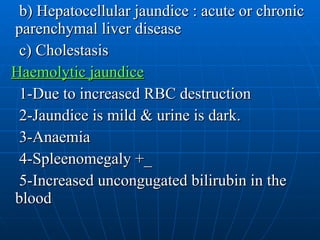
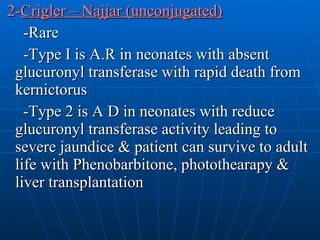
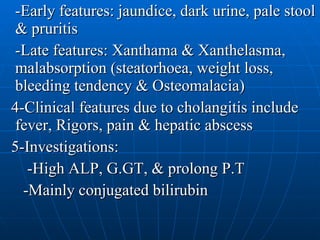
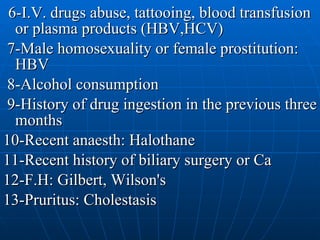
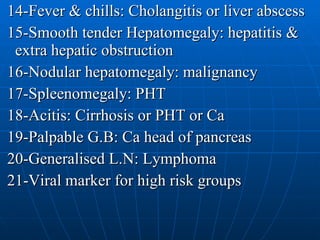
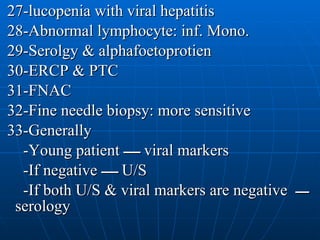
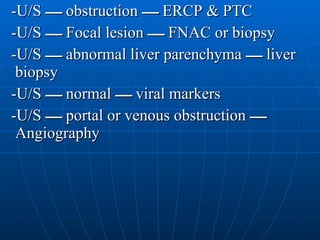
This document defines jaundice and discusses its various causes and mechanisms. Jaundice is caused by an increased bilirubin level in body fluids and can be due to increased production from hemolysis, impaired excretion from conditions like liver disease, or obstruction of bile flow from the liver or gallbladder. The causes, signs, investigations, and approach to evaluating a patient with jaundice are described.