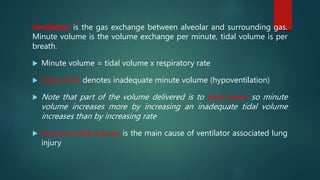
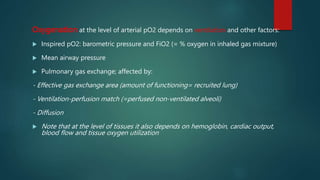
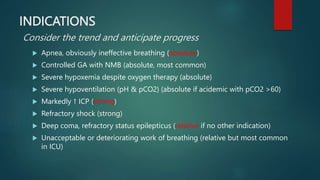
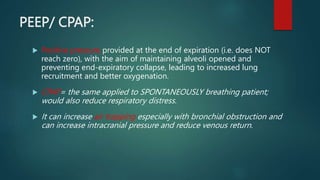
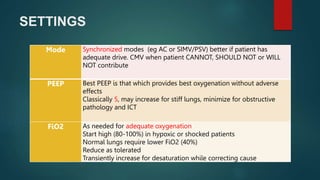
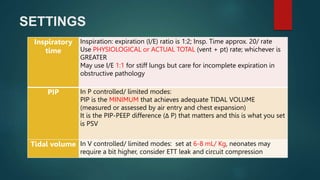
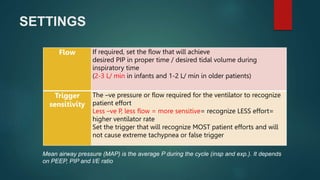
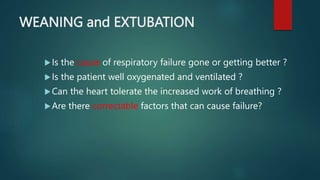
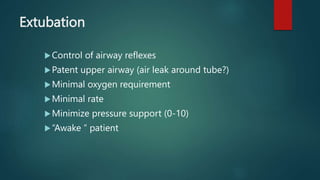
The document provides an introduction to basic mechanical ventilation. It discusses the objectives of mechanical ventilation as achieving appropriate ventilation, oxygenation, work of breathing, and lung protection through the interaction between the patient and ventilator. It describes the basic components of ventilation including tidal volume, minute volume, oxygenation factors, and types of respiratory cycles. Common modes of ventilation like CMV, SIMV, AC, and PSV are explained along with how to set parameters, assess the patient, and manage special cases like stiff or obstructed lungs. Factors in determining readiness for weaning and extubation are also outlined.