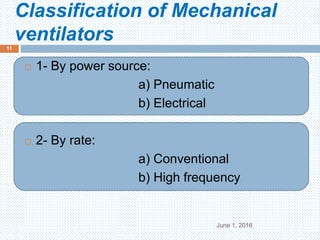
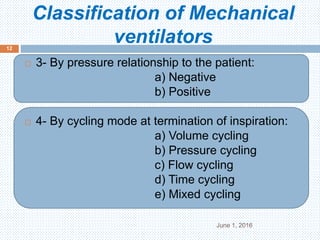
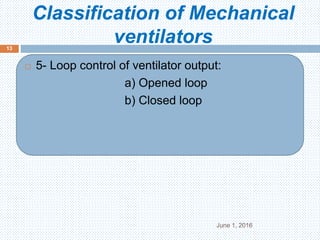
The document provides information on various aspects of mechanical ventilation including:
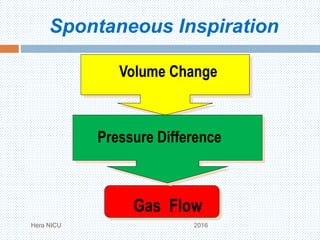
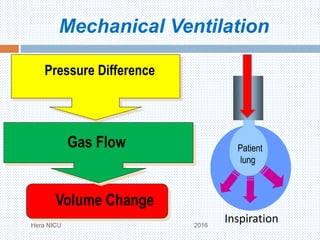
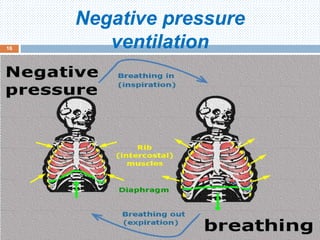
1. It defines mechanical ventilation as the movement of gas in and out of the lungs using an external mechanical device connected to the patient.
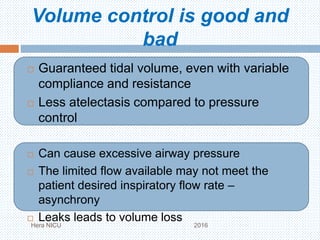
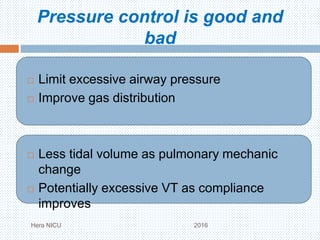
2. It discusses the various purposes of mechanical ventilation including facilitating gas exchange and reducing the work of breathing.
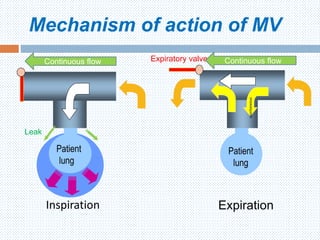
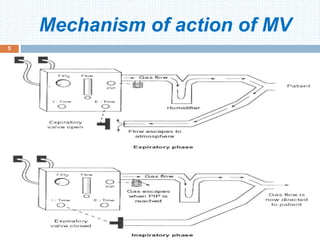
