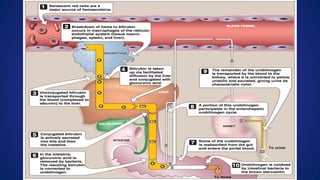
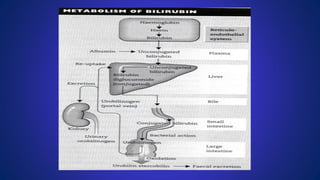
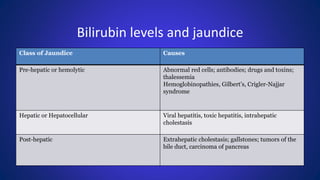
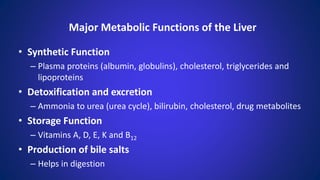
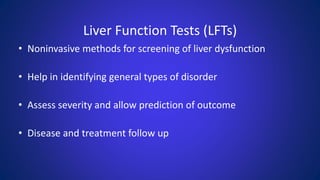
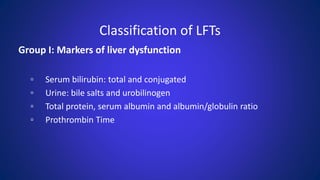
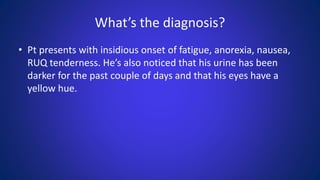
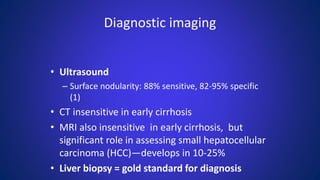
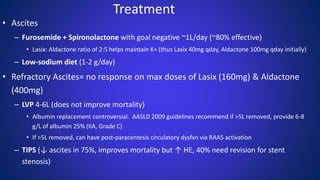
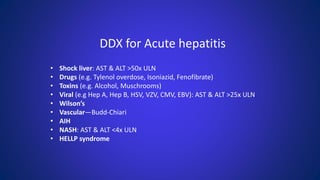
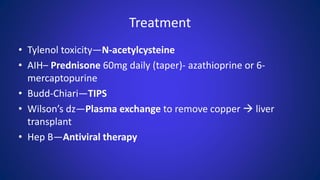
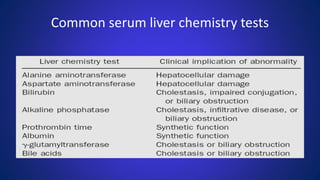
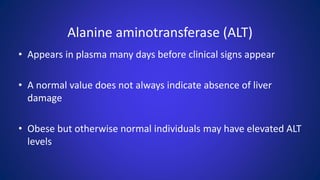
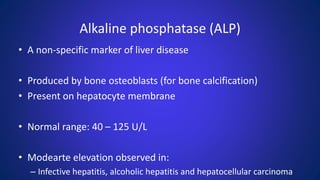
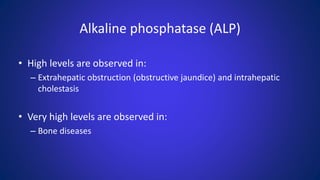
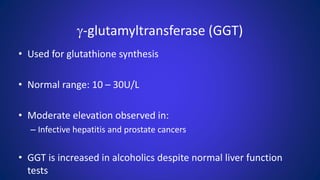
The document discusses liver function tests (LFTs), which are blood tests that provide information about the state of a patient's liver. It describes various LFTs that measure different aspects of liver function, including injury, biosynthesis, and biliary obstruction. Common LFTs examined are total bilirubin, ALT, AST, alkaline phosphatase, and GGT. Elevations in certain LFTs can indicate liver diseases like hepatitis, cirrhosis, or cancer. The tests are important for detecting early liver issues, assessing severity, and monitoring treatment effectiveness.

![Liver function tests
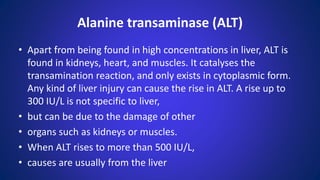
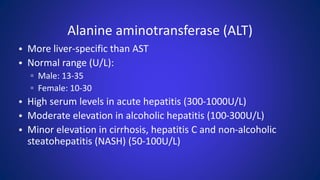
• The liver
– transaminases aspartate transaminase
– (AST or SGOT) and alanine transaminase
– (ALT or SGPT) are useful biomarkers of
– liver injury in a patient with some degree
– of intact liver function.[2][3][4] Most liver
– diseases cause only mild symptoms](https://image.slidesharecdn.com/lfts-230605050959-521c4f19/85/LFTs-pdf-5-320.jpg)

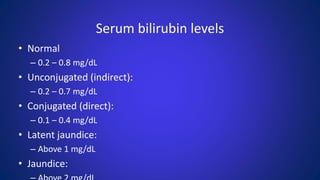
![Total bilirubin
• Reference range in adults
• Parameters/units Total bilirubin Unconjugated bilirubin
Conjugated bilirubin
• mg/dL 0.1–1.0[5] 0.2-0.7[5] 0.1–0.4[5]
• μmol/l 2.0 to 21[6] < 12[6] < 8[6]
• Measurement of total bilirubin includes
• both unconjugated (indirect) and](https://image.slidesharecdn.com/lfts-230605050959-521c4f19/85/LFTs-pdf-27-320.jpg)
![• In acute appendicitis, total bilirubin can
• rise from 20.52 μmol/l to 143 μmol/l. In
• pregnant women, the total bilirubin level
• is low in all three trimesters.[6]
• The measurement of bilirubin levels in
• the newborns is done through the use of
• bilimeter or transcutanoeus](https://image.slidesharecdn.com/lfts-230605050959-521c4f19/85/LFTs-pdf-33-320.jpg)
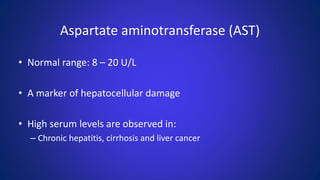
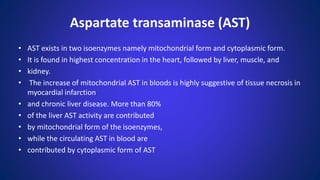
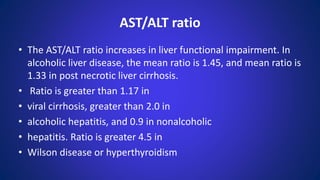
![• AST is especially markedly raised in
• those with liver cirrhosis.[6] AST can be
• released from a variety of other tissues
• and if the elevation is less than two times
• the normal AST then no further workup
• needs to be performed if a patient is
• proceeding to surgery.
Aspartate transaminase (AST)](https://image.slidesharecdn.com/lfts-230605050959-521c4f19/85/LFTs-pdf-49-320.jpg)