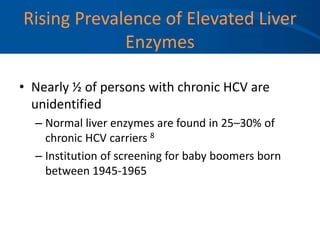
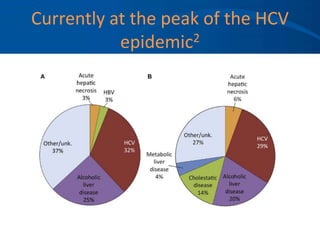
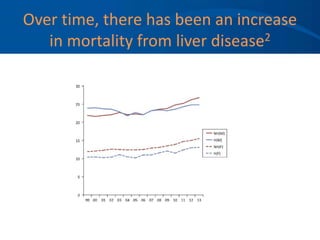
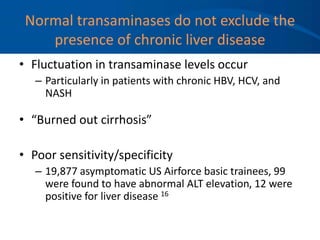
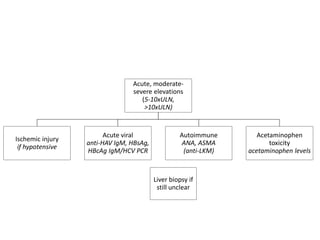
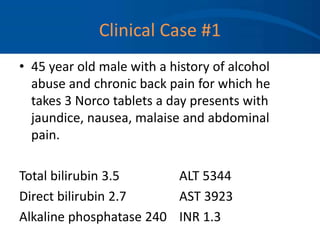
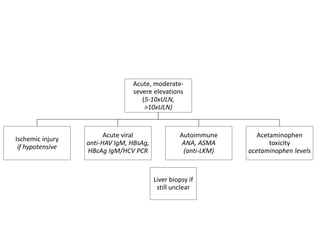
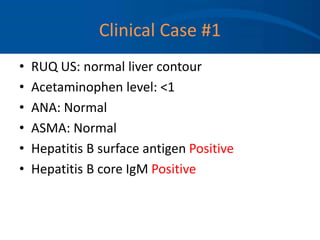
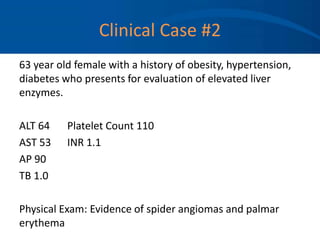
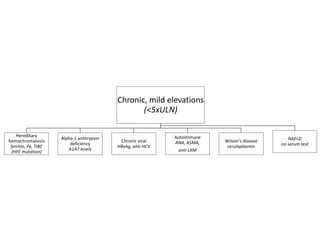
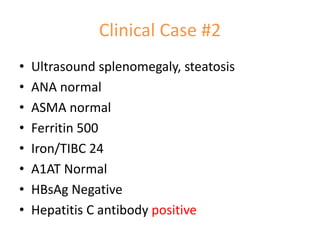
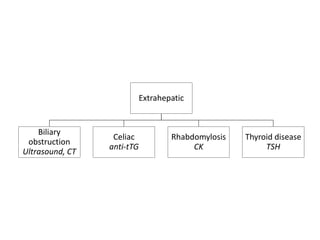
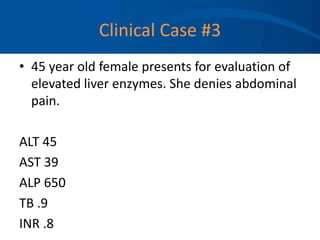
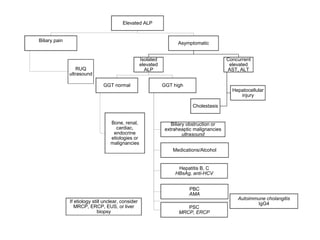
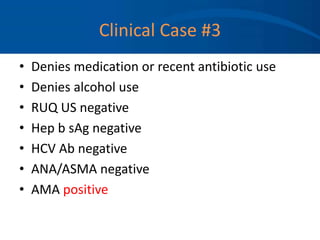
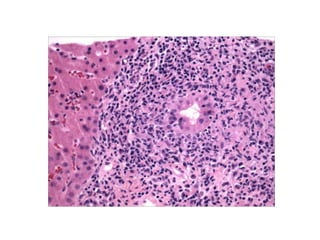
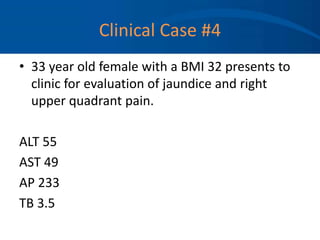
This document provides an overview on evaluating and managing elevated liver enzymes. It discusses the prevalence of liver disease in the US and the importance of identifying abnormal liver enzymes. The document reviews how to interpret different liver enzymes and develop a differential diagnosis for acute vs chronic conditions. Clinical cases are presented to demonstrate how to investigate the underlying cause of elevated enzymes. The conclusion emphasizes that stable elevated enzymes do not exist and screening is important given rising rates of HCV and NASH.


