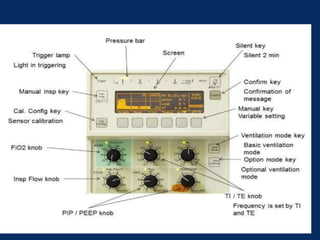
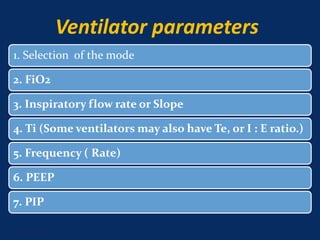
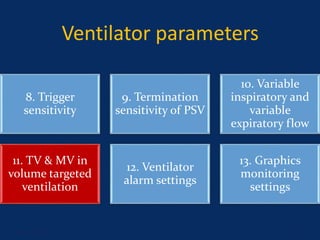
This document discusses ventilator settings and parameters. It covers:
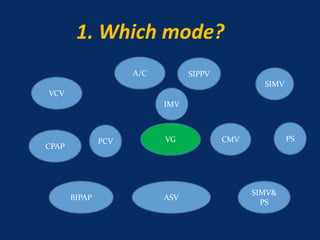
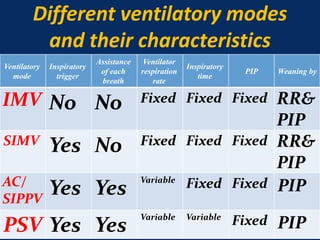
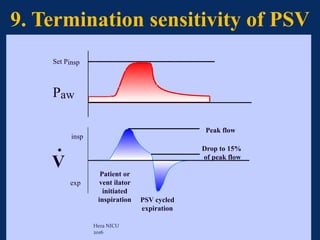
1. Modes of ventilation like IMV, SIMV, AC/SIPPV, PSV and their characteristics.
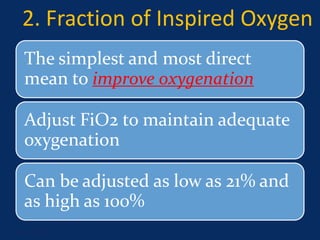
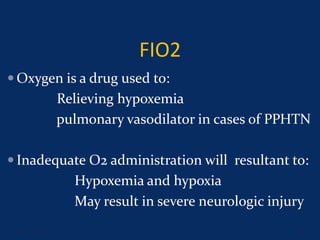
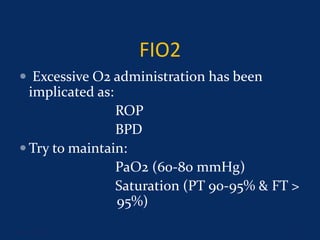
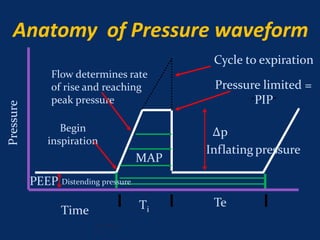
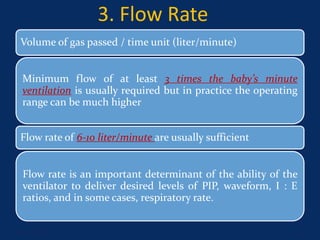
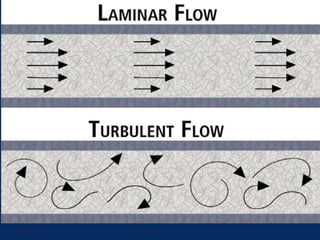
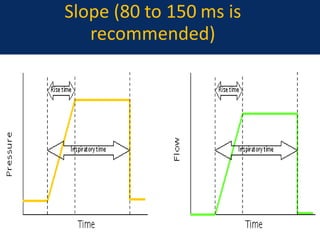
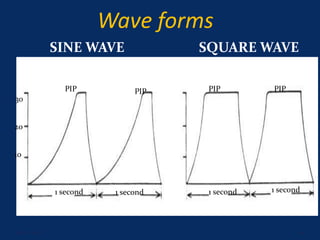