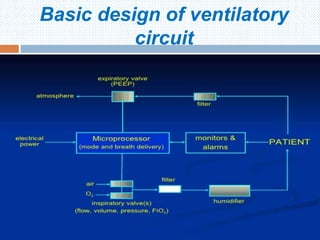
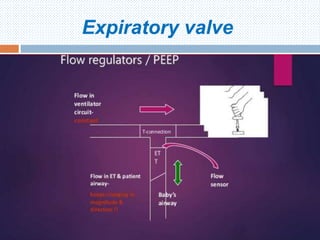
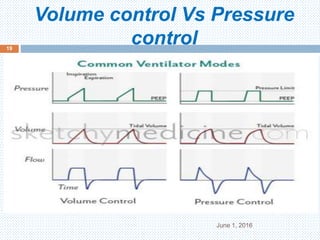
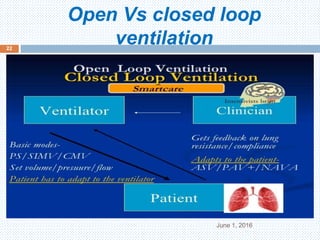
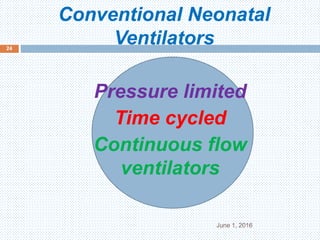
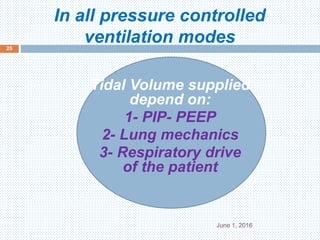
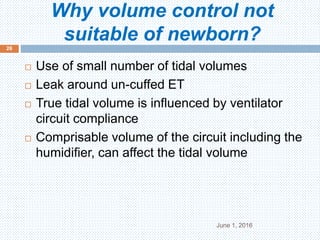
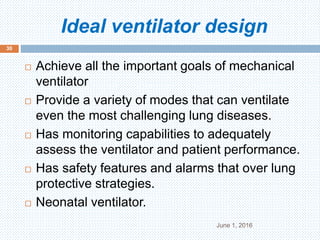
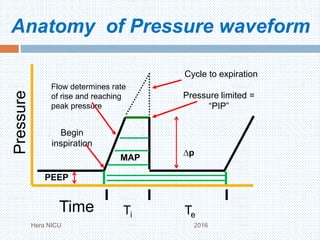
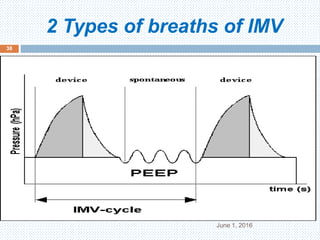
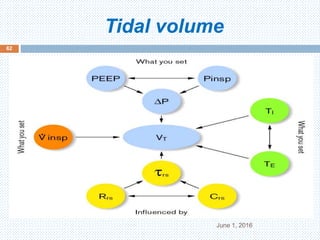
3. It describes the basic mechanisms and components involved in mechanical ventilation including the ventilator circuitry and expiratory valves.
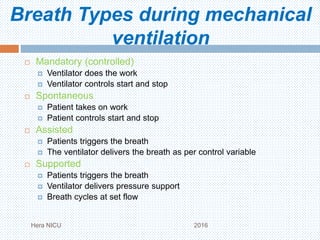
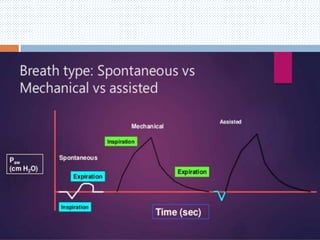
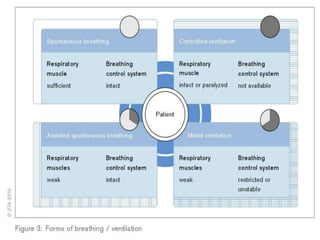
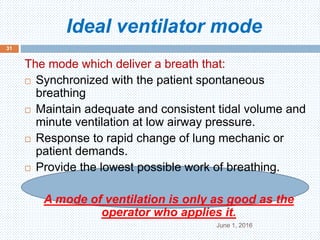
