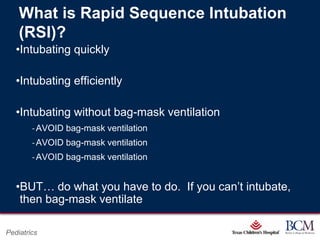
Here are 3 potential interventions for this scenario:
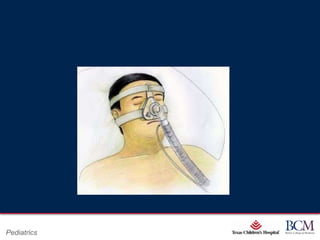
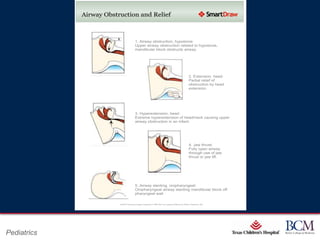
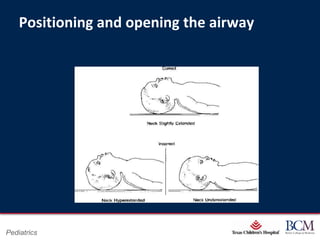
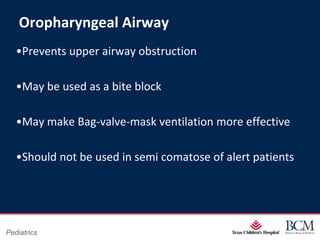
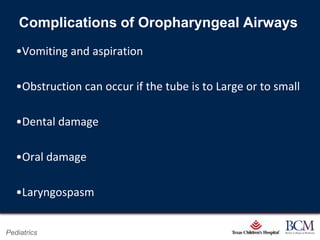
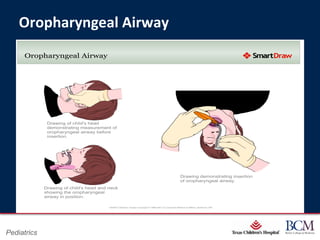
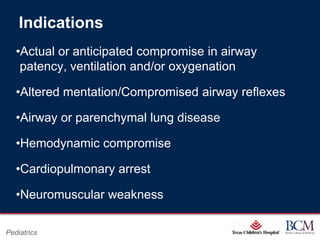
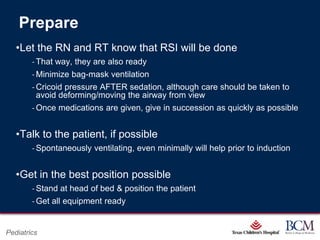
1. Place an appropriately sized oropharyngeal airway to help maintain an open airway and prevent obstruction. Monitor for signs of airway irritation or vomiting.
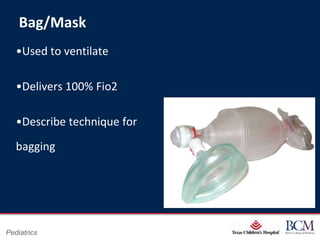
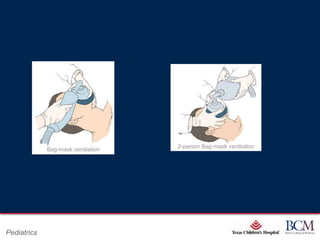
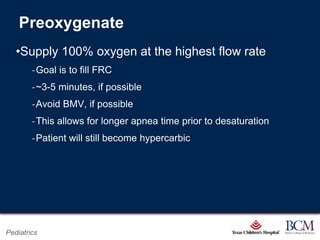
2. Use a bag-valve-mask to manually ventilate the patient with 100% oxygen while maintaining an open airway. Ensure proper mask seal and rate/volume of ventilation.
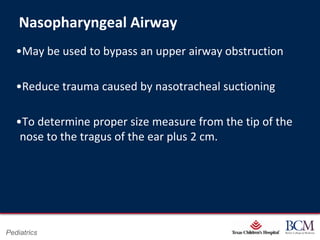
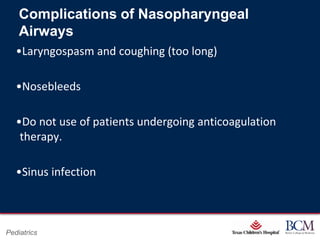
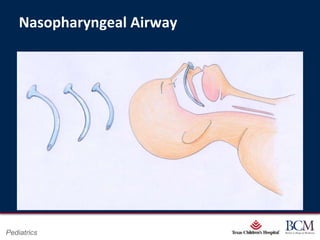
3. Consider placing a nasopharyngeal airway as an alternative to an oropharyngeal airway if the patient is at risk of vomiting. Monitor for signs of irritation, bleeding, or obstruction.