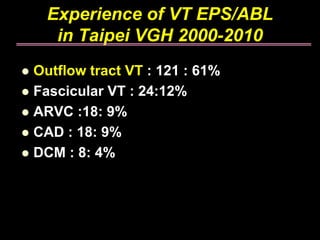
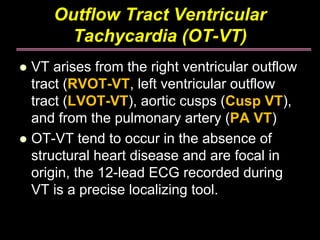
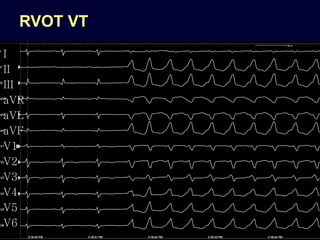
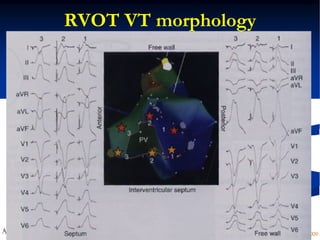
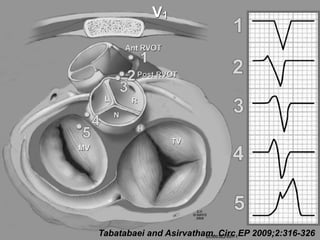
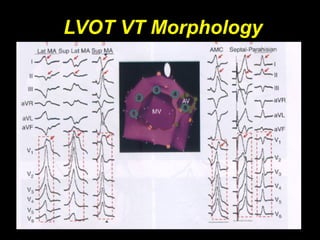
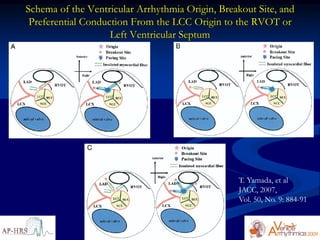
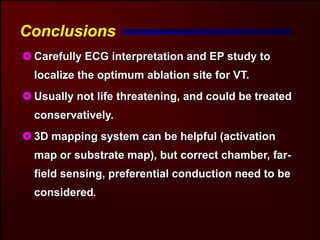
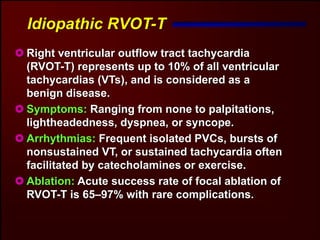
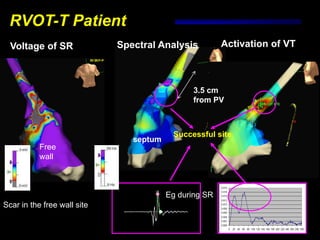
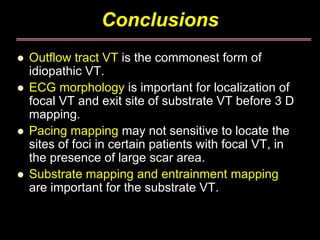
1. Outflow tract VT is the most common type of idiopathic VT, accounting for over 60% of cases in the study.
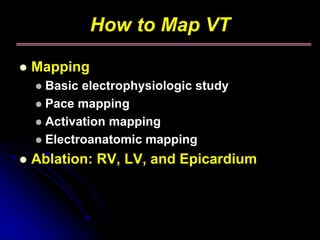
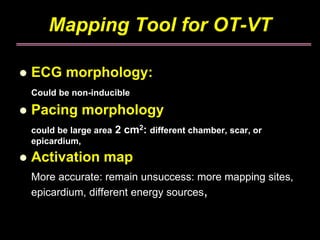
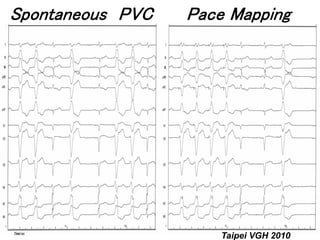
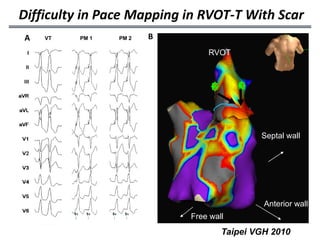
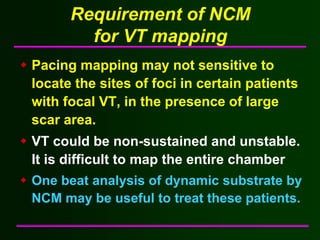
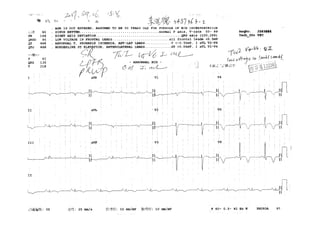
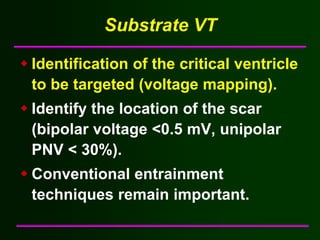
