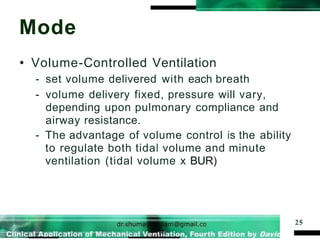
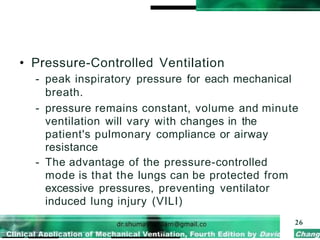
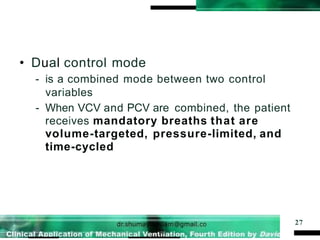
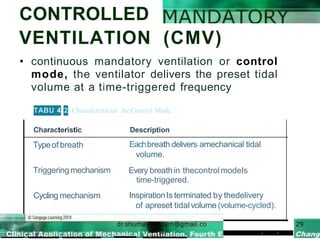
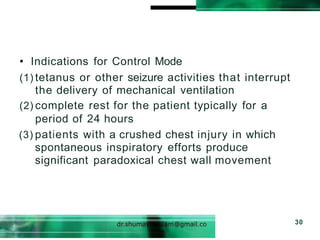
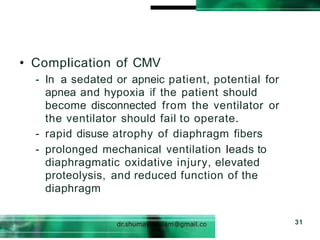
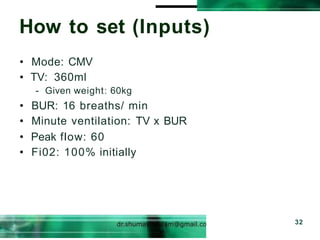
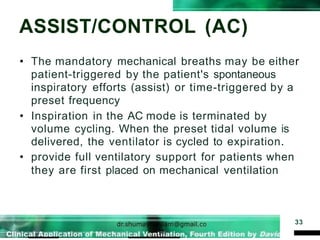
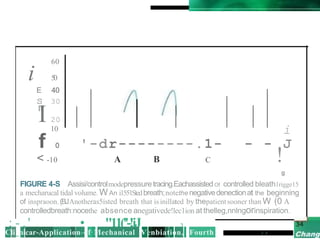
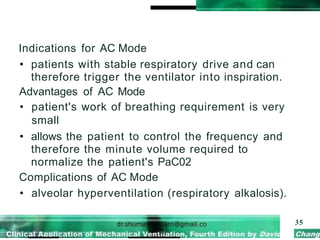
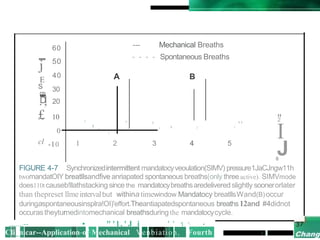
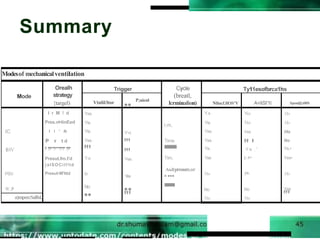
This document discusses the basic modes of mechanical ventilation. It describes the following modes: controlled mandatory ventilation (CMV), assist/control (AC), and synchronized intermittent mandatory ventilation (SIMV). CMV provides continuous mandatory breaths, while AC provides both patient-triggered and time-triggered mandatory breaths. SIMV delivers mandatory breaths synchronized with spontaneous breathing to avoid breath stacking. The modes are used to provide different levels of ventilatory support and to facilitate weaning from the ventilator. Complications include respiratory muscle atrophy with prolonged CMV and rapid weaning failure with SIMV.

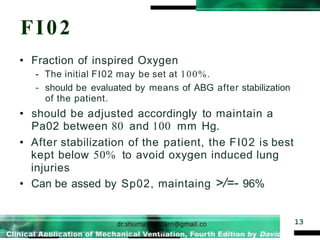
![Desired Fi02
14
If Age< 60, PO2 =104-age x 0.43
If Age >60, PO2 =80-(age-60)
Pao2 = (713 x Fio2)- Pco2/0.8
A2a2= PAo2/Pao2
Desired Fio2=
[(pO2/A2a2+pCO2/0.8)/713]x100%](https://image.slidesharecdn.com/5f292b2c1f71d3ed58db0d85befc65dc-230217085122-d58f887d/85/5f292b2c1f71d3ed58db0d85befc65dc-pptx-13-320.jpg)