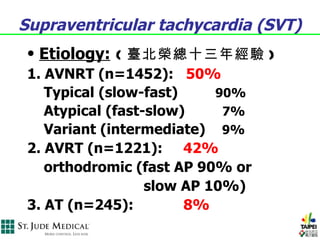
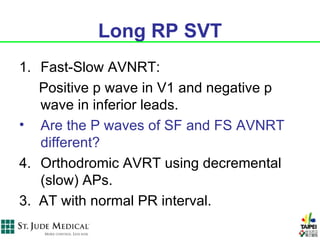
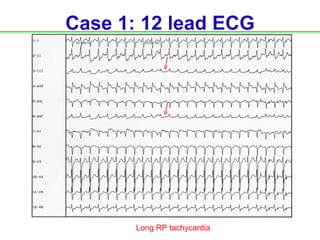
1. This document provides an overview of a training course on complex supraventricular tachycardia (SVT) differentiation. It discusses various SVT etiologies and electrocardiogram patterns.
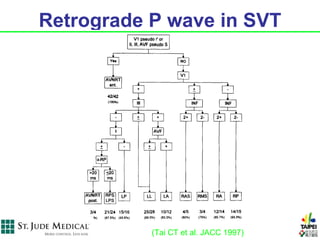
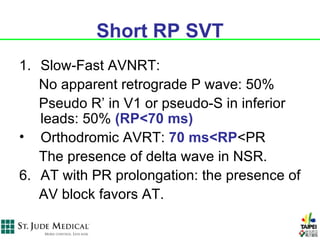
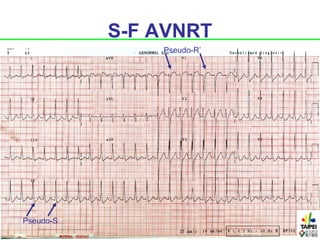
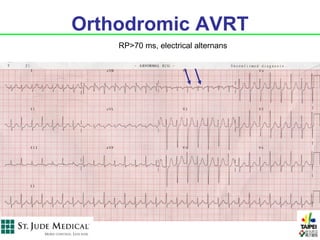
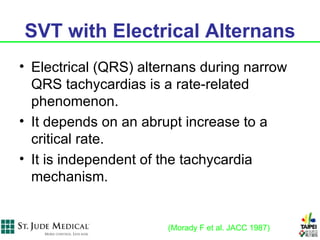
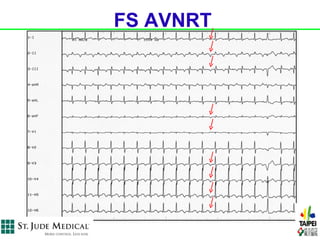
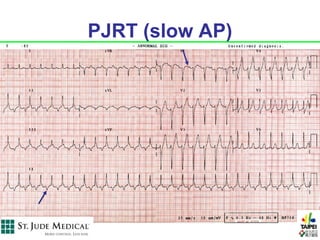
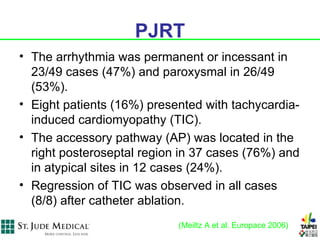
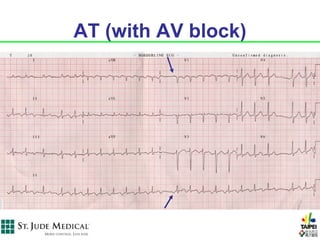
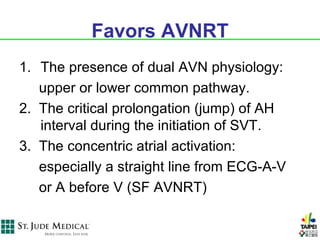
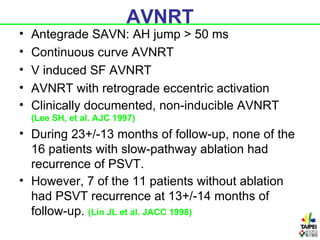