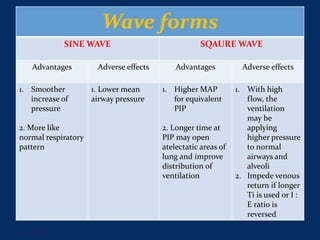
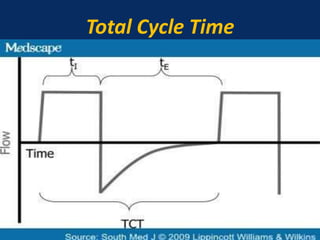
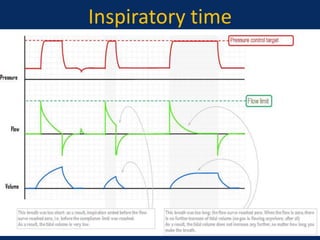
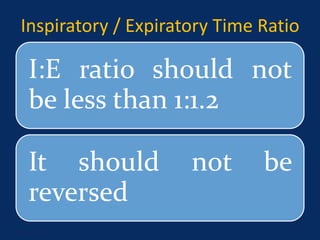
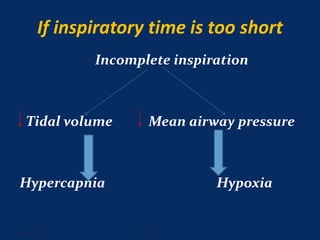
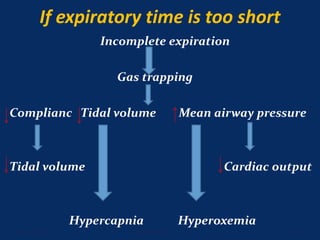
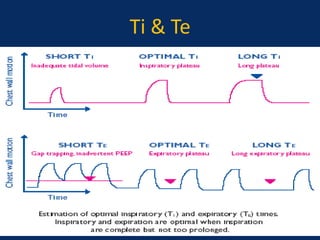
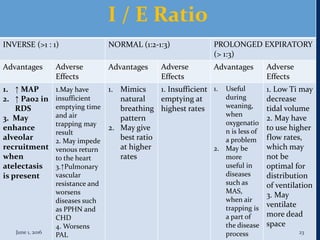
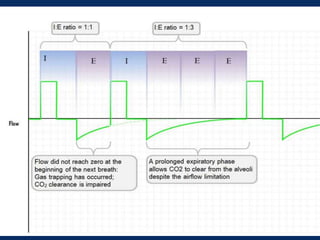
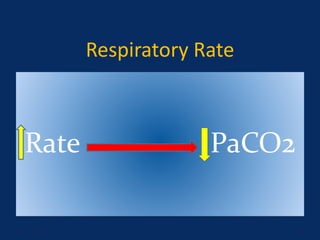
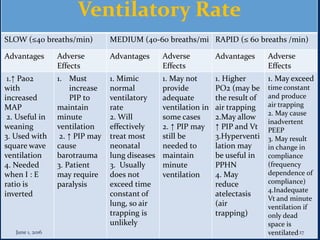
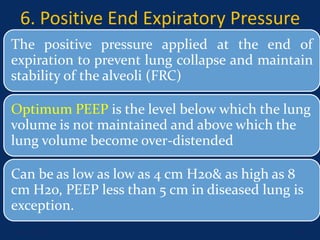
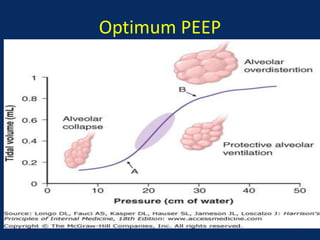
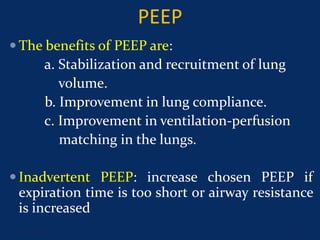
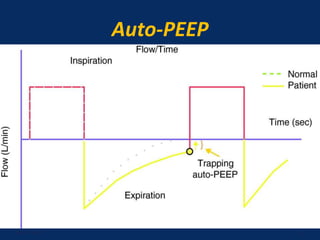
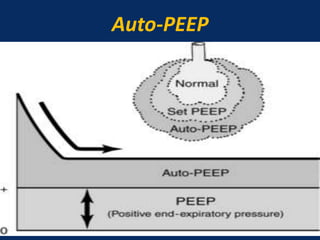
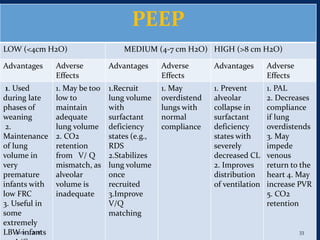
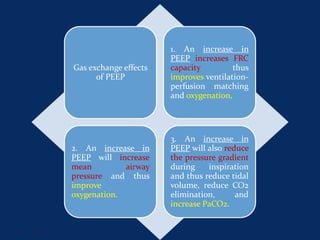
