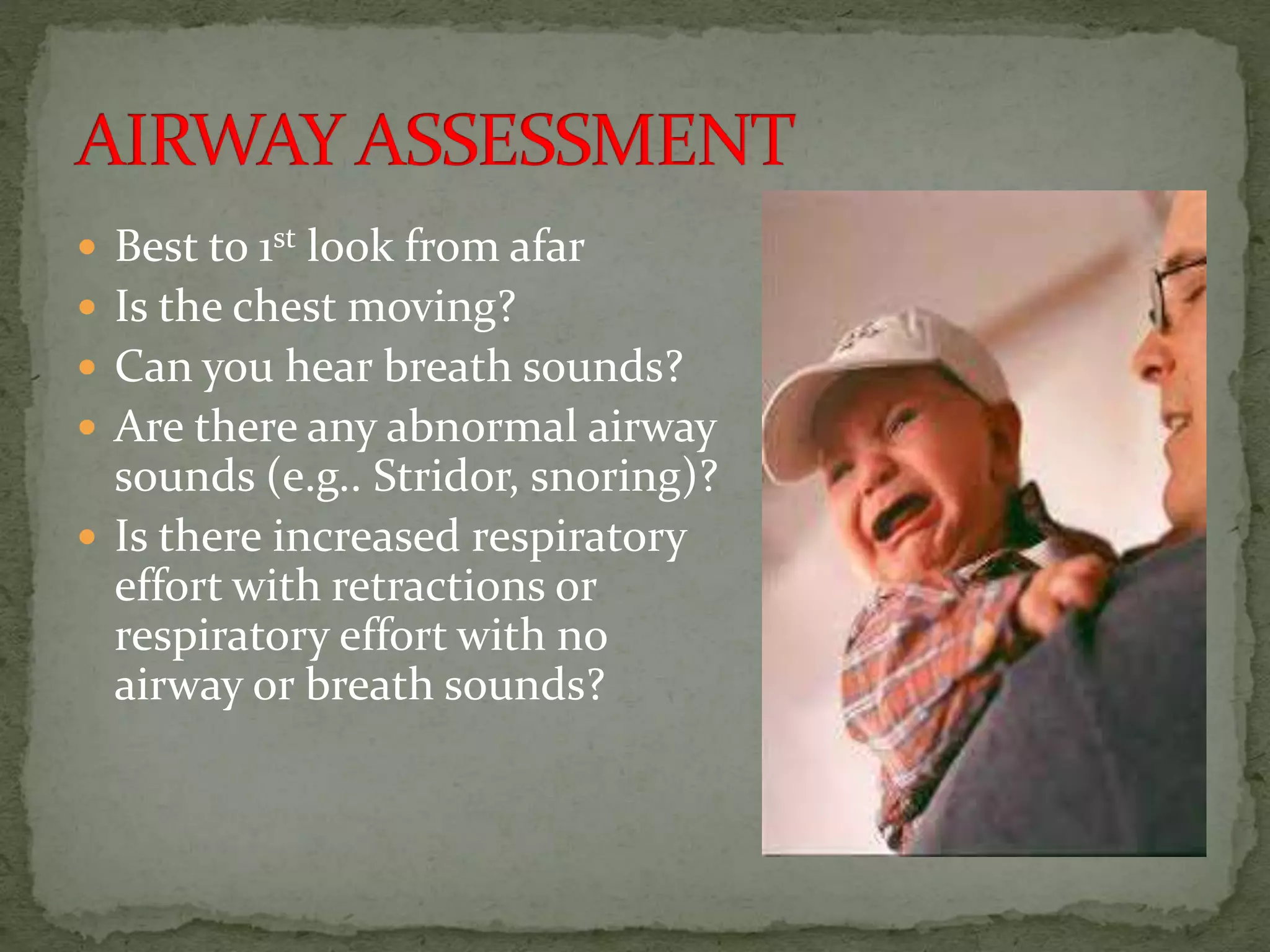
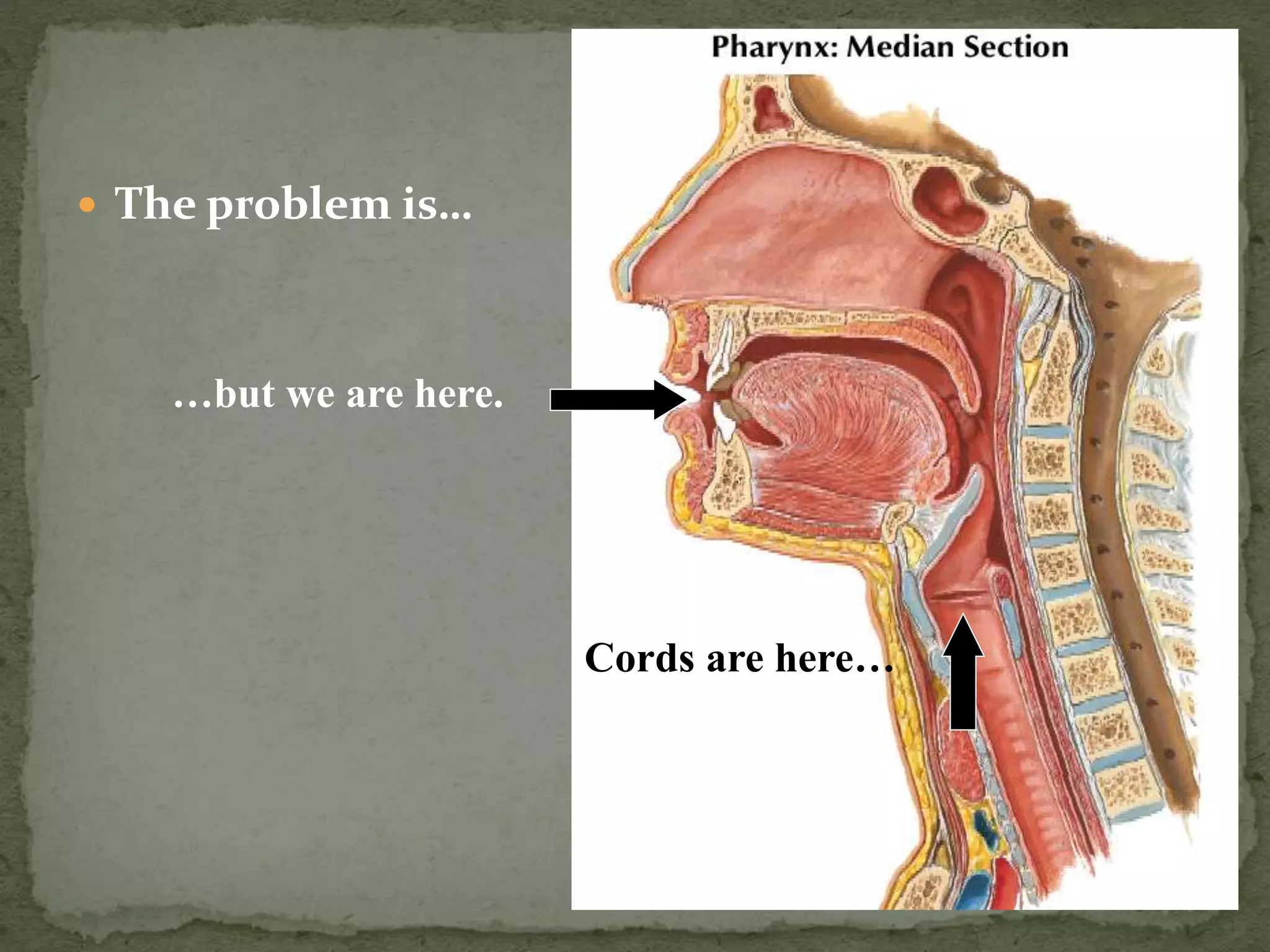
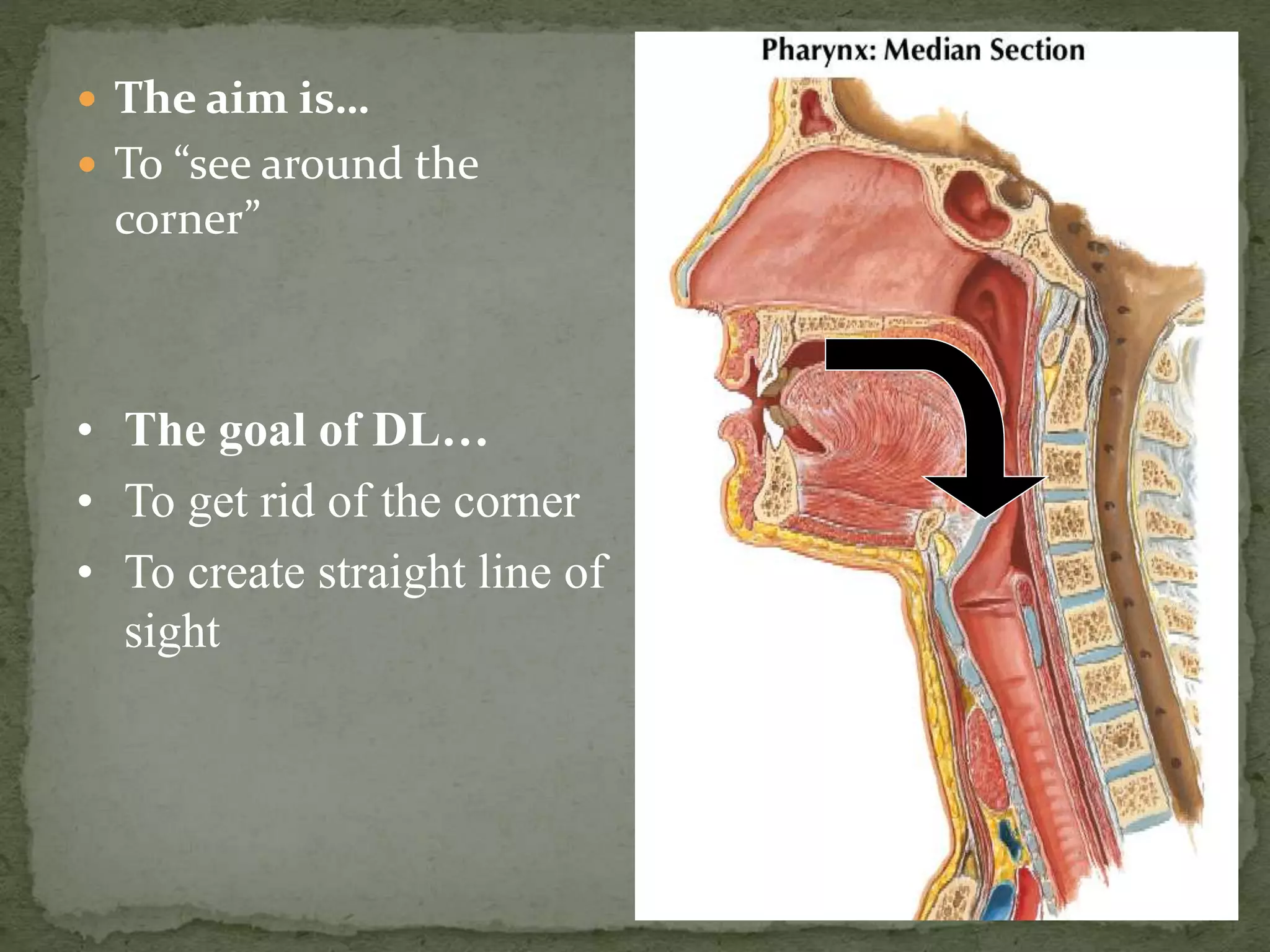
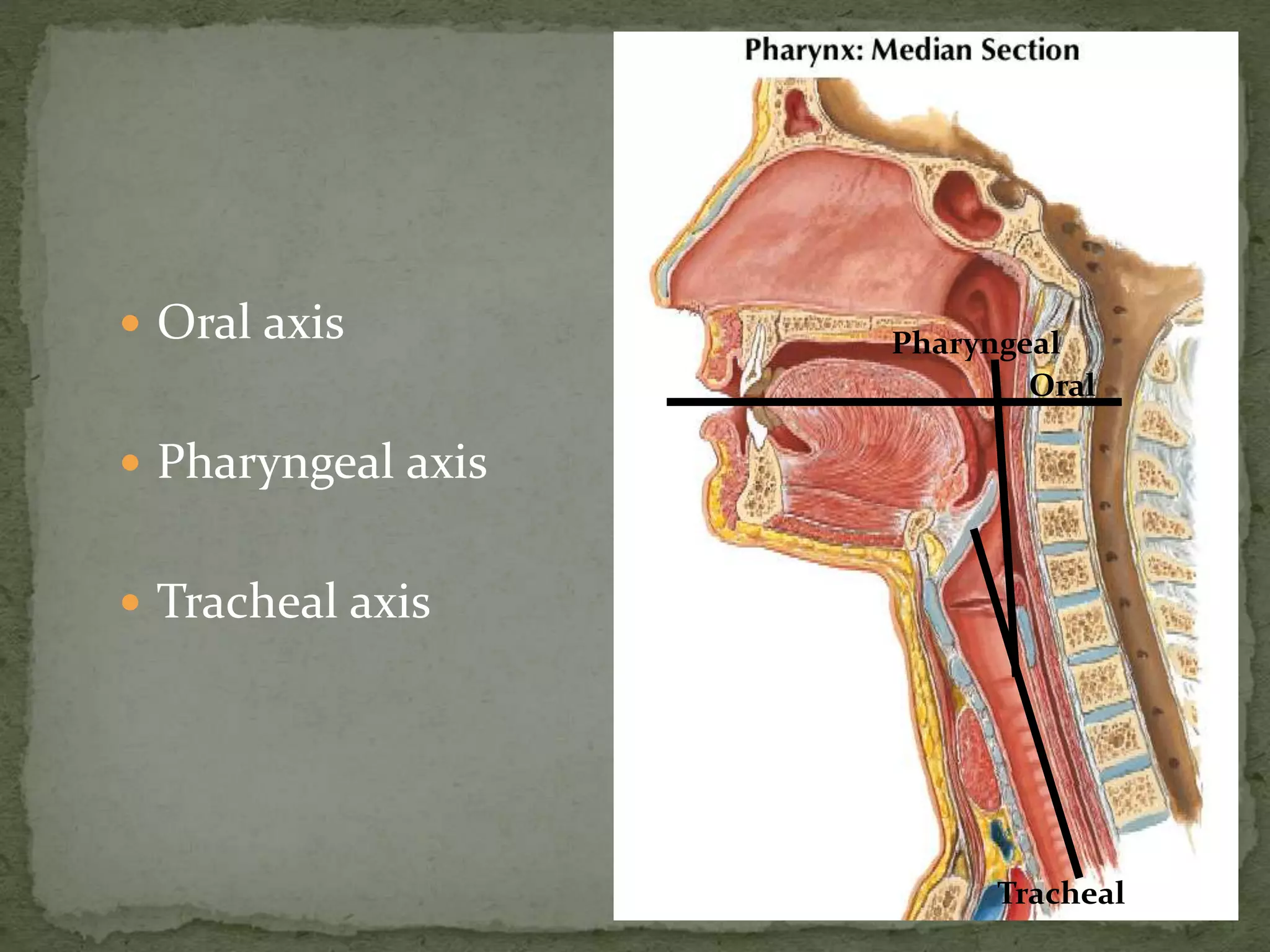
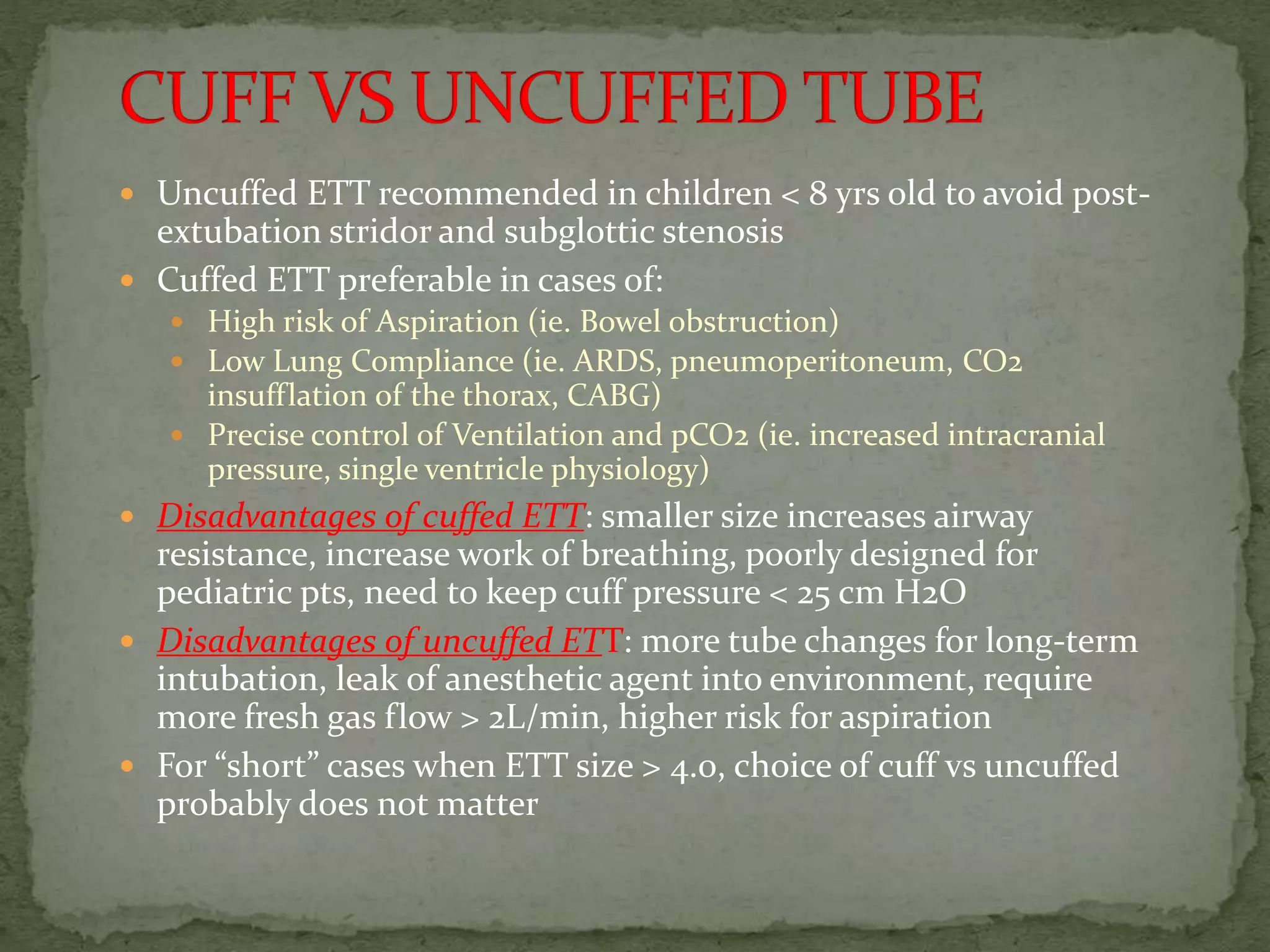
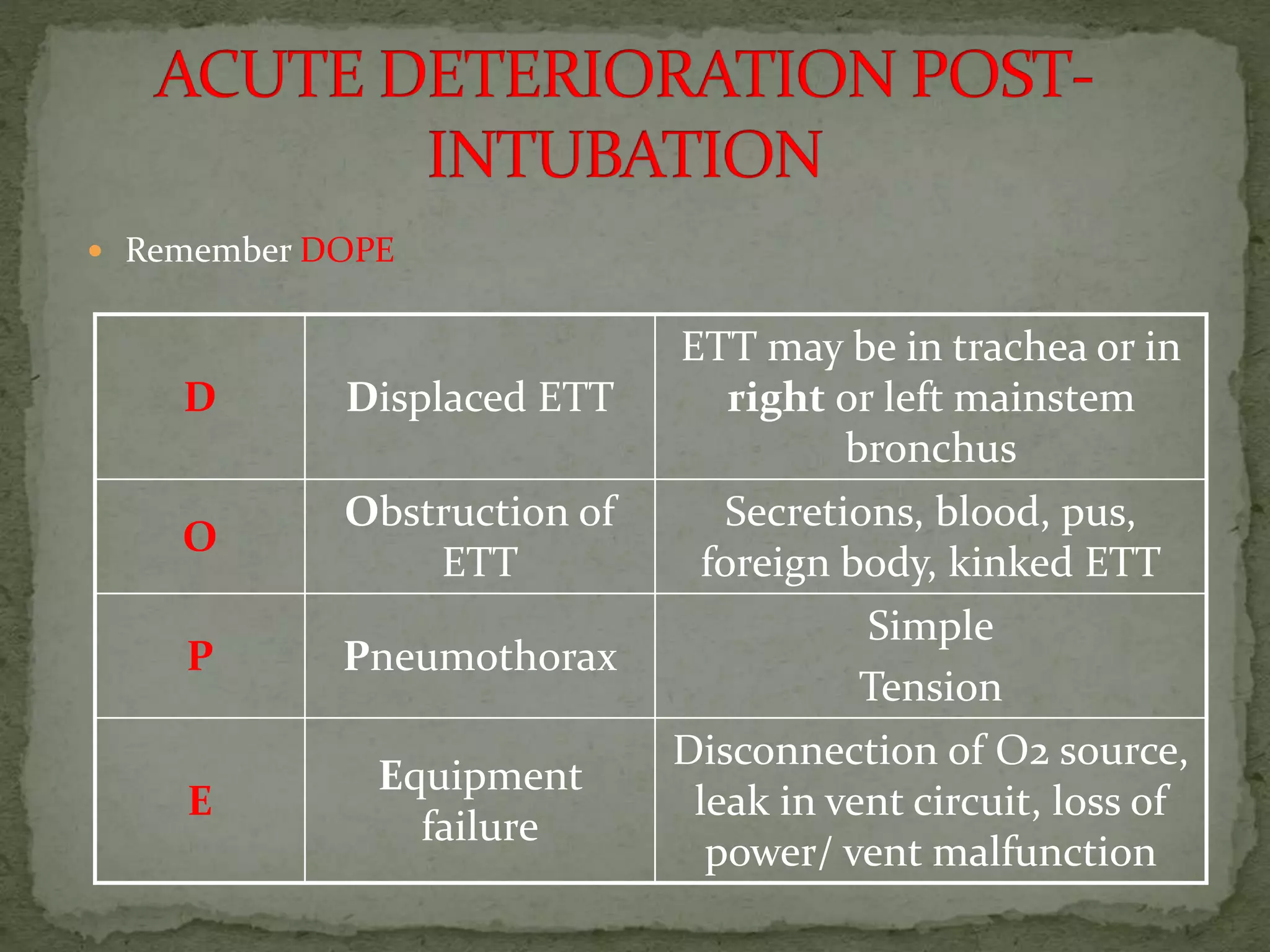
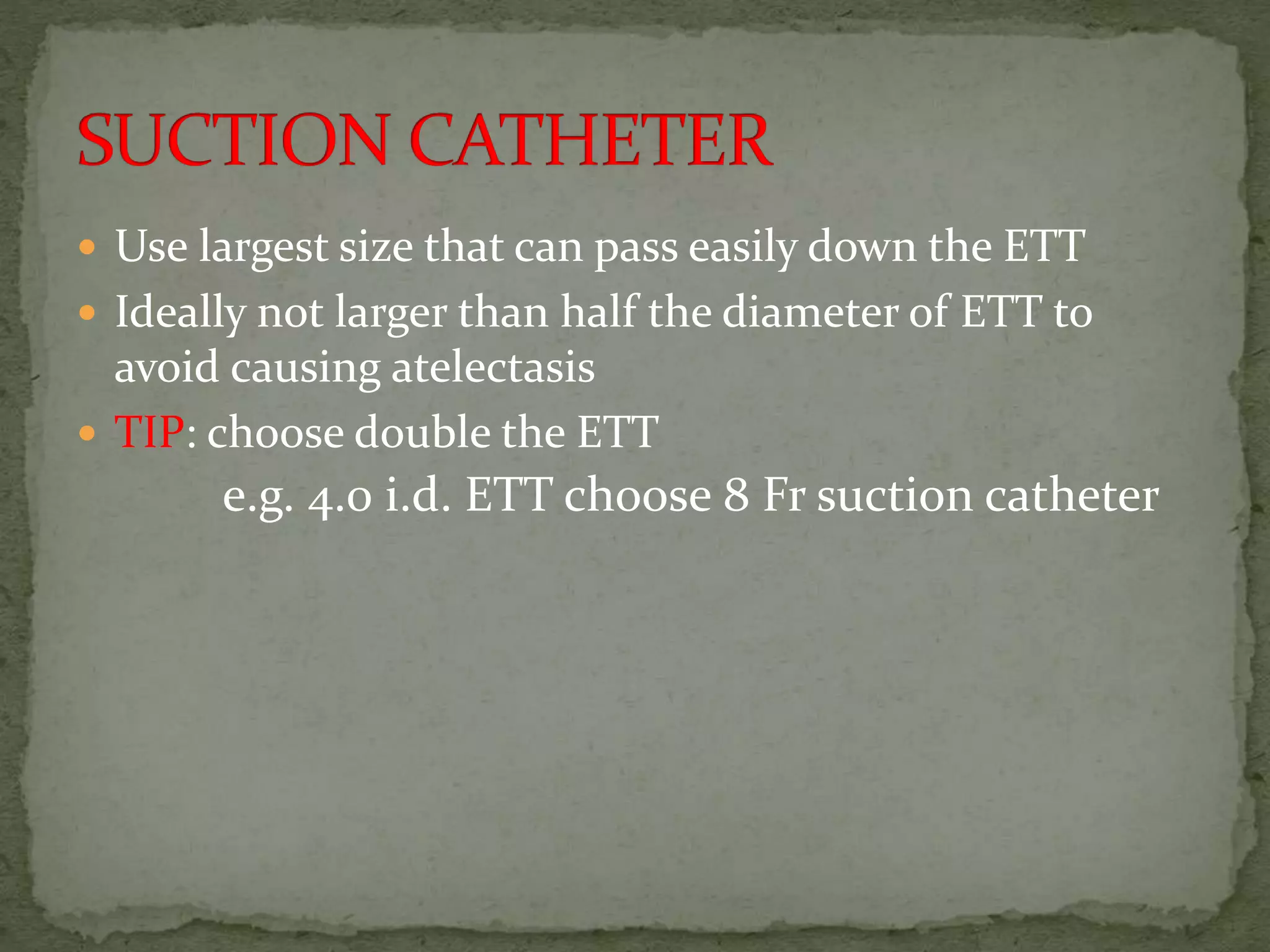
