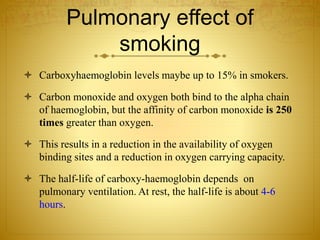
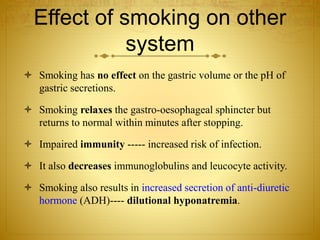
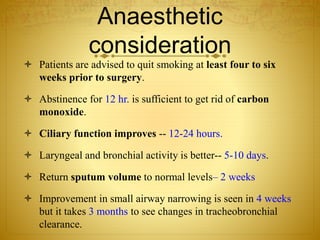
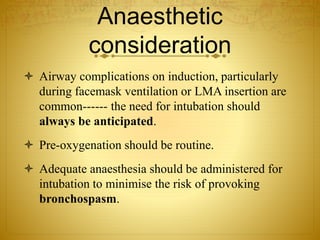
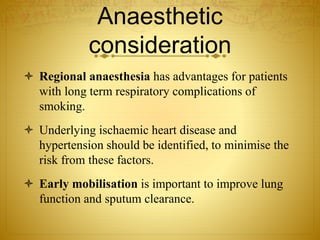
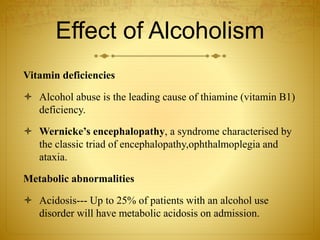
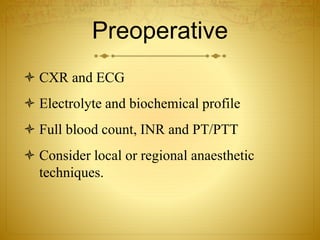
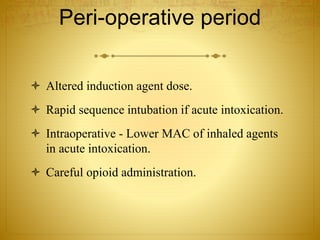
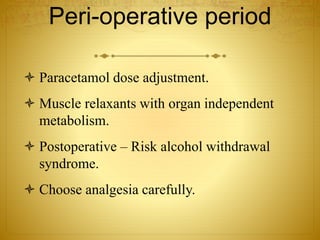
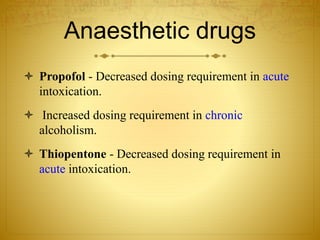
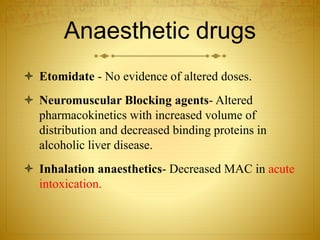
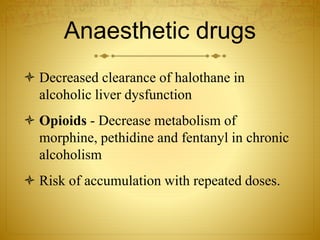
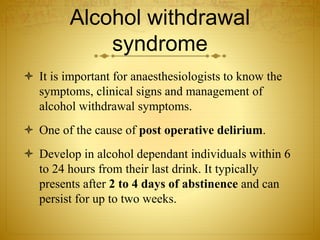
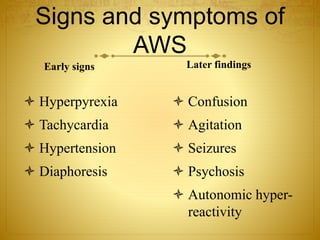
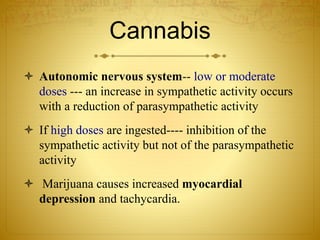
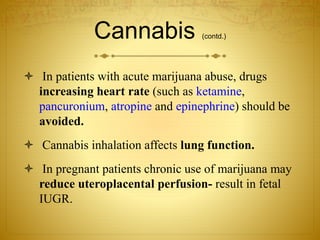
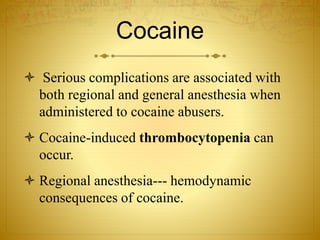
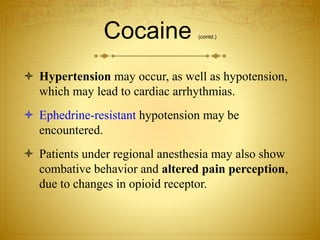
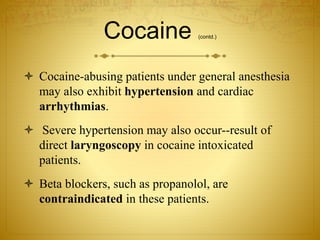
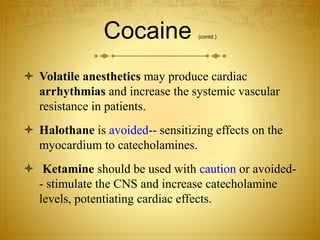
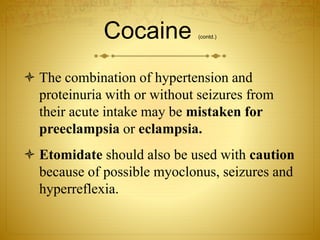