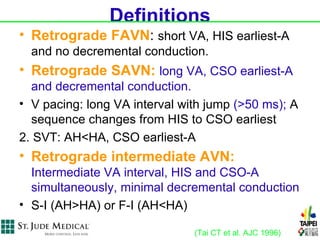
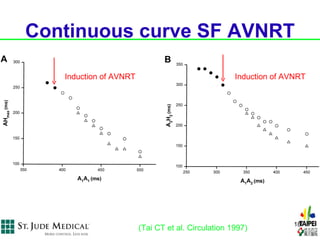
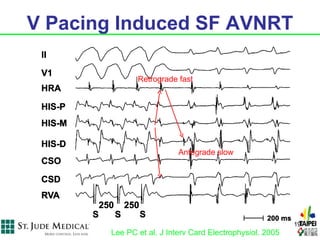
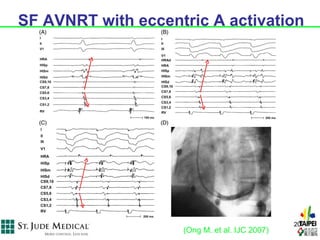
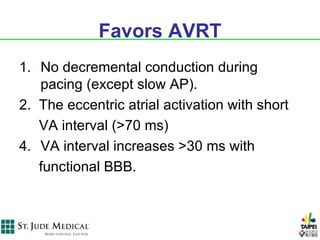
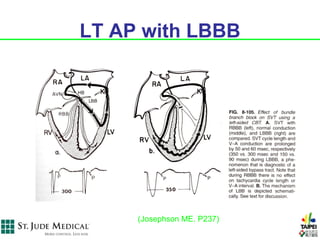
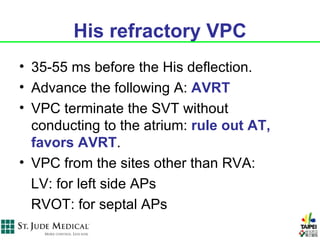
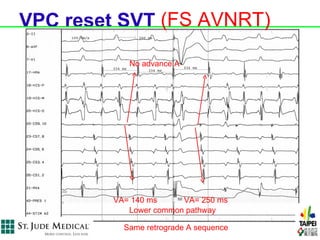
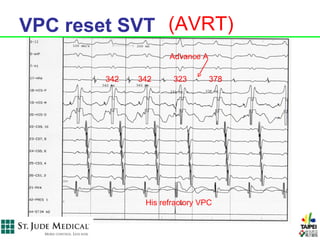
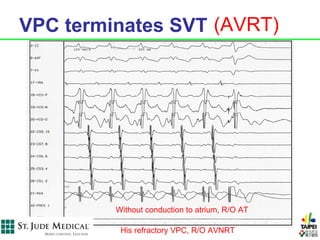
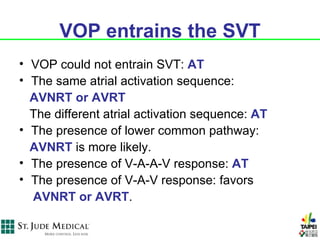
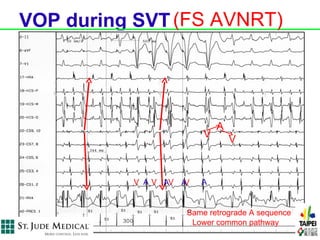
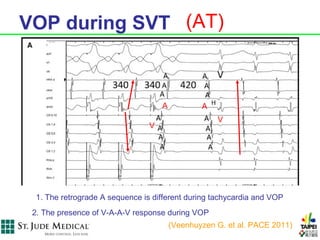
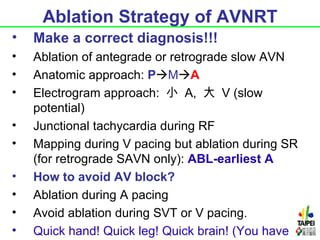
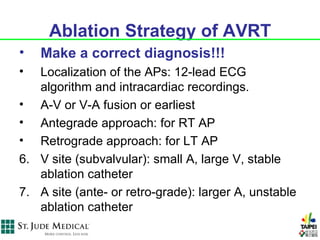
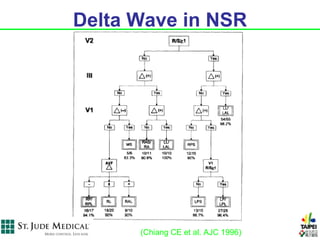
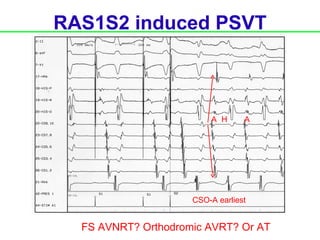
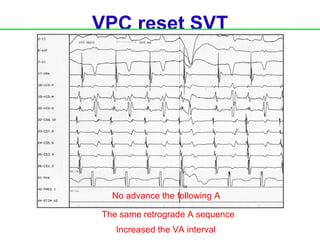
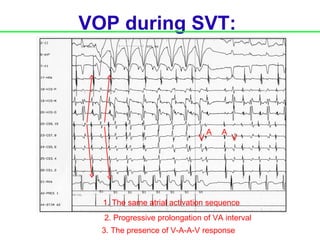
