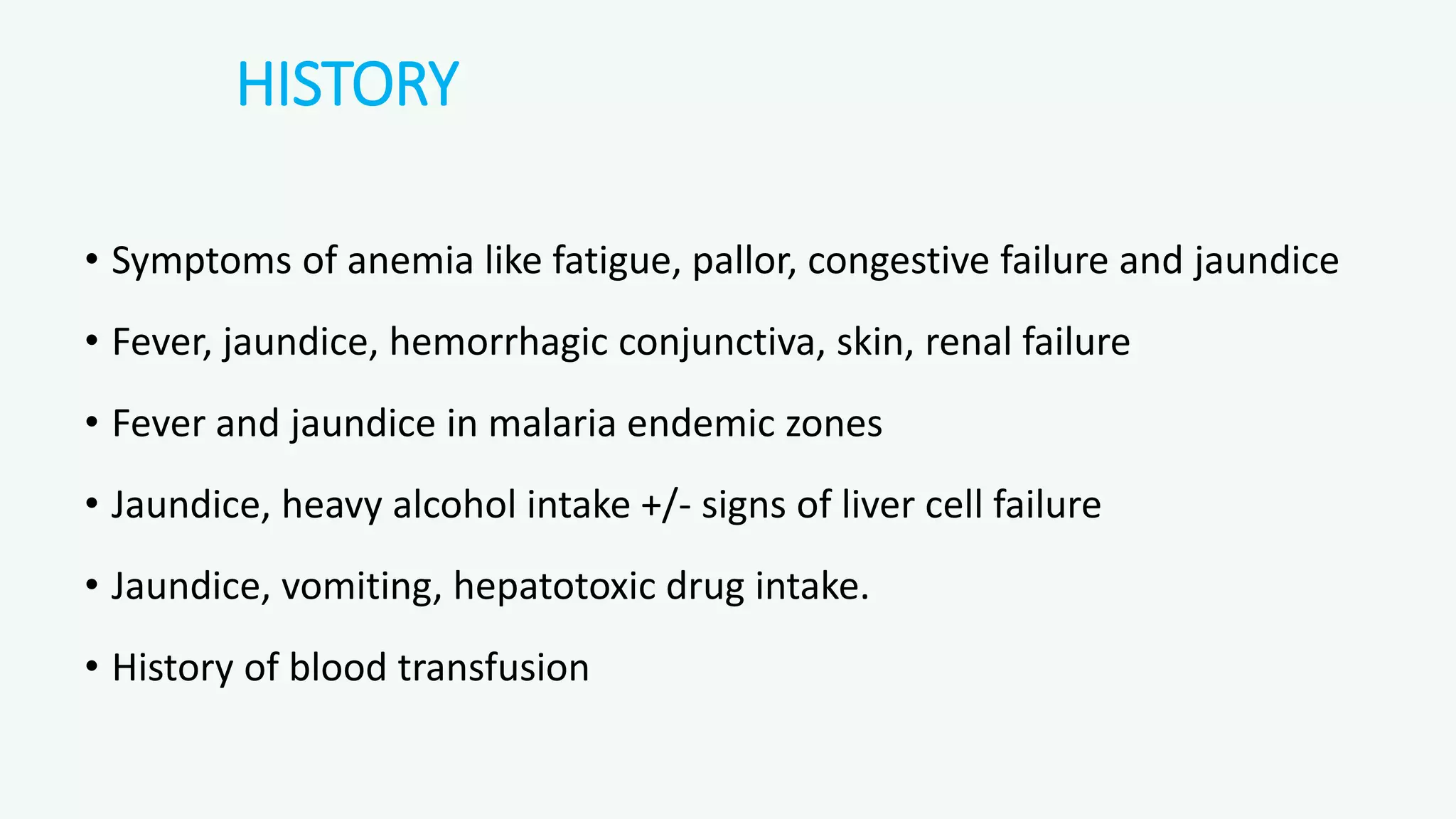
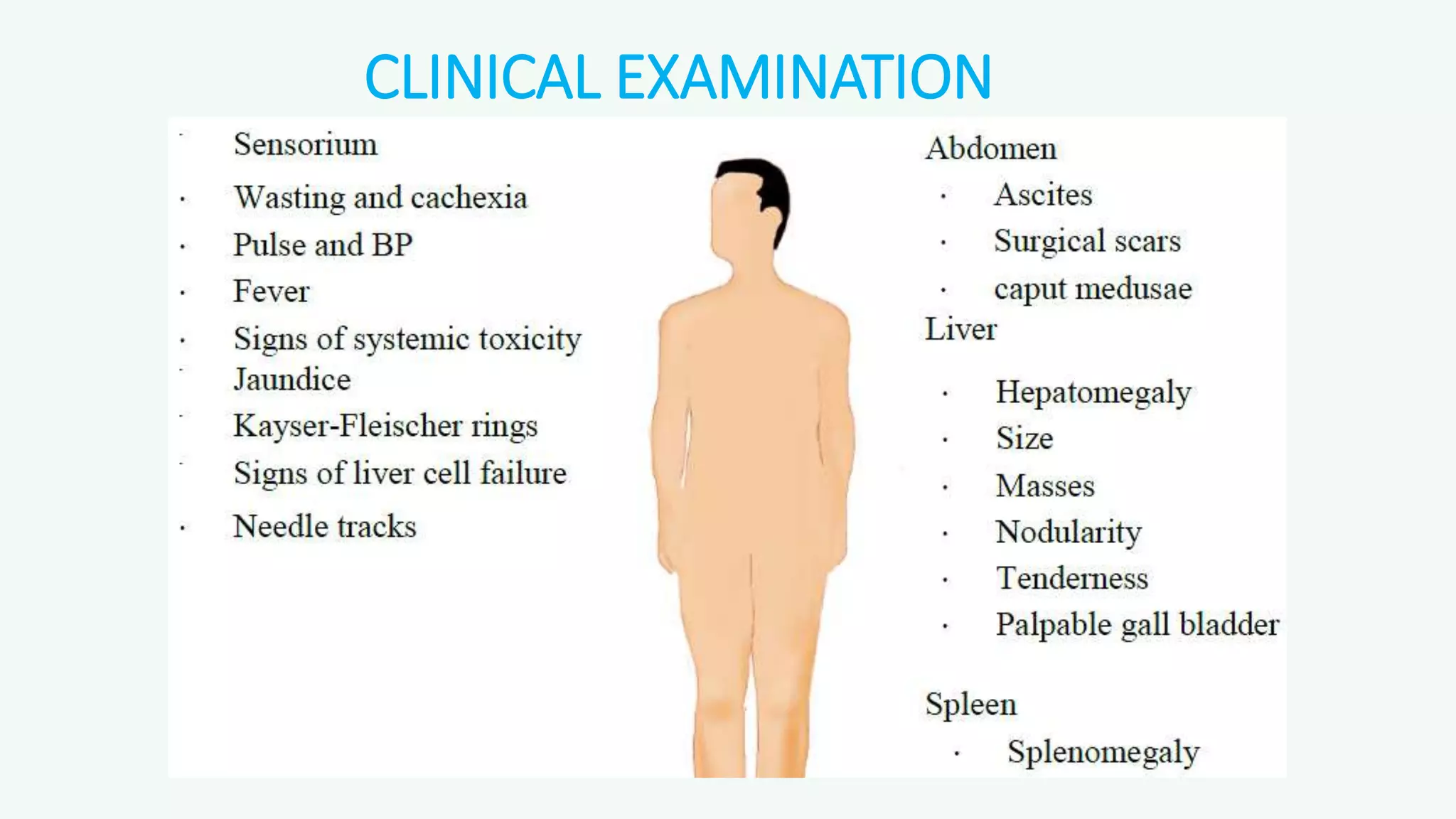
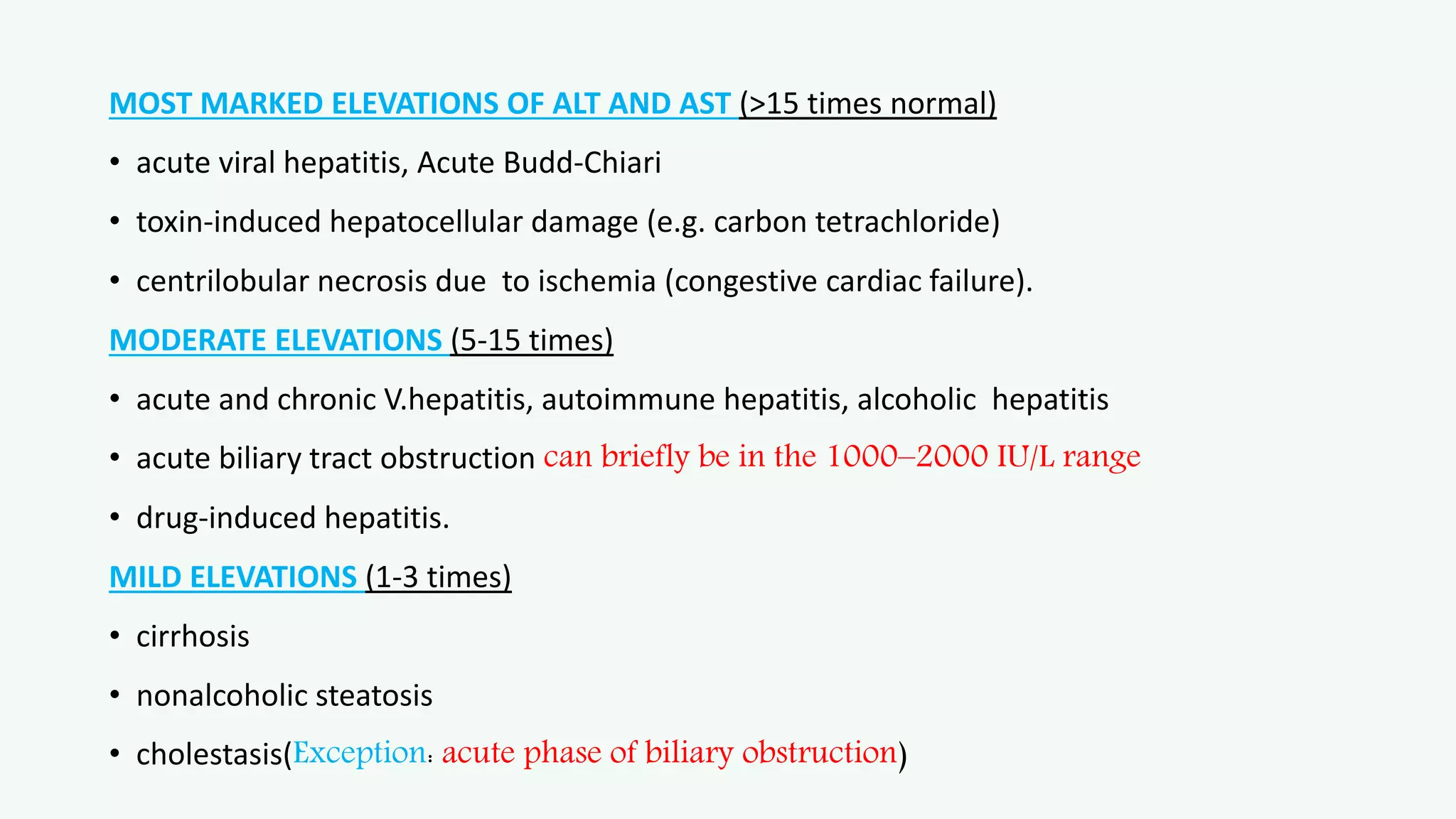
This document provides an overview of jaundice and its evaluation. It defines jaundice and discusses serum bilirubin levels. It covers the bilirubin production and metabolism pathways. It describes the classification of jaundice by etiology, bilirubin type, and site of disease. Key investigations for evaluating a patient with jaundice are outlined. Important aspects of history taking and clinical examination are highlighted.