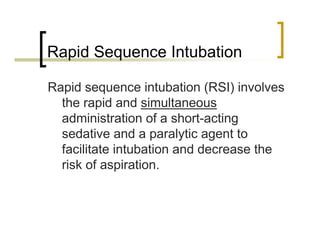
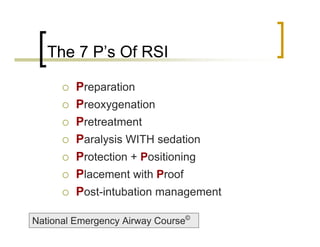
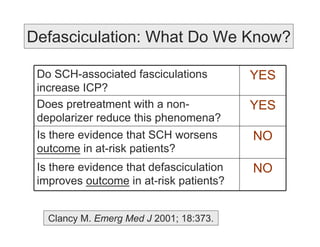
This document provides an overview of rapid sequence intubation (RSI) drugs and techniques. It discusses the "7 P's" approach to RSI, with a focus on pretreatment to reduce reflex sympathetic responses and potential increases in intracranial pressure. A number of induction agents (midazolam, thiopental, propofol, ketamine, etomidate) and paralytics (succinylcholine, rocuronium) are reviewed, noting their hemodynamic and other effects. The risks and benefits of different options are considered depending on the patient's condition, such as risk of adrenal suppression with etomidate in sepsis. Overall it emphasizes selecting drugs carefully based on individual patient


![Pretreatment
The delivery of drugs to reduce the “RSRL”
[Reflex sympathetic response to
laryngoscopy]
National Emergency Airway Course©](https://image.slidesharecdn.com/rsi-091106193808-phpapp02/85/Rsi-6-320.jpg)


![Pretreatment – “LOAD”
Lidocaine 1.0 mg/kg
Opiates 3-5 µg/kg
Atropine 0.02 mg/kg
Defasculation [eg: vecuronium] 0.01 mg/kg
National Emergency Airway Course©](https://image.slidesharecdn.com/rsi-091106193808-phpapp02/85/Rsi-9-320.jpg)










![RSI Induction Agents
Midazolam:
Commonly used if etomidate n/a
Little effect on RSRL or ICP
Dose-dependent respiratory depression
& hypotension
Often under-dosed [NEAR mean = 4 mg]
0.1-0.3 mg/kg](https://image.slidesharecdn.com/rsi-091106193808-phpapp02/85/Rsi-21-320.jpg)






![Etomidate In The ED
Prospective study of 522 ED RSI
cases using etomidate.
Outcome measures:
Ease of intubation
Hemodynamics [BPS, BPD, HR] at the
time of intubation, 5 minutes, 15 minutes
Zed PJ. Acad Emerg Med 2006; 13:378-383.](https://image.slidesharecdn.com/rsi-091106193808-phpapp02/85/Rsi-28-320.jpg)


![Adrenal Suppression?
Prospective evaluation of adrenal
function in 31 ED patients receiving
etomidate or midazolam for RSI
Assessed at 4/12/24 hours:
Cosyntropin stimulation test [CST]
Serum cortisol levels
Schernarts C. Academ Emerg Med 2001; 8:1.](https://image.slidesharecdn.com/rsi-091106193808-phpapp02/85/Rsi-31-320.jpg)


![Succinylcholine
Remains the drug of choice for the ED
Intubation level paralysis in 45 sec
Clinical duration 6-8 min
The dark side:
Fatal hyperkalemic risk
Bradycardia [children, 2nd dose]
Malignant hyperthermia](https://image.slidesharecdn.com/rsi-091106193808-phpapp02/85/Rsi-34-320.jpg)

![Fatal Hyperkalemic Risk
Receptor Myopathic Process
Upregulation Muscular dystrophy
Burns, crush Rare idiopathic
Prolonged ICU stay
UMN [eg: stroke]
LMN [eg: SC
injury]
Mortality 11% Mortality 30%
Gronert GA. Anesthesiology 2001; 94:523.](https://image.slidesharecdn.com/rsi-091106193808-phpapp02/85/Rsi-36-320.jpg)



