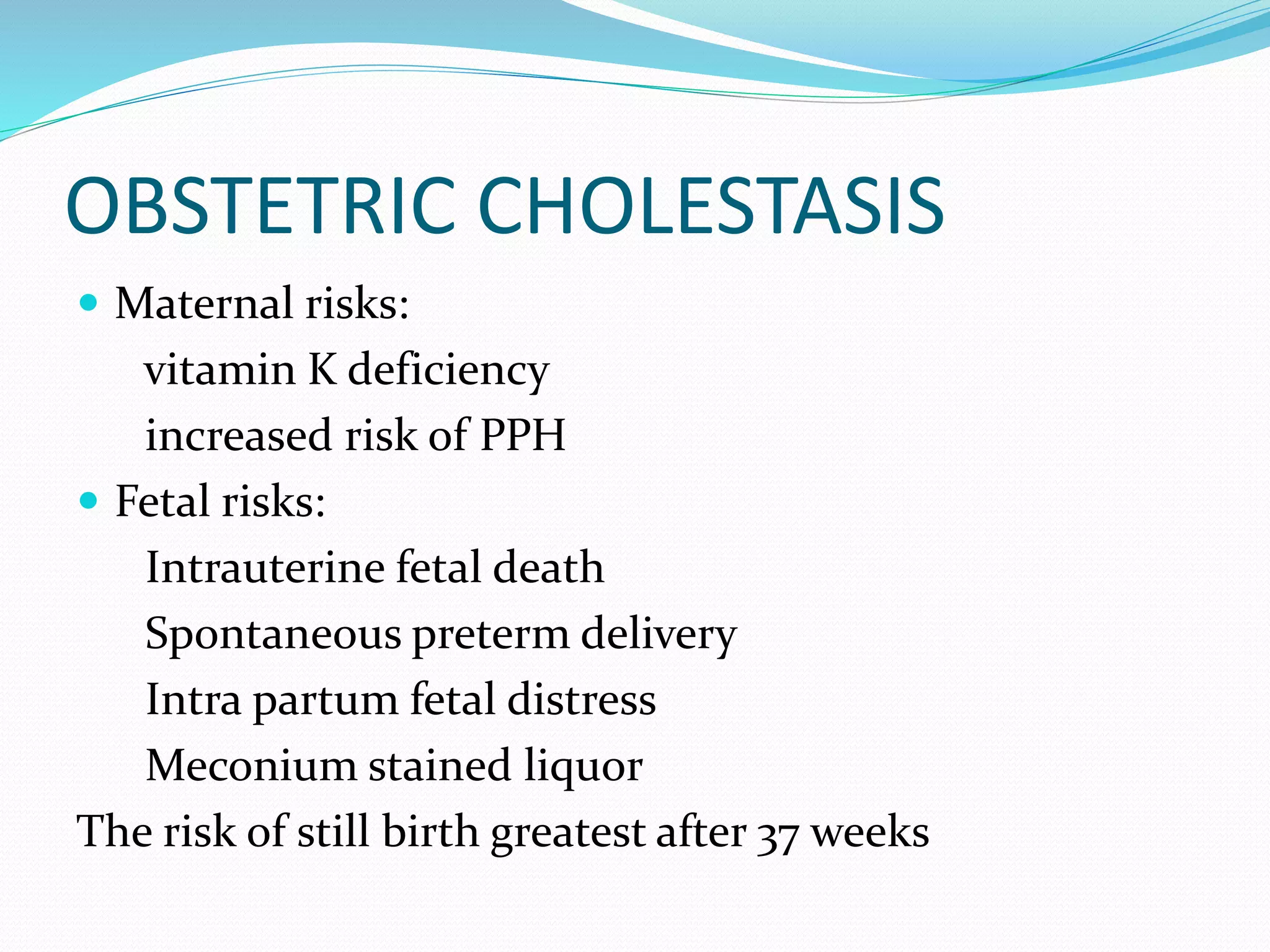
This document discusses various causes of jaundice that can occur during pregnancy. It begins with definitions of jaundice and normal liver physiology during pregnancy. It then discusses changes in liver function tests during pregnancy and the effects of maternal hyperbilirubinemia on the fetus. The main causes of jaundice unique to pregnancy are identified as intrahepatic cholestasis of pregnancy, acute fatty liver of pregnancy, HELLP syndrome, and severe hyperemesis gravidarum. Viral hepatitis, gallstones, autoimmune disorders and drugs are identified as causes that can coincide with pregnancy. Details are provided on diagnosis and management of specific conditions like obstetric cholestasis, acute fatty liver of pregnancy, HEL