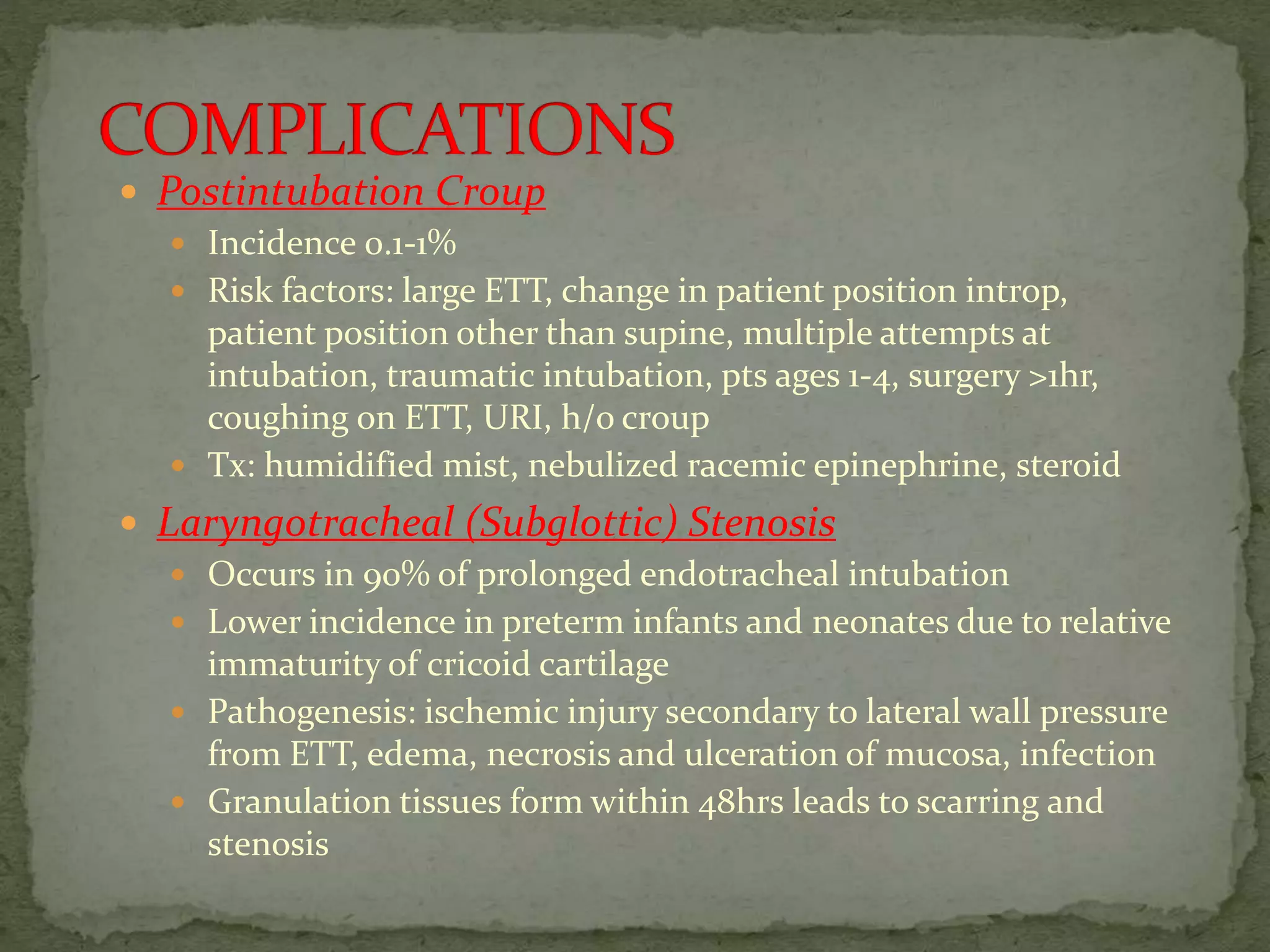
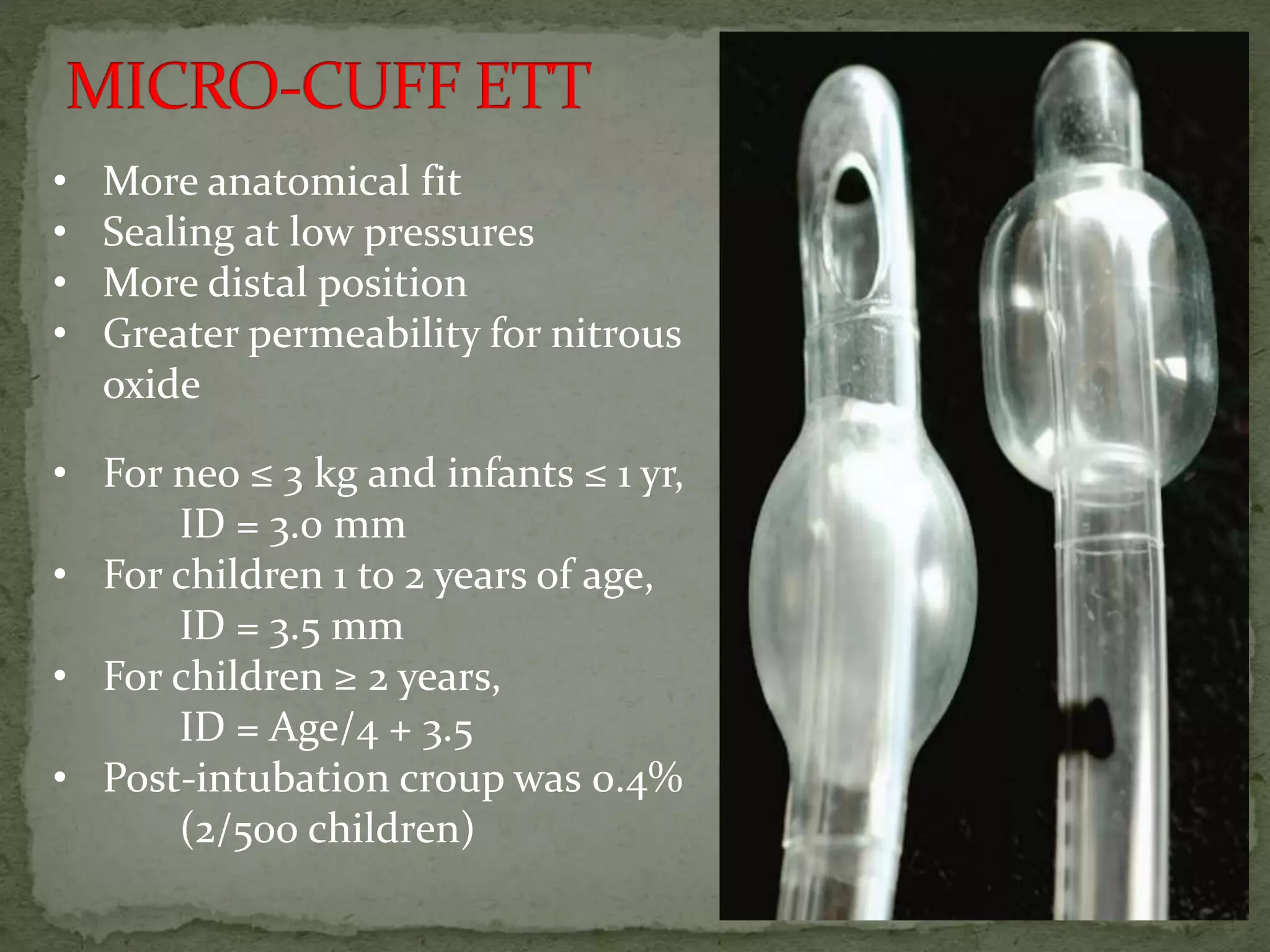
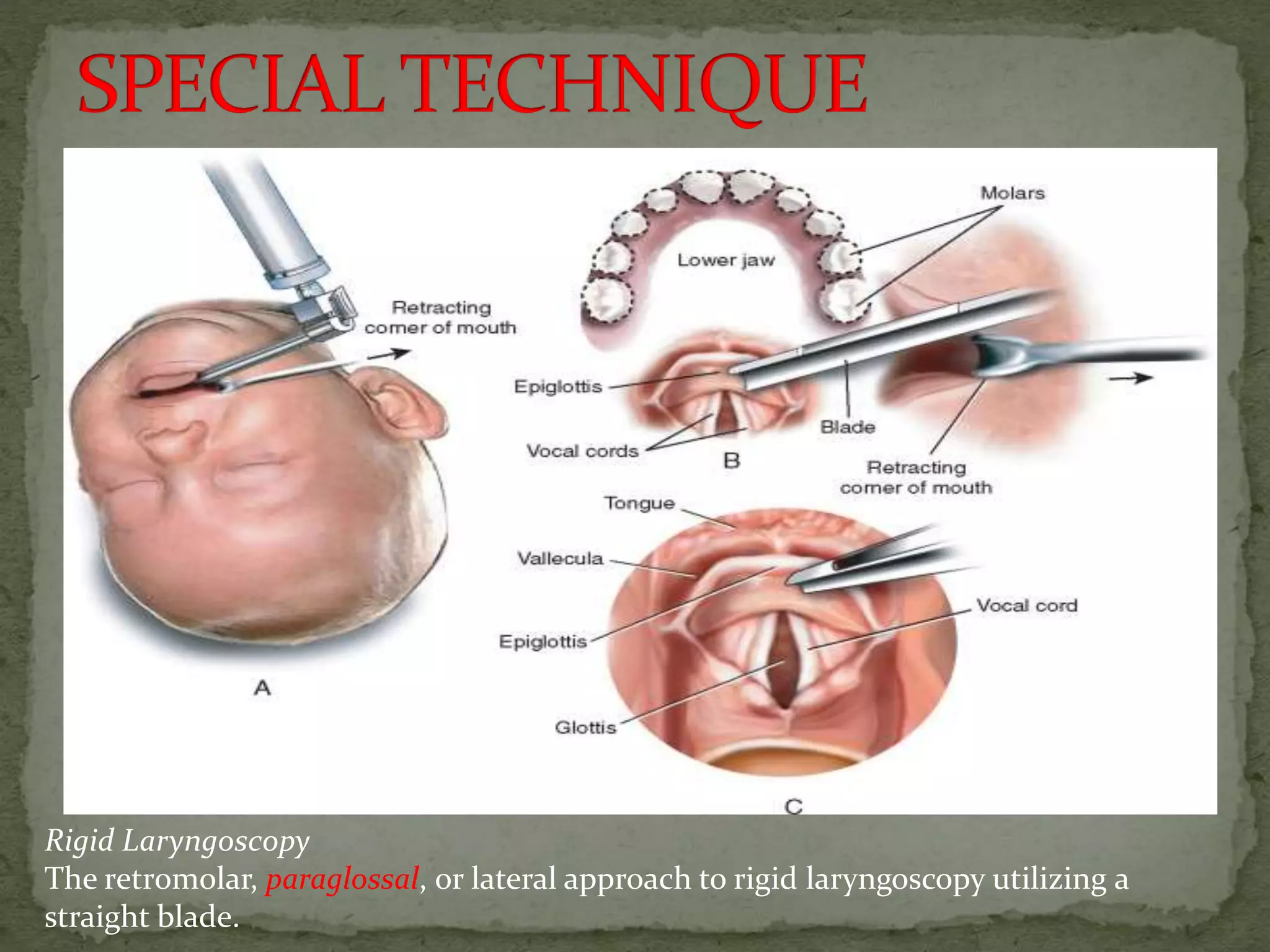
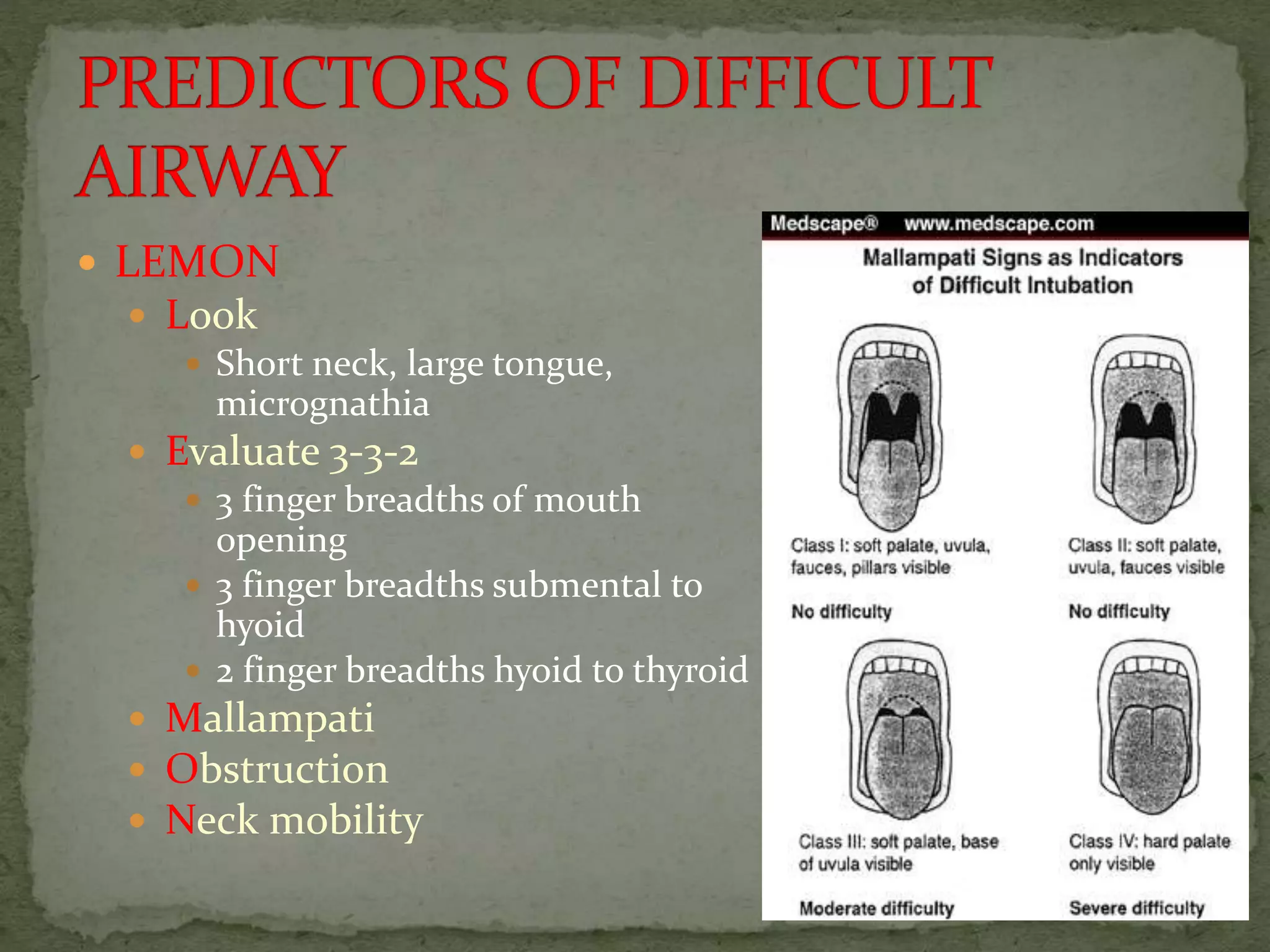
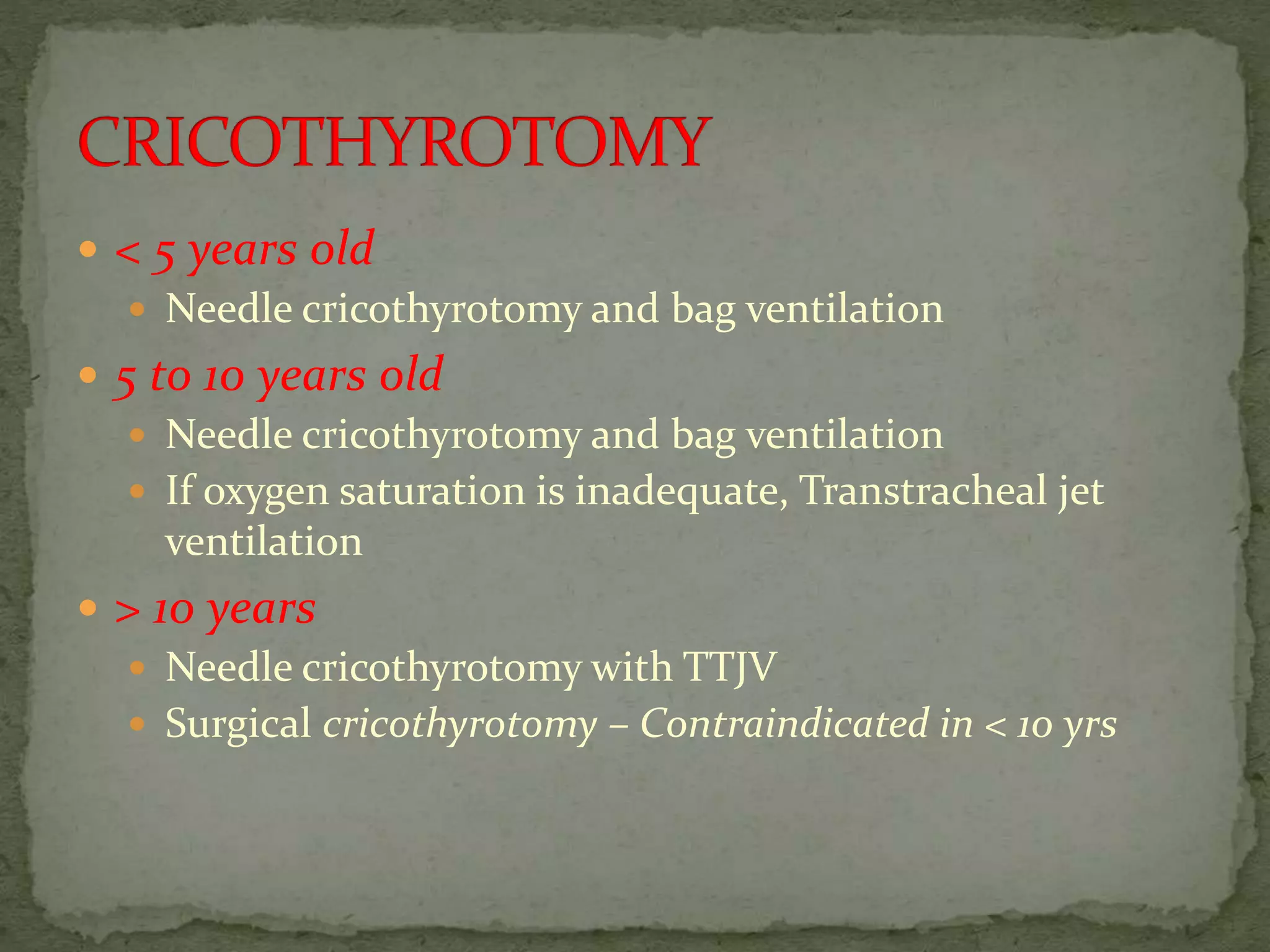
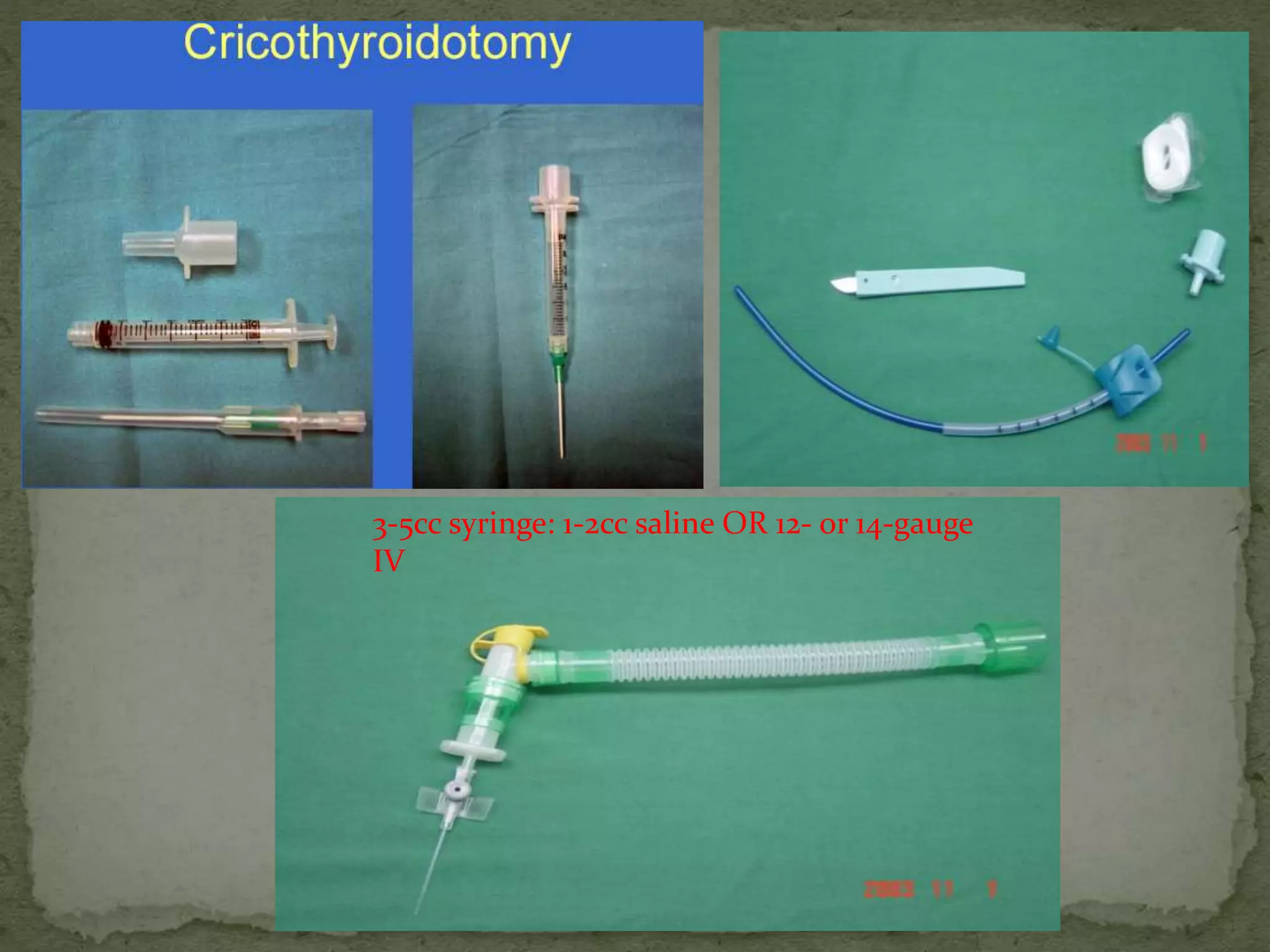