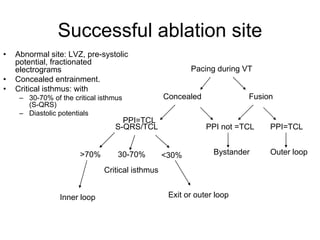
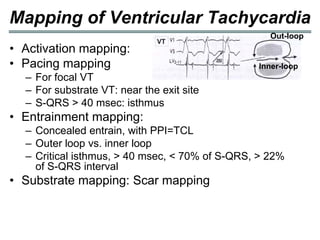
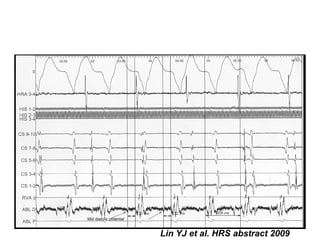
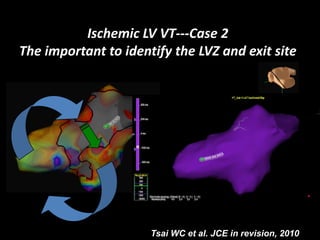
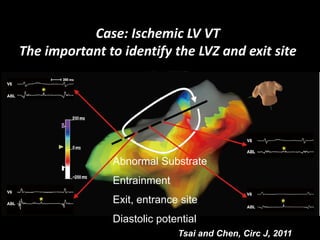
2. Pace mapping alone may not accurately locate ablation sites, especially for VT associated with scar tissue. Activation mapping and substrate identification are important complementary mapping techniques.
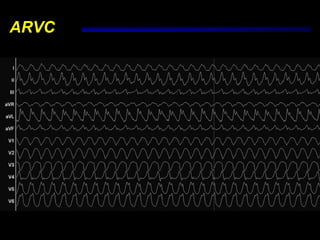
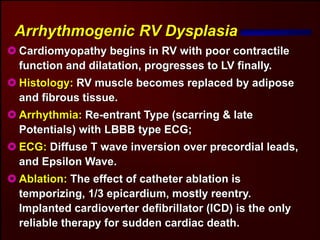
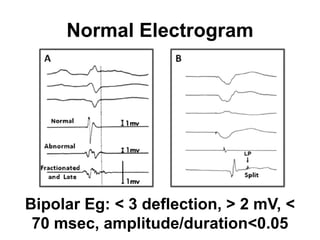
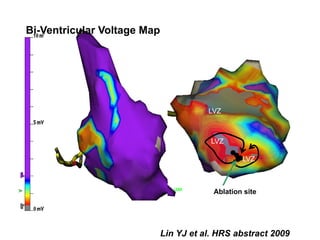
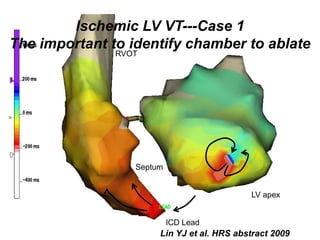
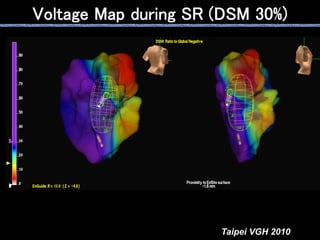
3. Successful ablation of substrate-based VT requires targeting abnormal electrograms within scar regions like late potentials or fractionated signals at the critical isthmus.