![References
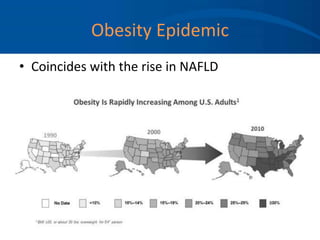
1. Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from
1988 to 2008. Clin Gastroenterol Hepatol. 2011 Jun;9(6):524-530.
2. Udompap P, Kim D, Kim WR. Current and Future Burden of Chronic Nonmalignant Liver Disease. Clin Gastroenterol Hepatol. 2015 Nov;13(12):2031-41.
Epub 2015 Aug 17.
3. Hultcrantz R, Glaumann H, Lindberg G, Nilsson LH. Liver investigation in 149 asymptomatic patients with moderately elevated activities of serum
aminotransferases. Scand J Gastroenterol 1986; 21:109–113.
4. Ioanou GN, Boyko EJ, Lee SP. The prevalence and predictors of elevated serum aminotransferase activity in the United States in 1999-2002. Am J
Gastroenterol 2006; 101:76–82.
5. Chou R et al. Agency for Healthcare Research and Quality; 2012.
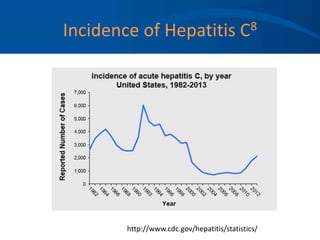
6. Chak E et al. Liver Int. 2011 Sep;31(8):1090-101.
7. Lavanchy D. Liver Int. 2009 Jan;29 Suppl 1:74-81.
8. Puoti C, Castellacci R, Montagnese F et al. Histological and virological features and follow-up of hepatitis C virus carriers with normal aminotransferase
levels: the Italian prospective study of the asymptomatic C carriers (ISACC). J Hepatol 2002; 37: 117–123.
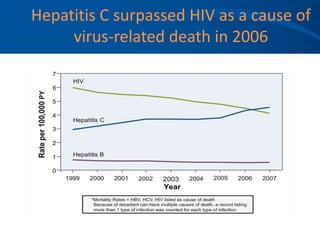
9. Ly KN et al. Ann Intern Med. 2012;156:271-8.
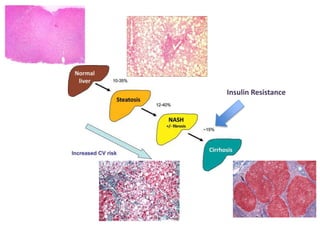
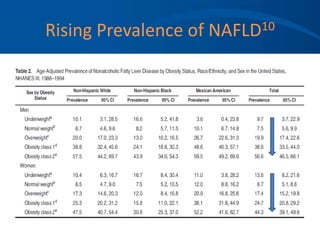
10. Lazo M, Hernaez R, Eberhardt MS, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition
Examination Survey, 1988-1994. Am J Epidemiol. 2013 Jul 1;178(1):38-45.
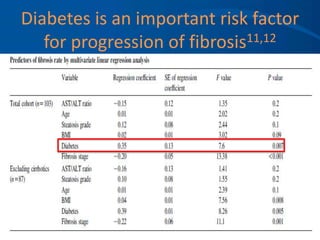
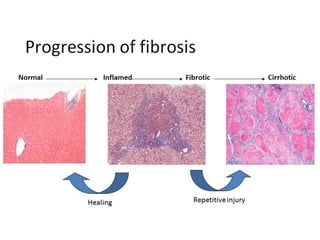
11. L.A. Adams, S. Sanderson, K.D. Lindor, P. Angulo. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with
sequential liver biopsies. J Hepatol, 42 (2005), pp. 132–138.
12. McPherson S, Hardy T, Henderson E, et al. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications
for prognosis and clinical management. J Hepatol. 2015 May;62(5):1148-55.
13. Heron M. Natl Vital Stat Rep.2012;61:1–96.
14. Scaglione S et al. J Clin Gastroenterol. 2014 Oct 8.
15. Chou R et al. Agency for Healthcare Research and Quality; 2012.
16. Kundrotas LW; Clement DJ. Serum alanine aminotransferase (ALT) elevation in asymptomatic US Air Force basic trainee blood donors. Dig Dis Sci 1993;
38:2145-2150
17. Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003
May;98(5):960–7.
18. Liangpunsakul S, Chalasani N. Unexplained Elevations in Alanine Aminotransferase in Individuals with the Metabolic Syndrome: Results from the Third
National Health and Nutrition Survey (NHANES III). The American Journal of the Medical Sciences [Internet]. 2005;329(3).](https://image.slidesharecdn.com/2-approach-to-elevated-lft-230705084702-92dcb83b/85/2-Approach-to-Elevated-LFT-ppt-58-320.jpg)