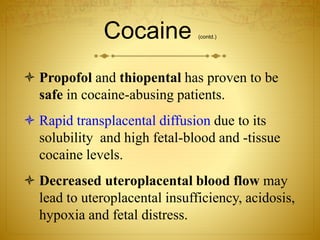
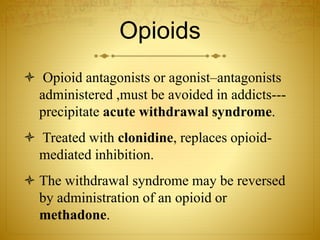
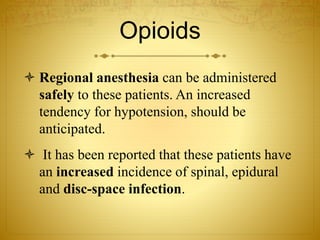
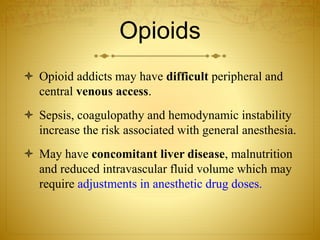
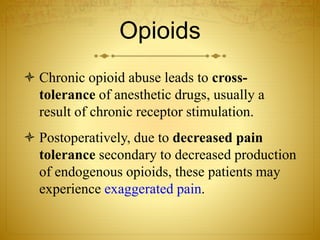
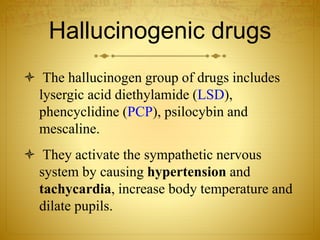
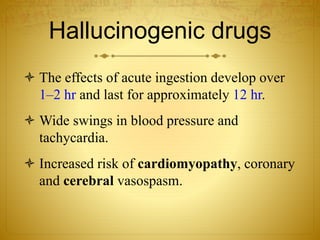
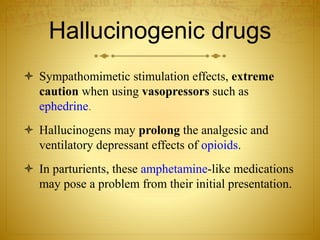
Smoking, alcoholism, and drug addiction can impact anesthesia care. Smoking increases risks of pulmonary and cardiovascular complications. Alcoholism can cause vitamin deficiencies, metabolic abnormalities, and liver or pancreatic damage. Drug abuse may cause pulmonary, cardiac, or CNS issues that worsen under anesthesia. When providing anesthesia for smokers, alcoholics, or drug abusers, their medical history must be thoroughly reviewed and precautions taken regarding airway management, hemodynamic stability, and potential withdrawal syndromes.