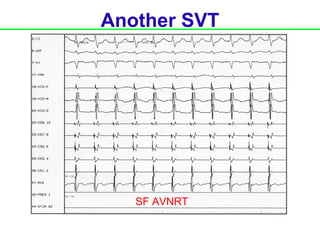
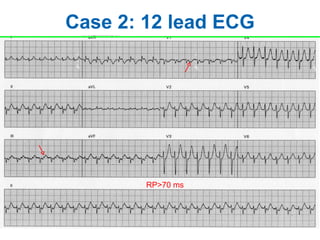
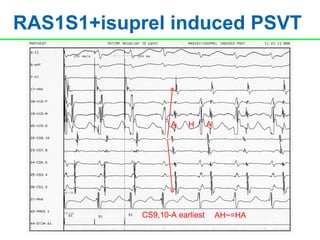
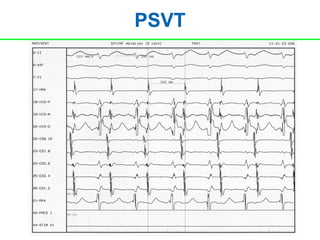
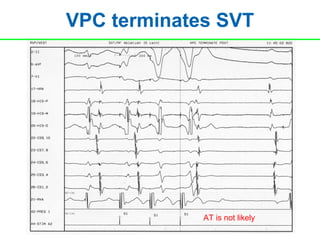
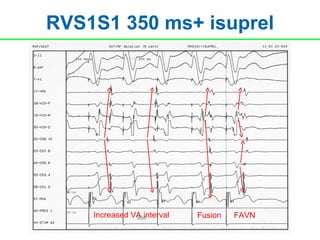
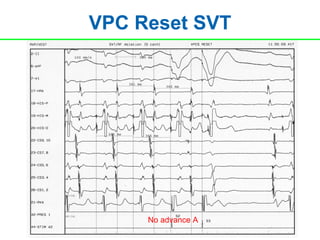
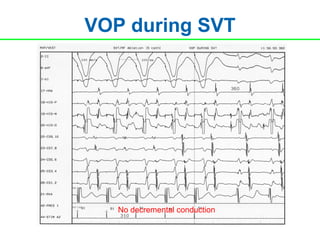
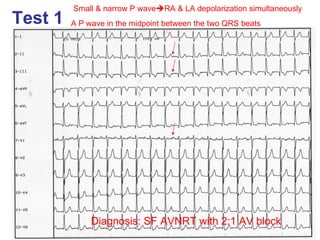
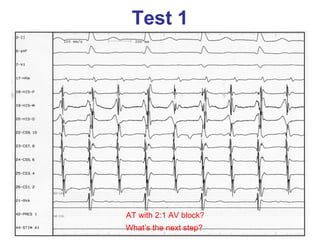
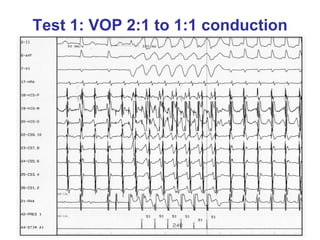
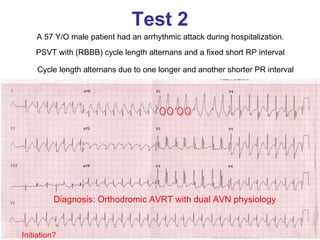
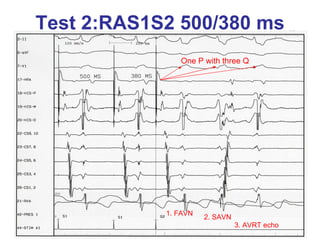
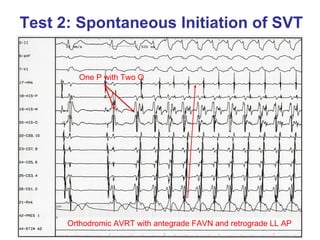
2. Mechanisms of SVT discussed include atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT), and atrial tachycardia (AT). The document also reviews electrophysiology study findings that help differentiate the mechanisms.
