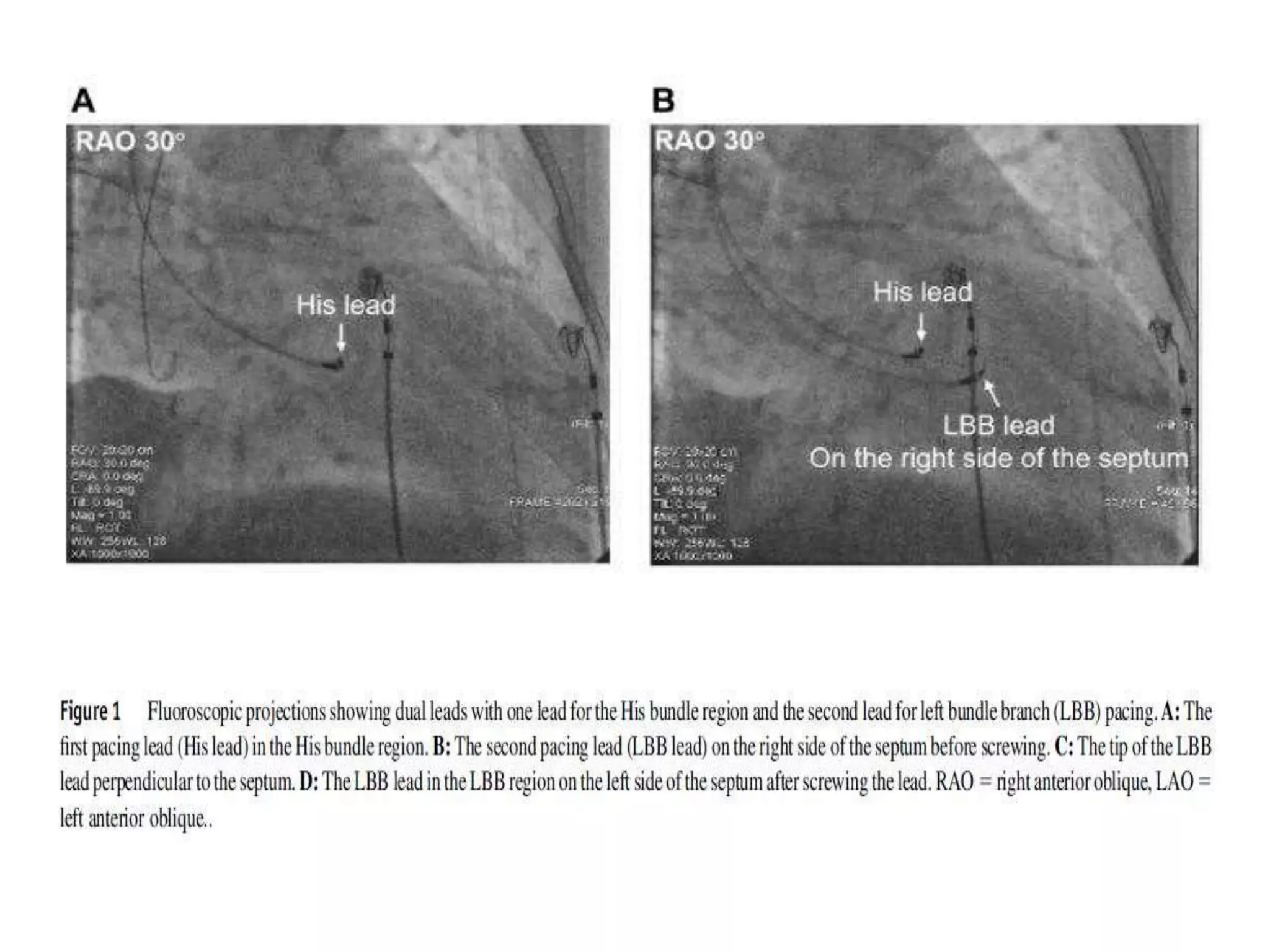
- Left bundle branch pacing (LBBP) was attempted in 87 patients needing a pacemaker, successfully implanting the lead in the left bundle branch in 80.5% of patients.
- LBBP resulted in a shorter paced QRS duration and left ventricular activation time compared to right ventricular septal pacing. It also had a lower pacing threshold and higher R-wave amplitude.
- The study demonstrated the feasibility of LBBP with potential advantages over traditional right ventricular and His bundle pacing, including more physiological ventricular activation. However, larger long-term studies are still needed to understand the full benefits of LBBP.