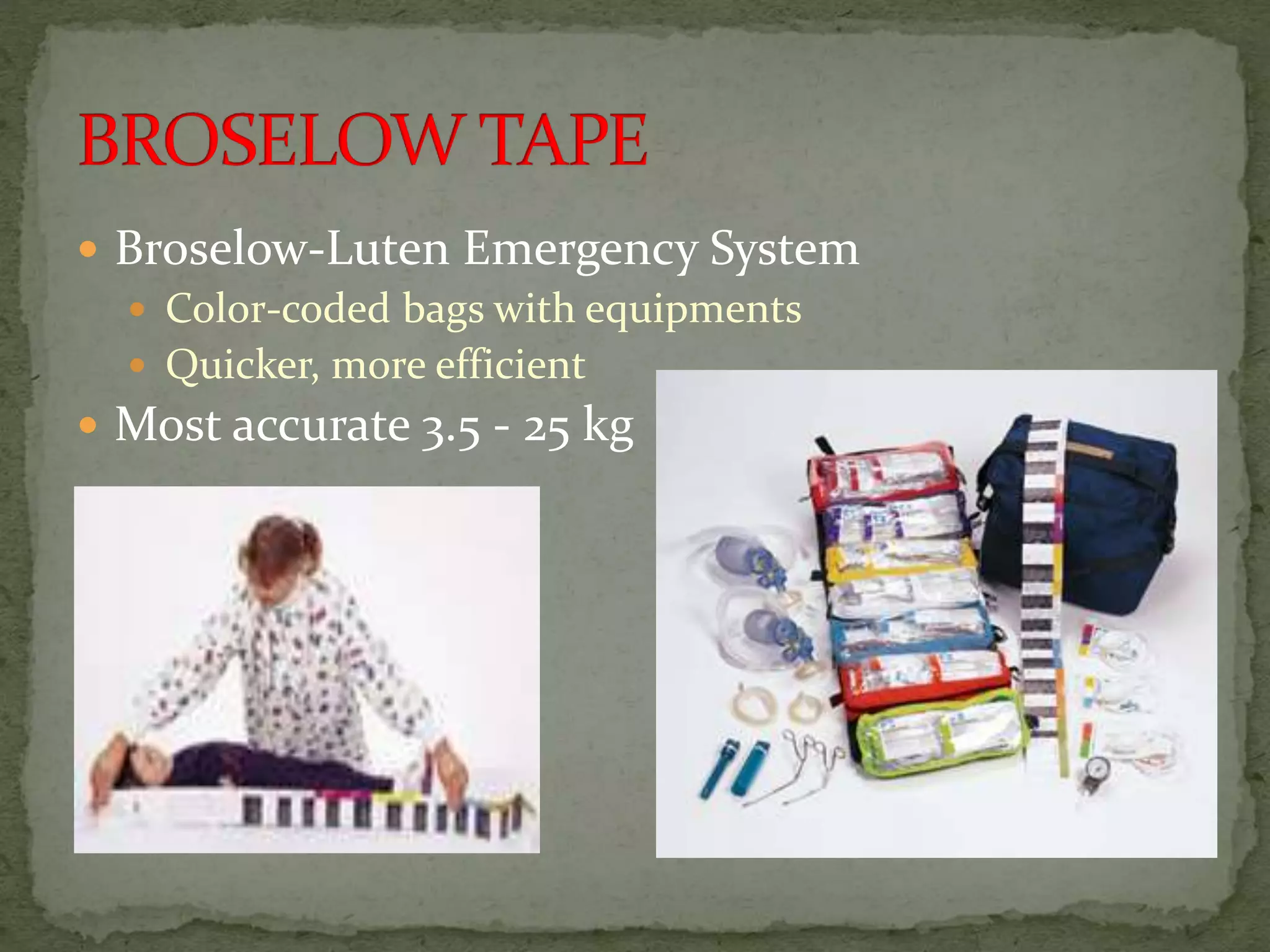
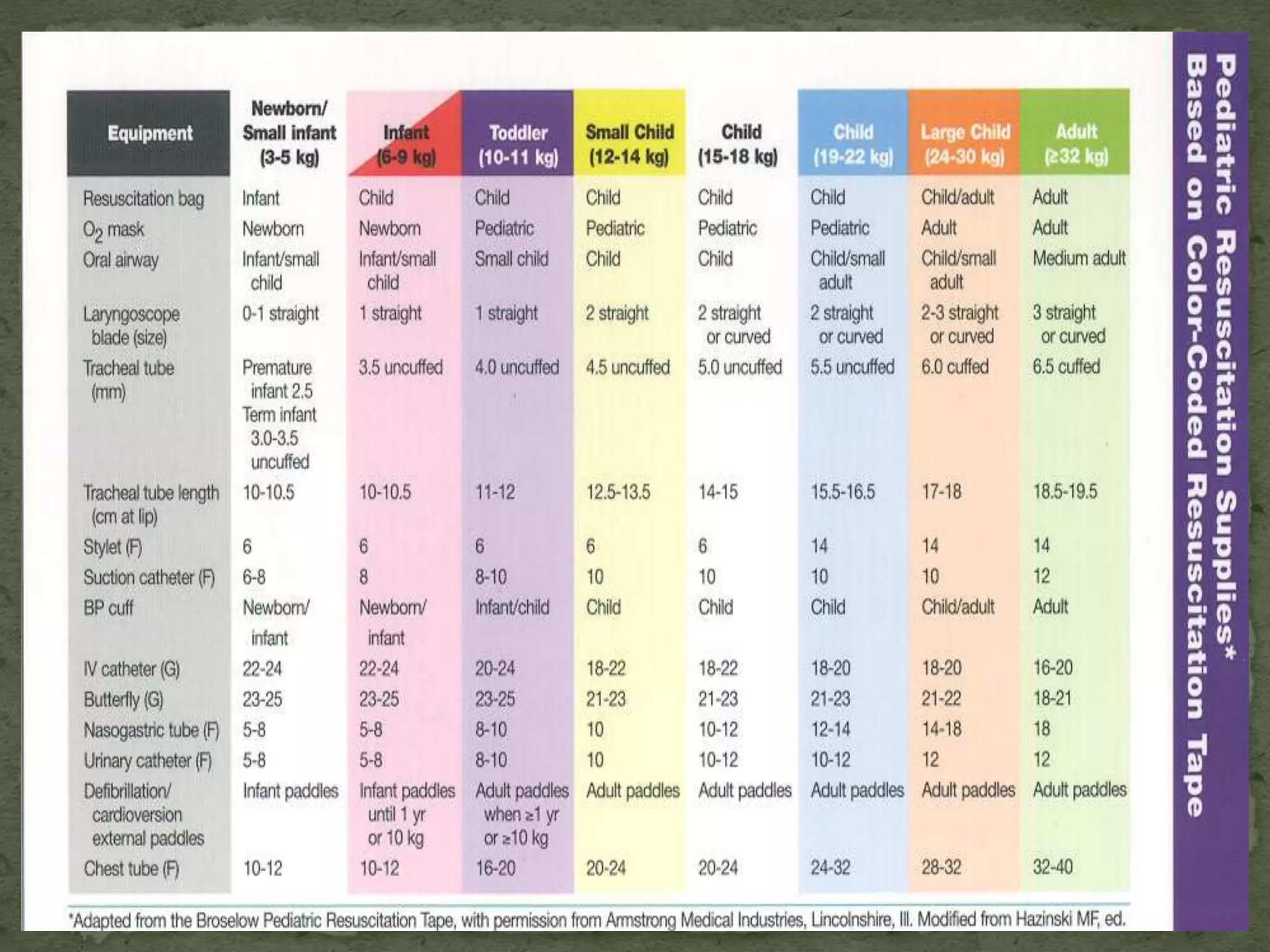
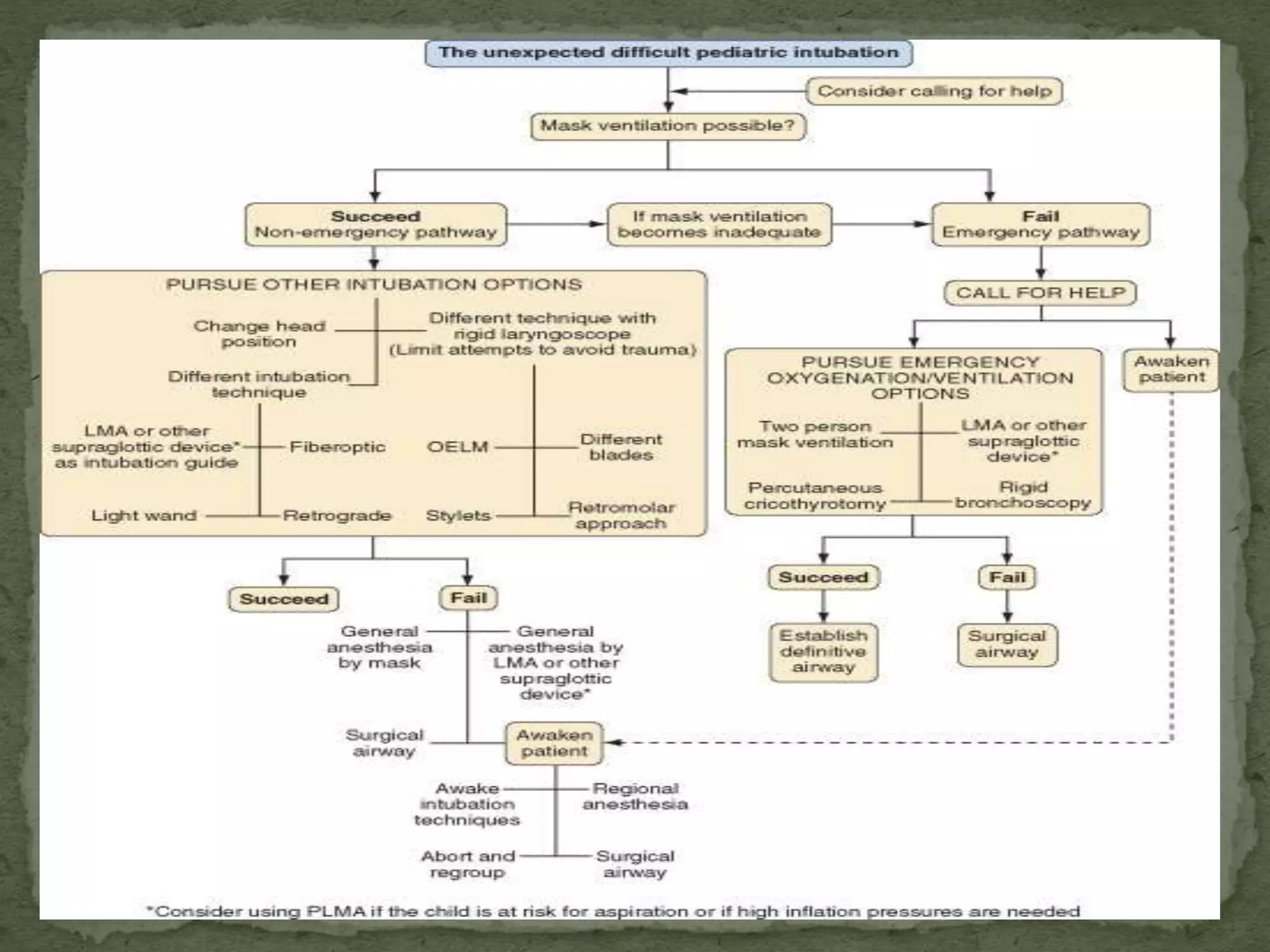
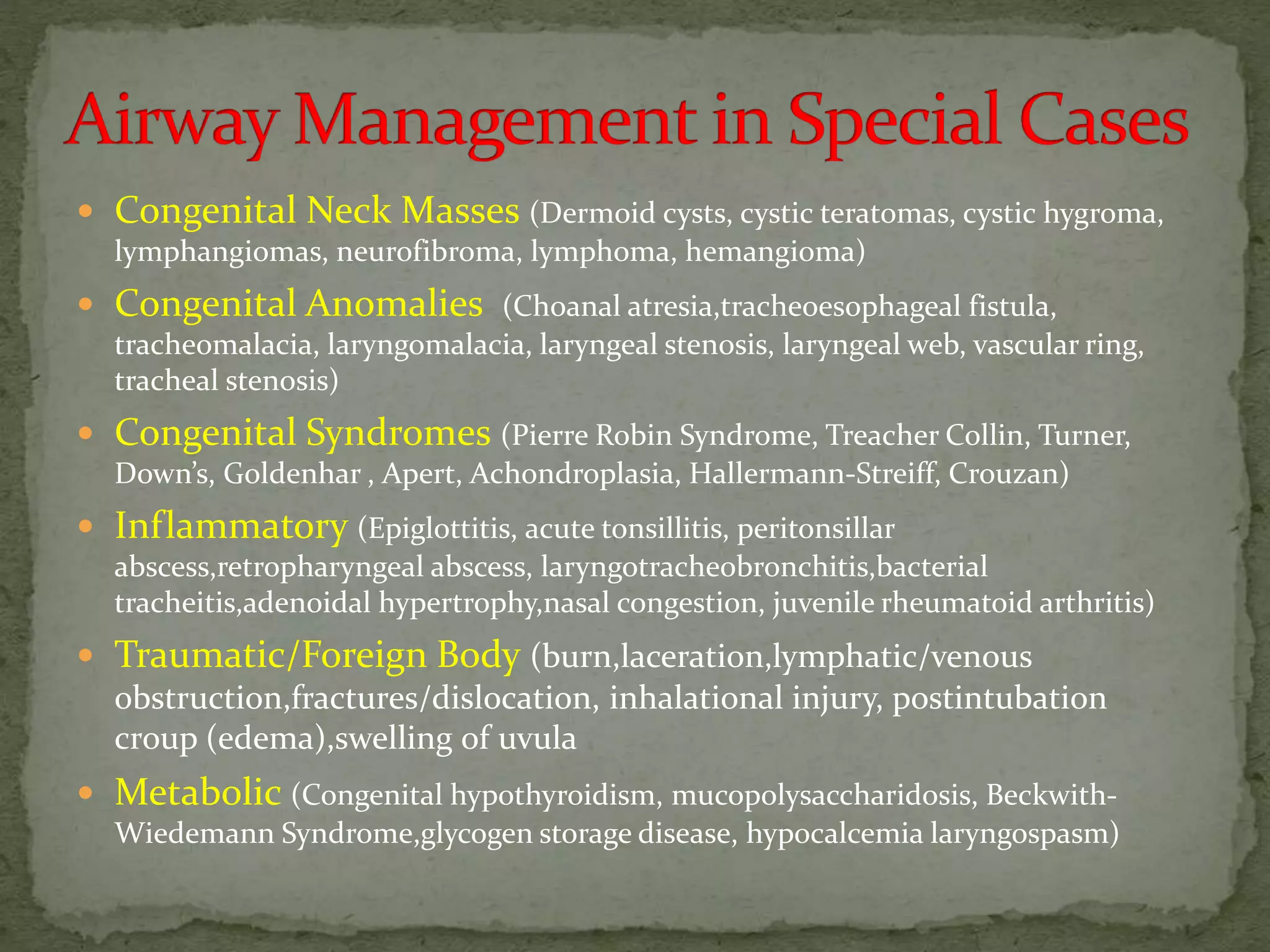
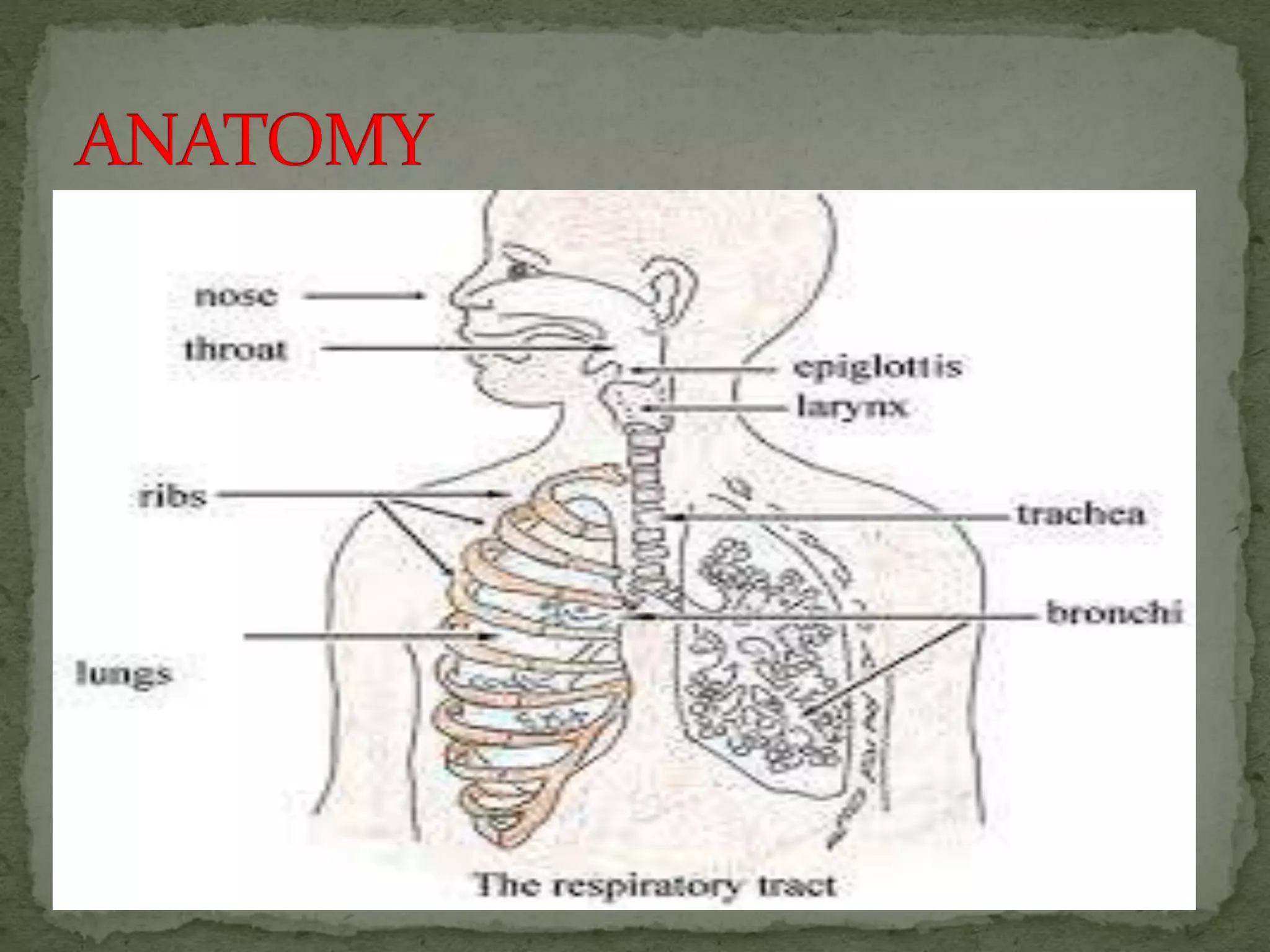
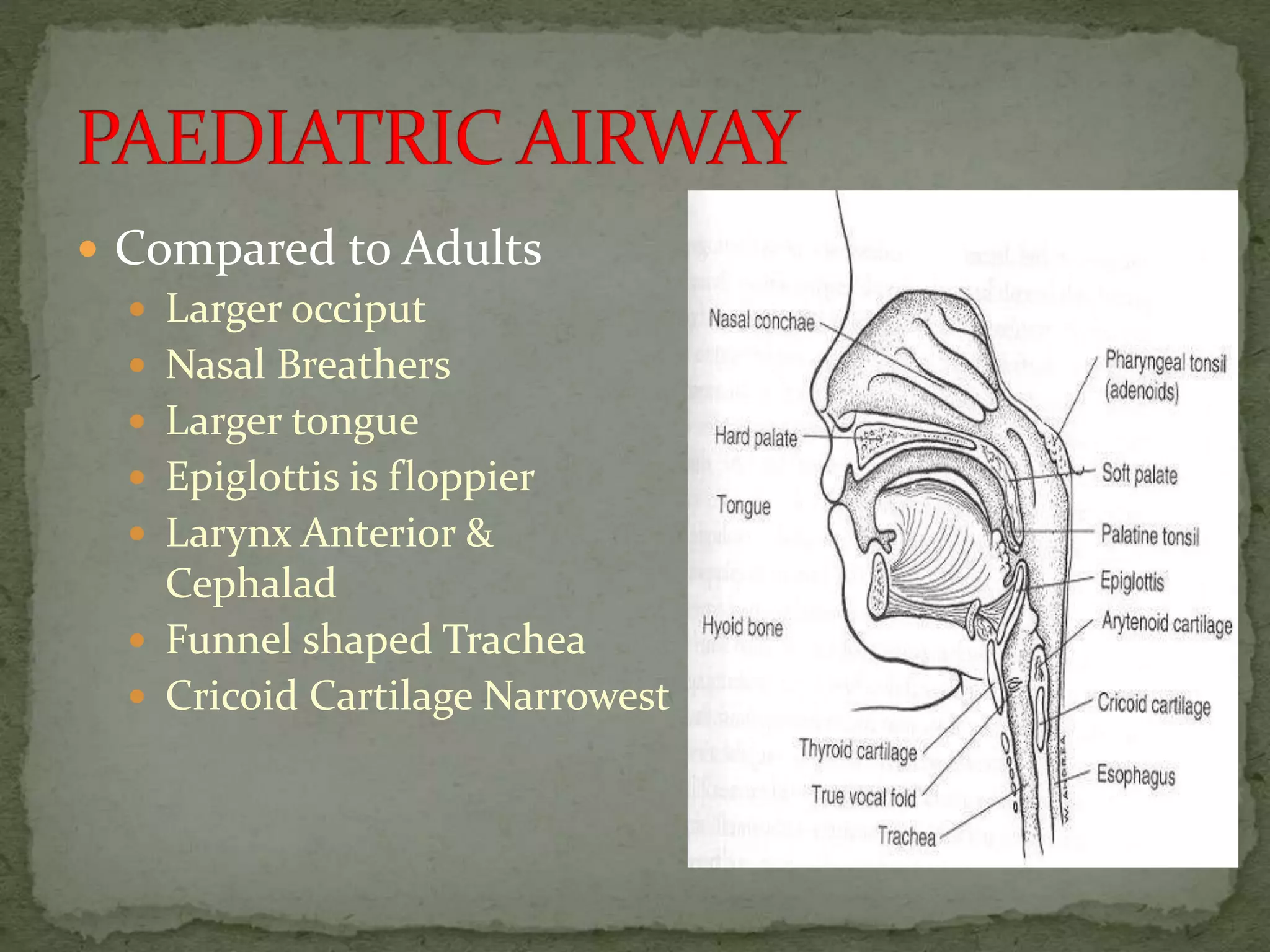
The document provides a comprehensive overview