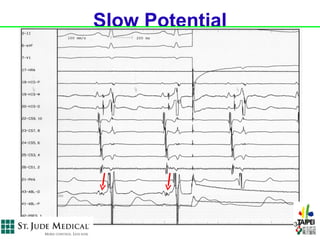
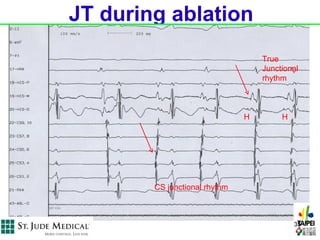
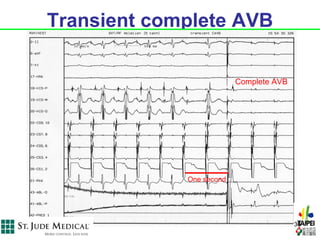
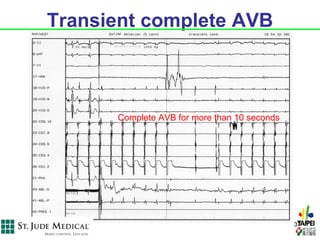
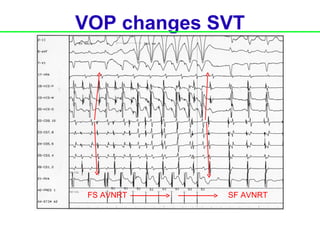
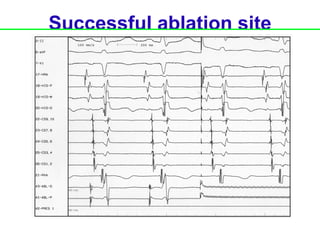
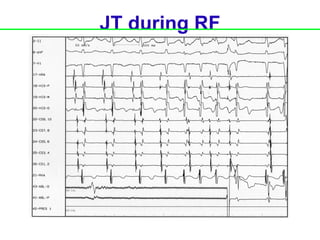
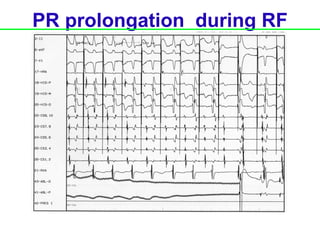
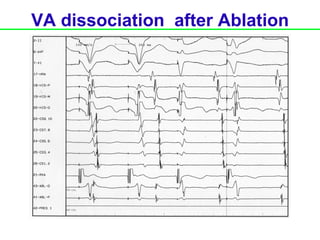
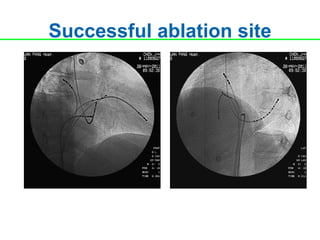
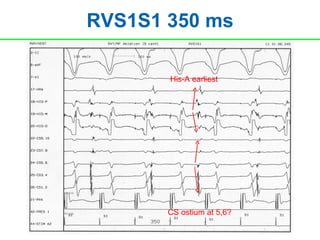
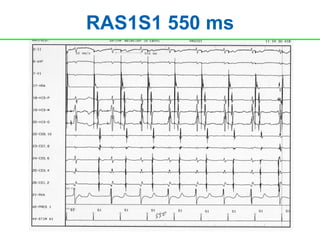
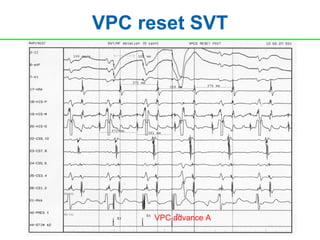
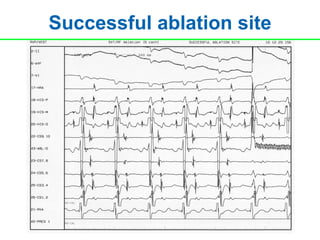
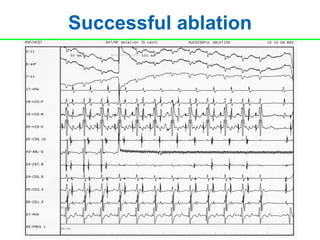
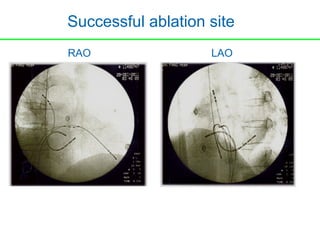
3. Case examples are presented to demonstrate electrophysiology study techniques for SVT diagnosis and ablation, including ventricular overdrive pacing, ventricular extrastimuli, and induction protocols.