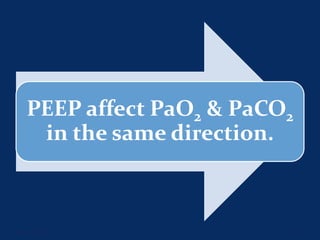
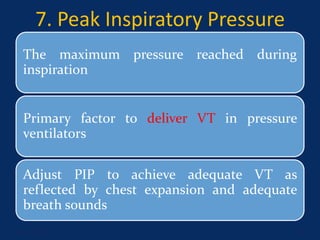
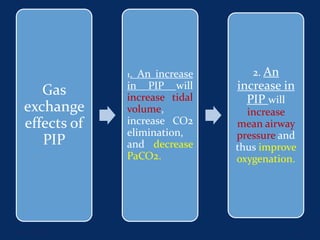
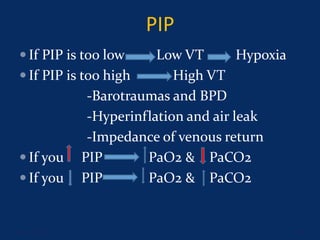
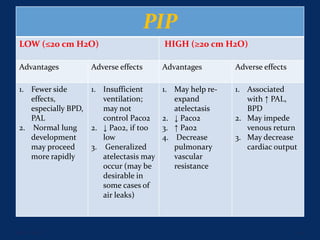
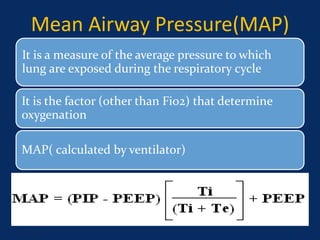
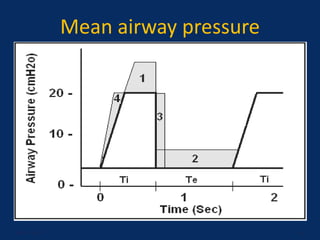
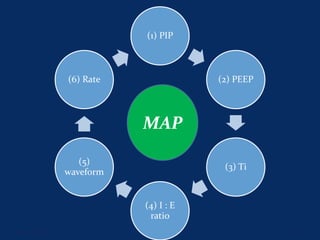
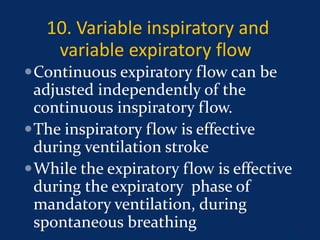
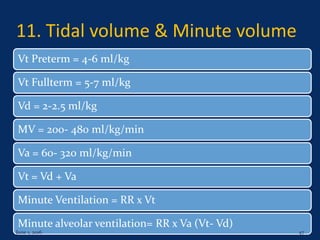
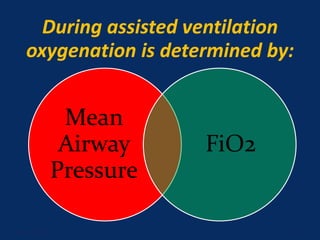
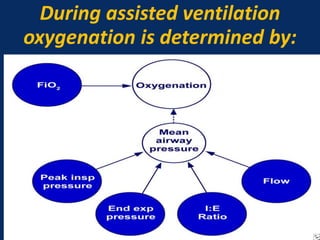
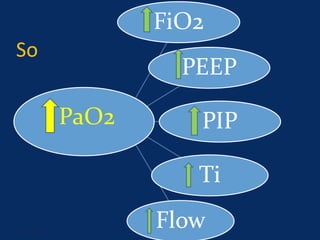
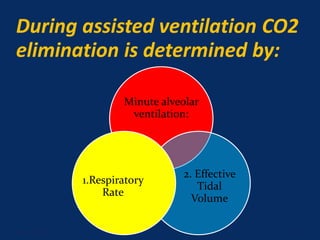
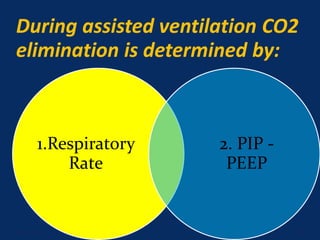
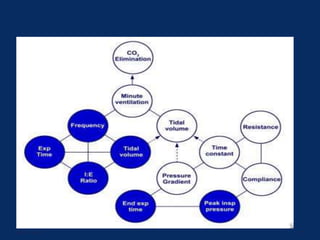
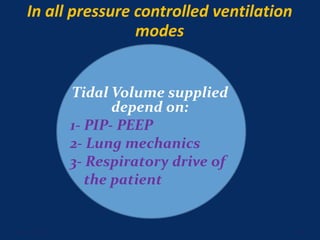