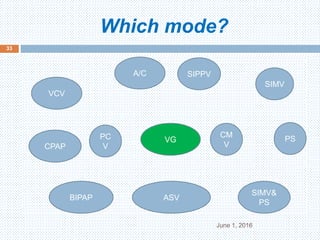
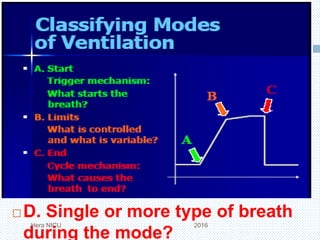
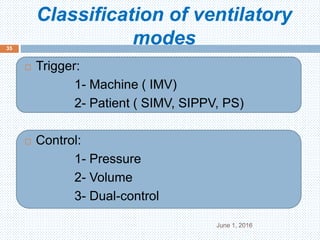
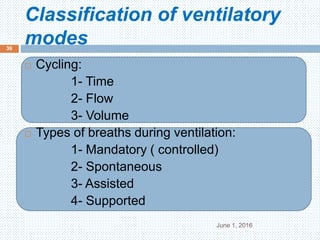
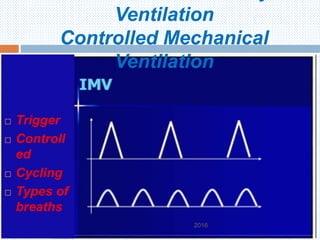
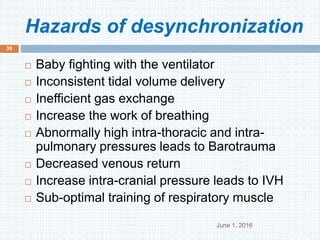
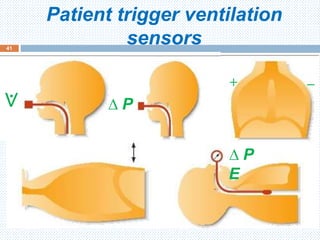
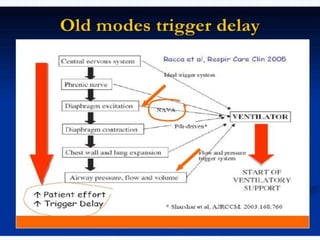
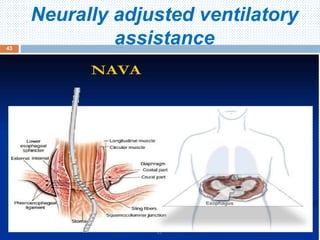
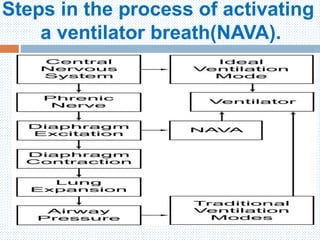
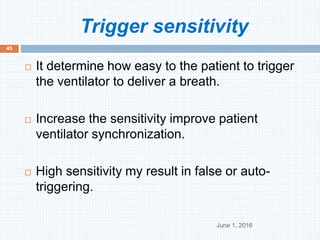
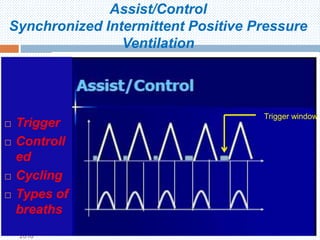
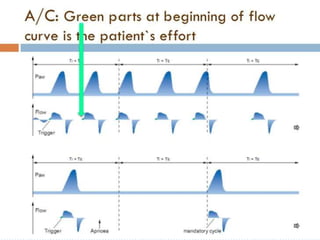
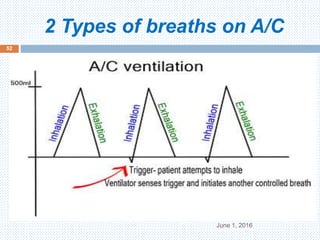
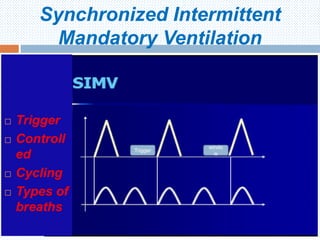
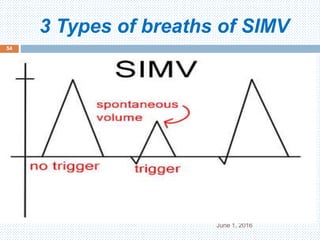
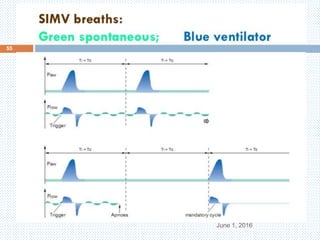
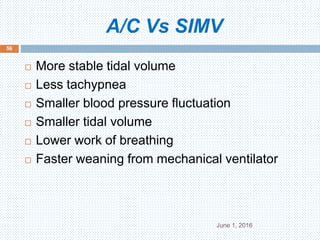
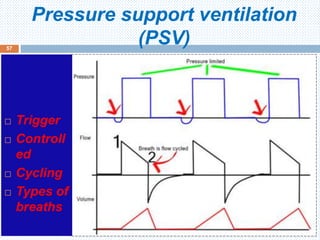
