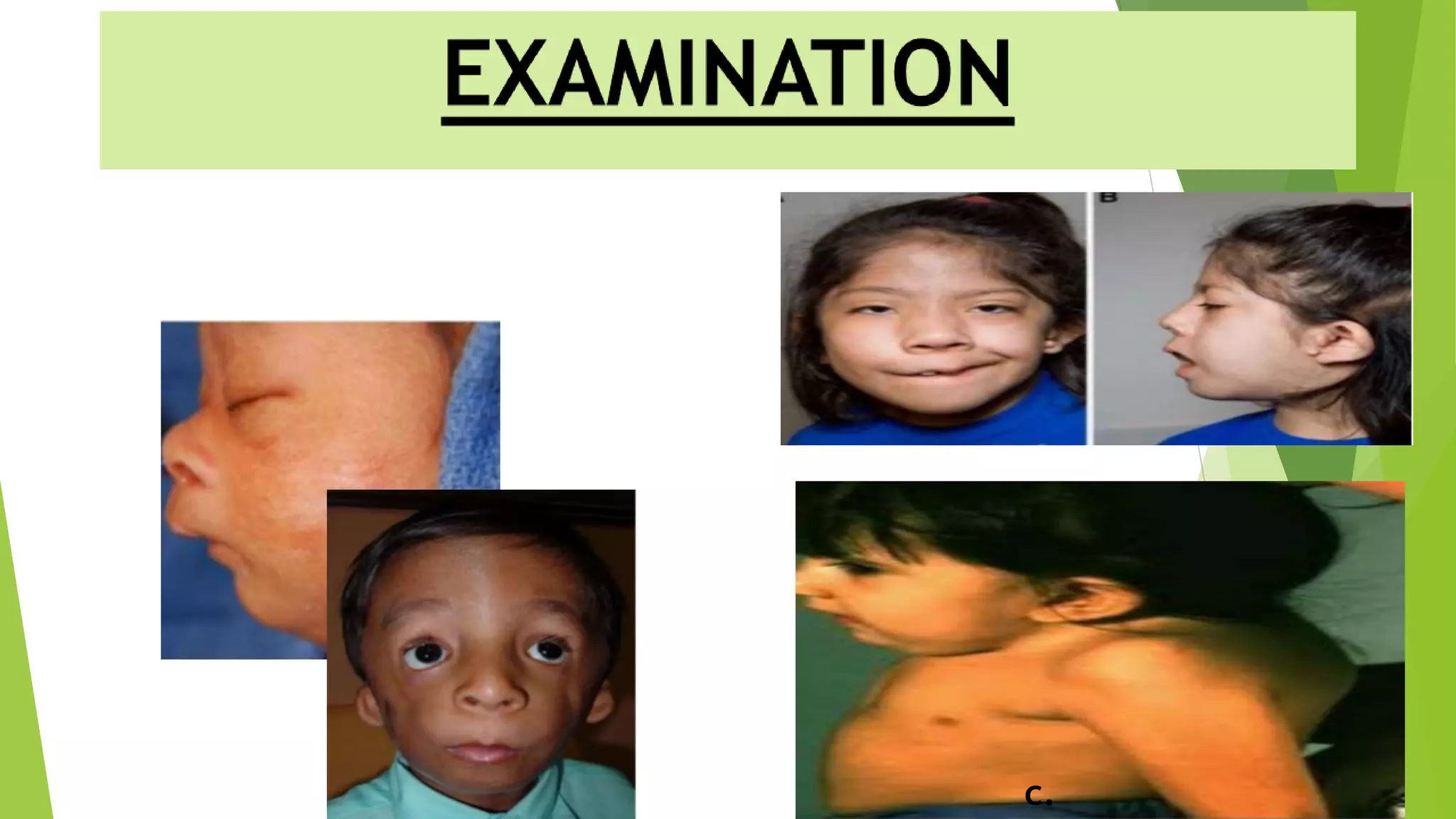
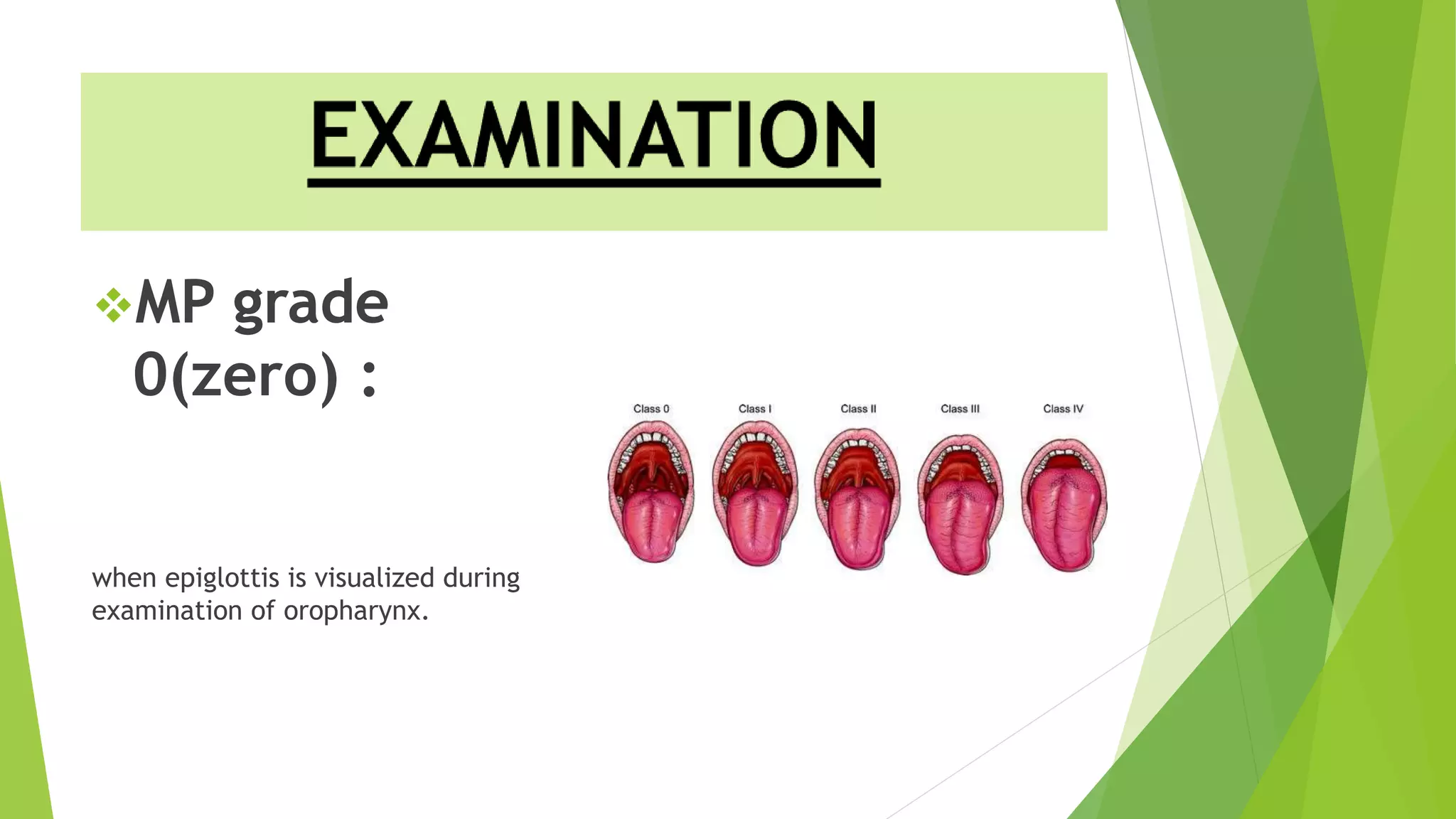
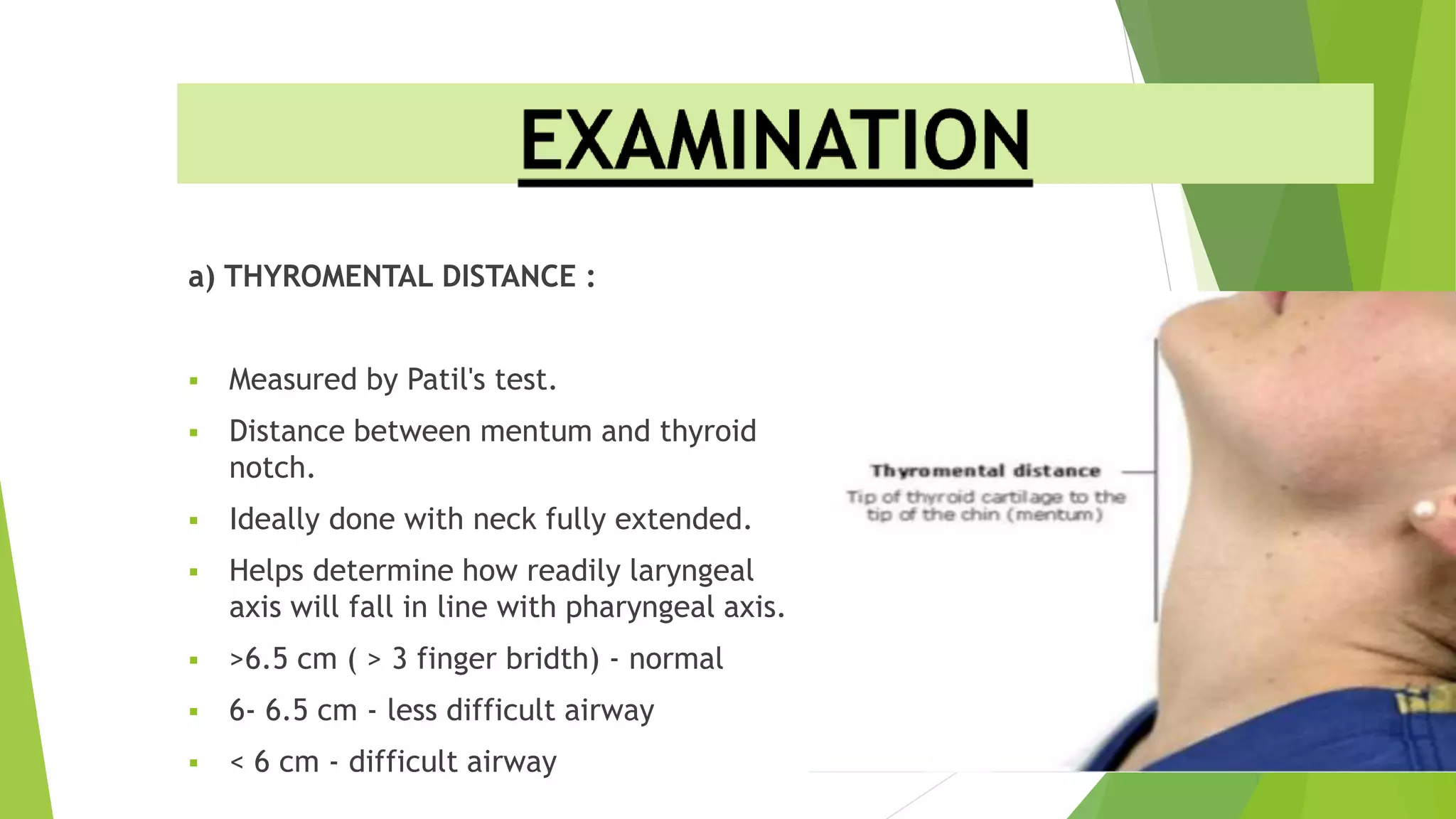
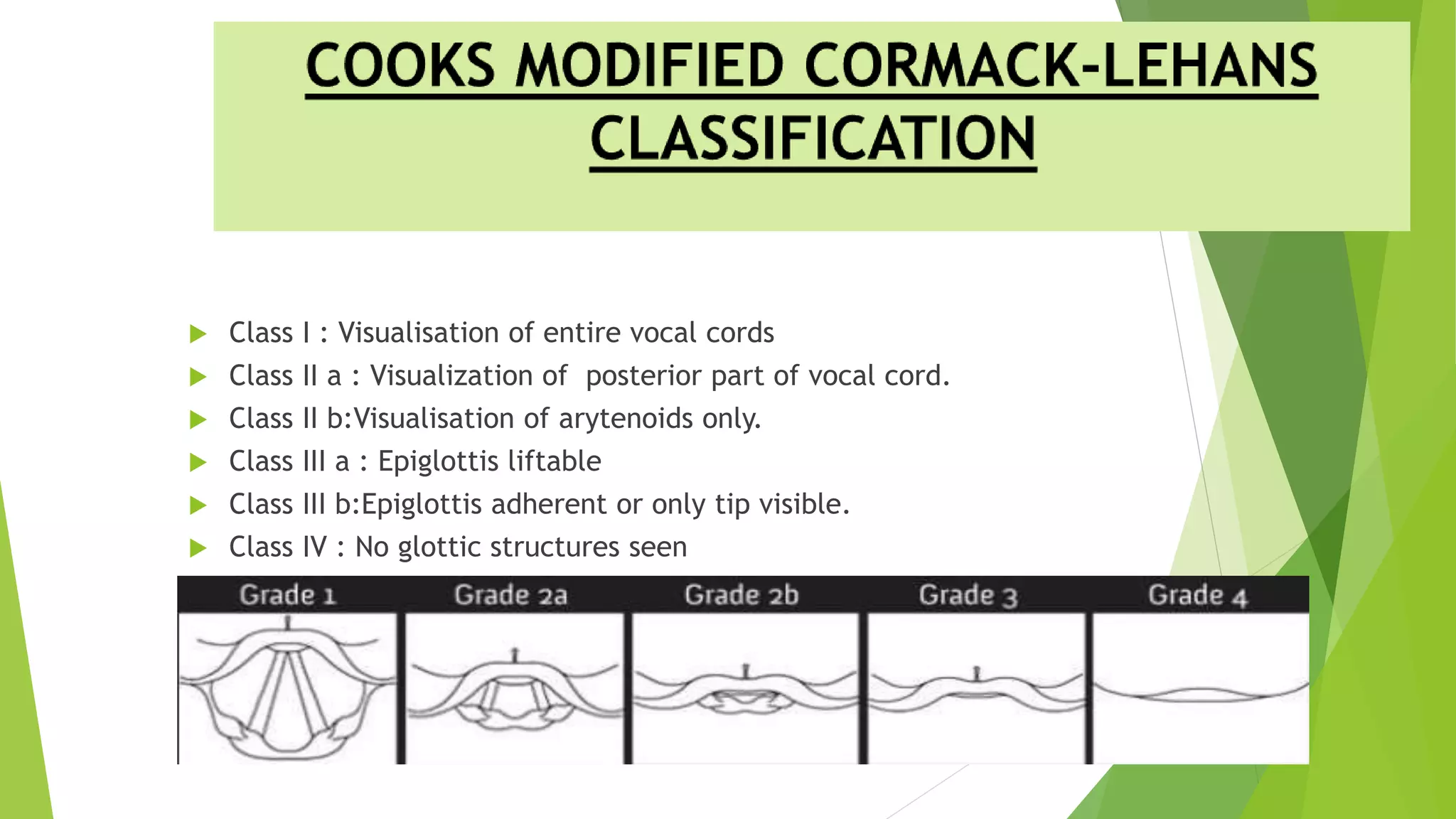
The document discusses difficult airway assessment and management. It defines a difficult airway as situations involving difficult mask ventilation, difficult intubation, difficult placement of a supraglottic airway device, or difficult surgical airway access. It describes predictors of a difficult airway related to patient characteristics and anatomy. It also discusses the importance of assessing the airway and having appropriate equipment and personnel prepared when encountering an anticipated or unanticipated difficult airway.