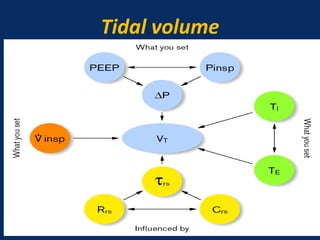
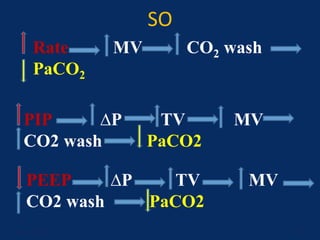
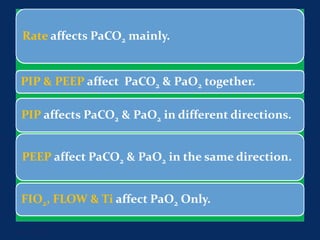
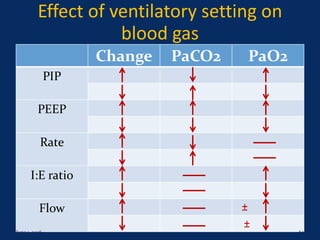
2. Parameters that determine gas exchange like FiO2, PEEP, PIP, flow rate, I:E ratio and how they affect oxygenation and ventilation.
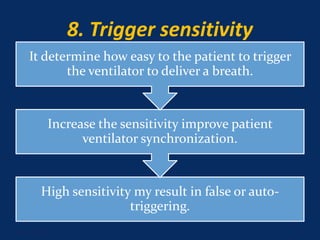
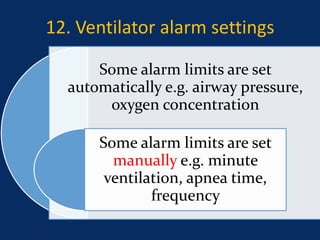
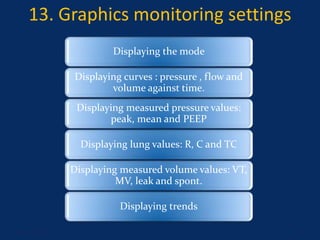
3. Other settings like trigger sensitivity, tidal volume, alarms and graphics that help optimize the ventilator for the patient's needs.
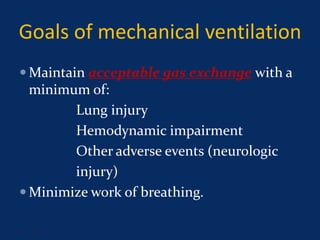
The goal is to maintain gas exchange with minimum lung injury or other adverse effects by properly adjusting these various settings.