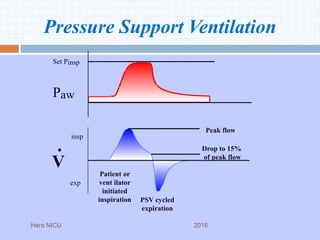
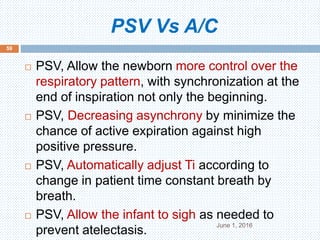
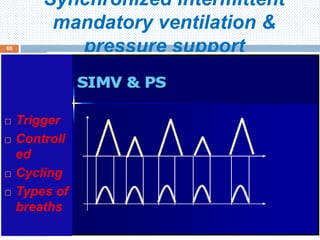
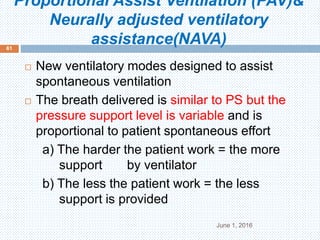
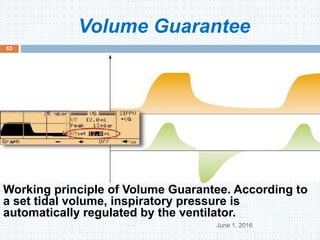
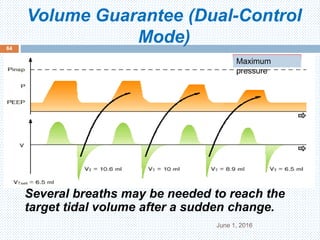
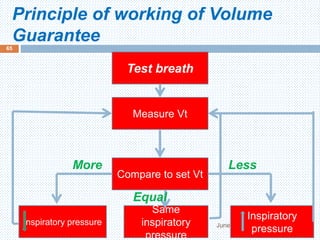
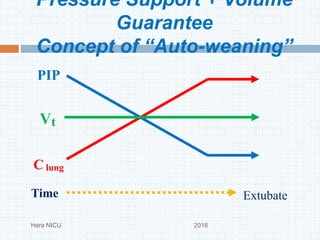
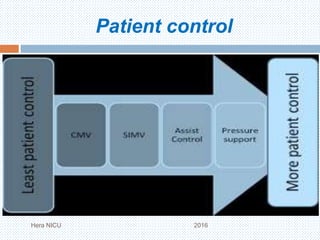
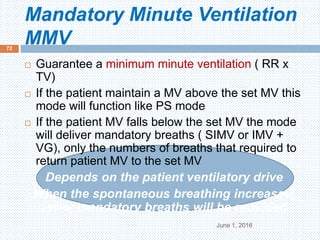
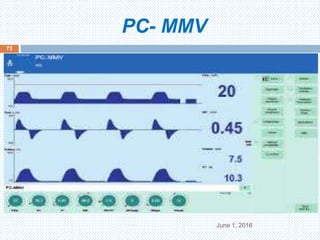
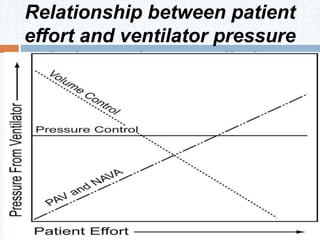
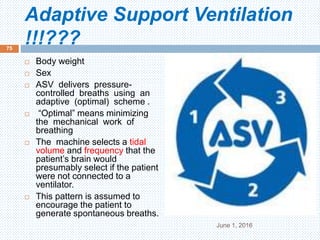
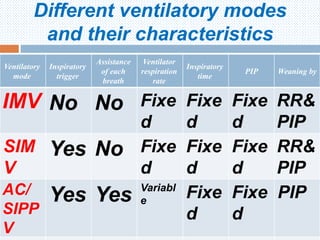
4. It covers the different modes of ventilation including controlled mandatory ventilation, assisted/controlled modes, and pressure support ventilation. It discusses the importance of patient-ventilator synchrony.