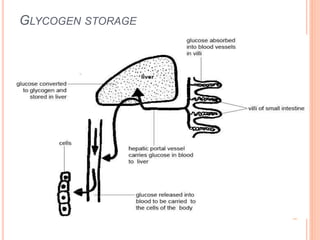
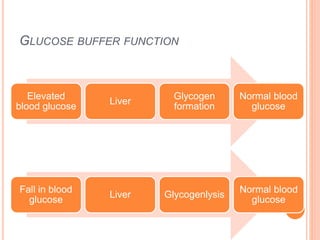
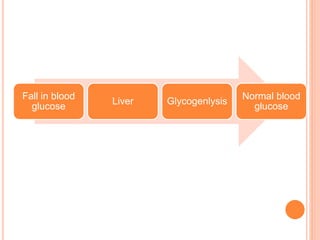
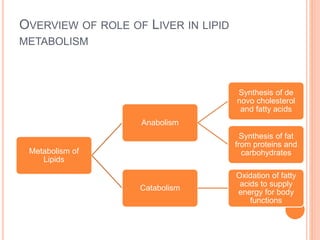
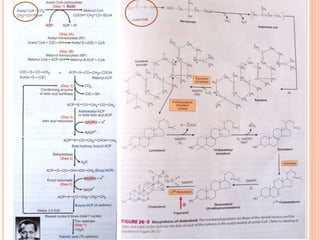
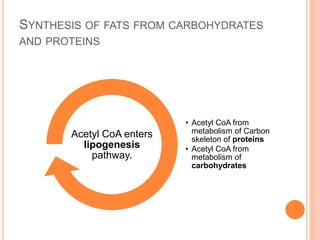
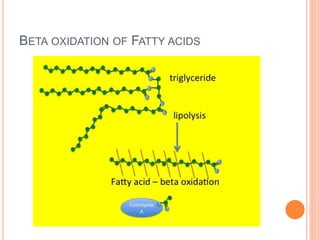
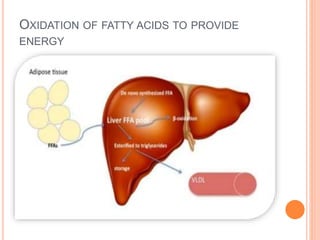
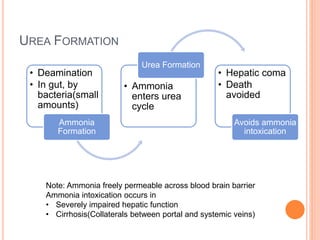
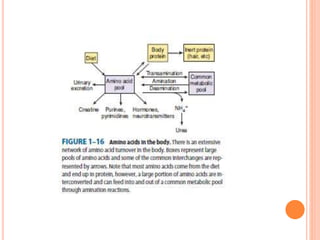
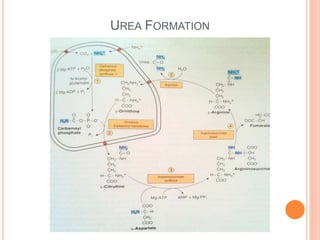
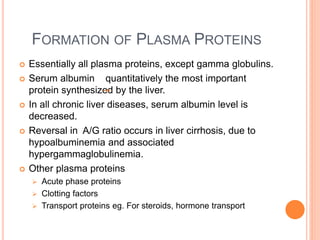
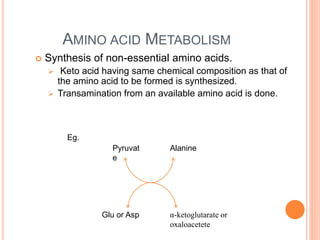
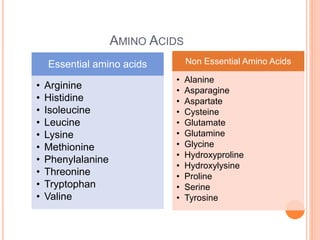
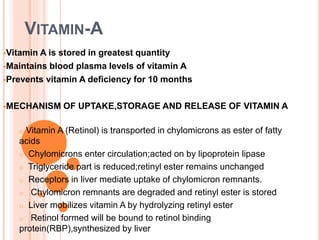
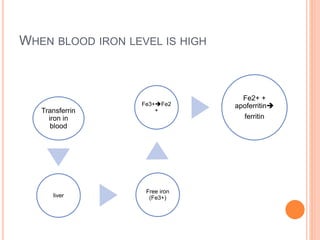
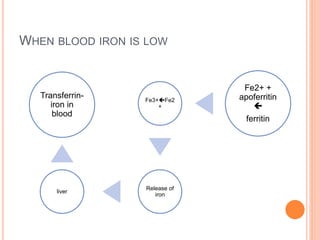
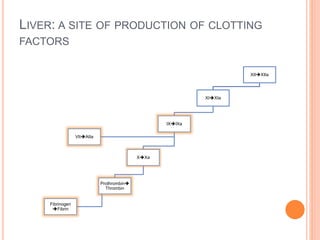
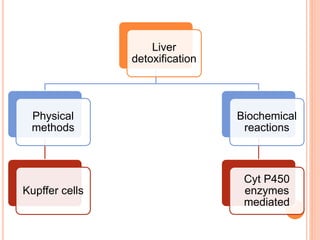
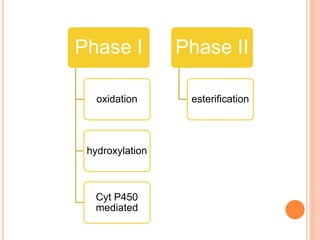
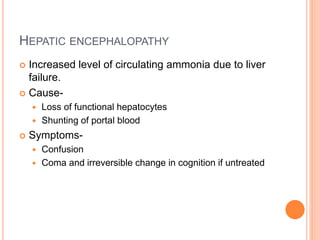
The liver performs many important metabolic functions including carbohydrate, fat, and protein metabolism. It stores glycogen, gluconeogenesis, and converts galactose and fructose to glucose. The liver synthesizes, oxidizes, and transports lipids. It deaminates amino acids, forms urea to remove ammonia, and synthesizes plasma proteins. The liver also stores vitamins A, D, B12 and iron. It produces clotting factors and aids in detoxification through phase I and II reactions. Liver failure can cause hepatic encephalopathy due to increased ammonia levels.