of pediatric airway management, highlighting anatomical differences between adults and infants, challenges in airway assessment and intubation, and various techniques and devices utilized in difficult airway situations. Key considerations include the selection of endotracheal tubes, the importance of appropriate airway adjuncts, and the management of potential complications such as post-intubation croup. It also discusses the physiological differences in infants and their implications for anesthesia and airway management.

![ High metabolic rate (5-8 ml/kg/min)
Oxygen consumption of infant (6 ml/kg/min) is twice that
of an adult (3 ml/kg/min) [Less Oxygen Reserve]
Tidal volume is relatively fixed (6-7 ml/kg/min)
Minute Alveolar Ventilation is more dependent on
increased Respiratory Rate than on Tidal Volume
Ratio of Alveolar Minute Ventilation to FRC is doubled
under circumstances of hypoxia, apnea or anesthesia
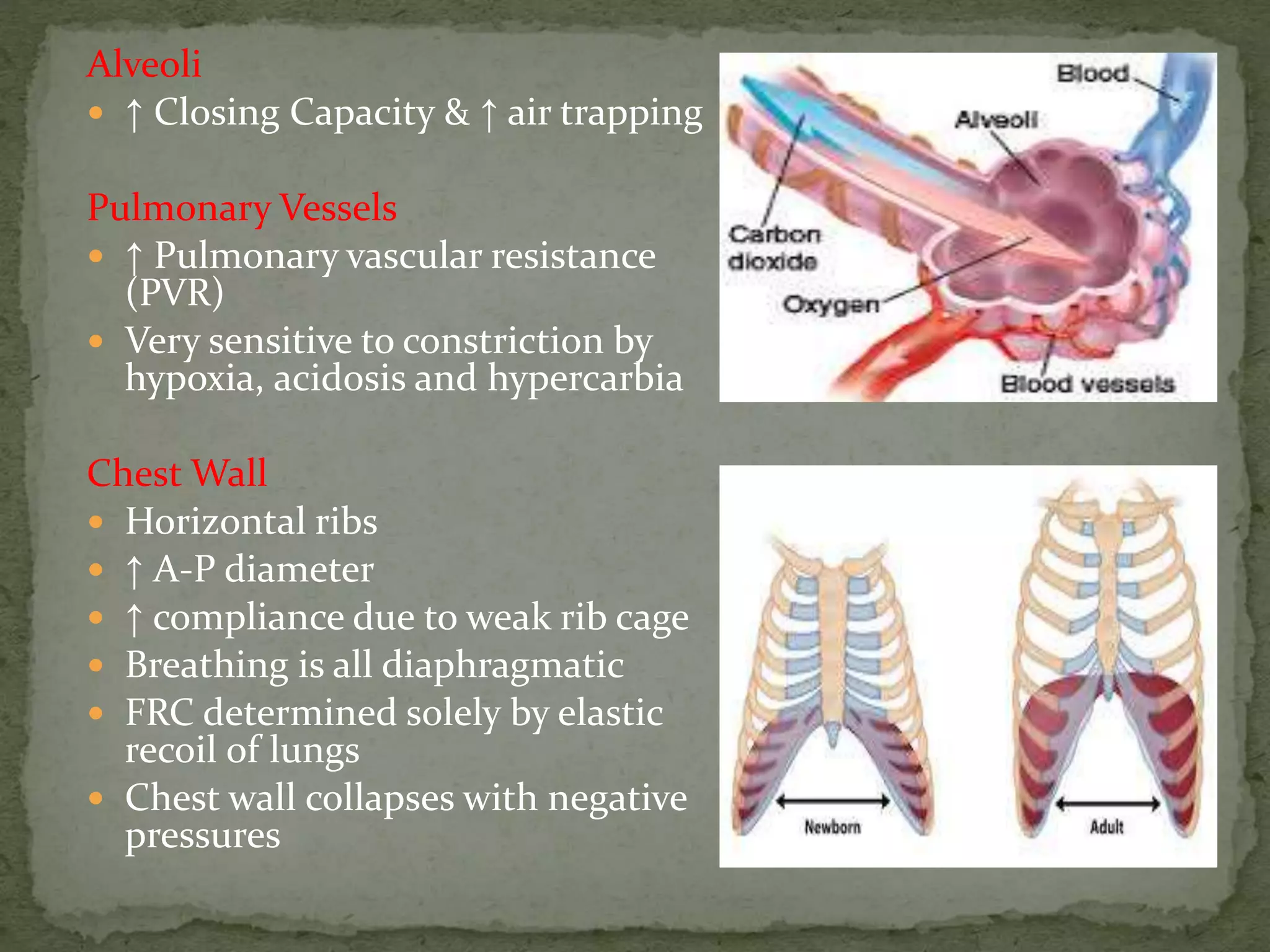
Lung compliance is less while chest wall compliance is
more than those in adults - Reduced FRC and Atelectasis.
Infant’s FRC is diminished and de-saturation occurs more
precipitously
Lack Type I muscle fibers, fatigue more easily
Prone to Bradycardia - Laryngeal stimulation and hypoxia](https://image.slidesharecdn.com/mypresentation-150223160008-conversion-gate01/75/PAEDIATRIC-AIRWAY-15-2048.jpg)