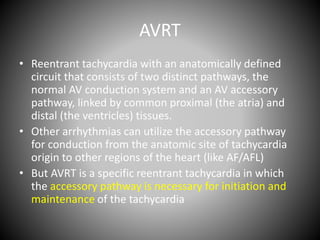
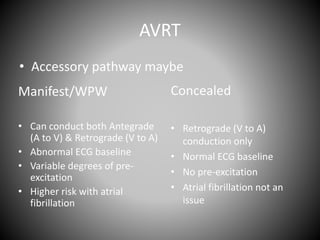
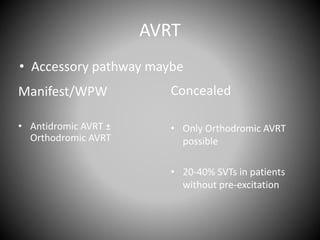
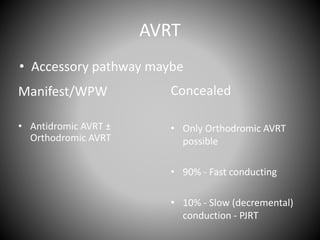
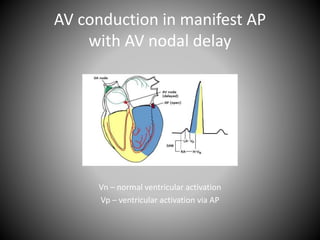
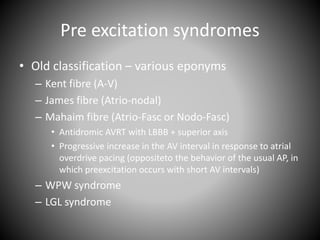
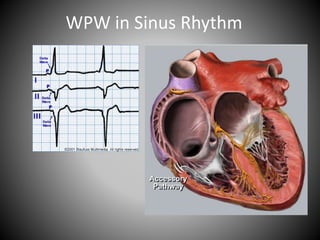
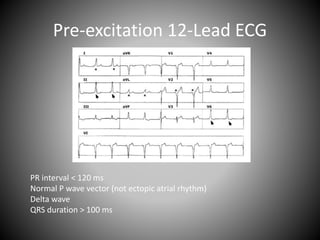
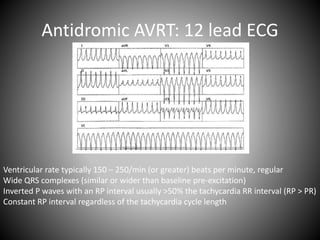
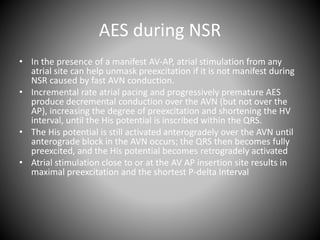
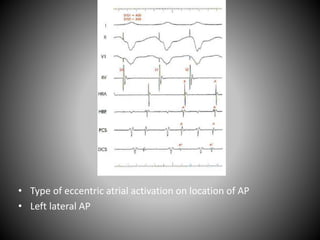
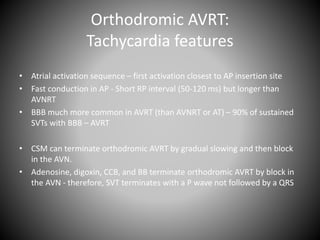
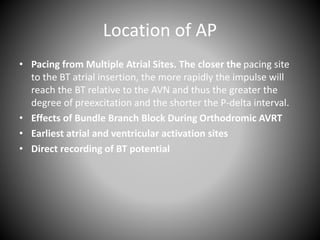
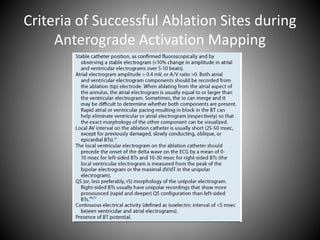
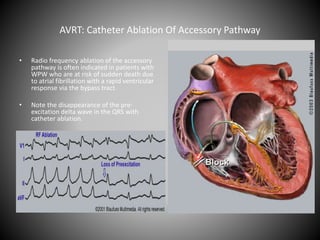
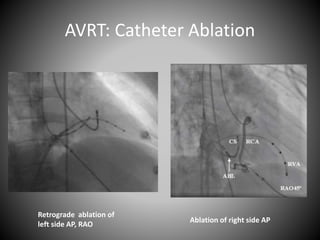
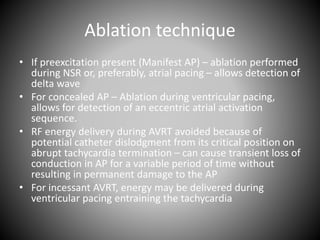
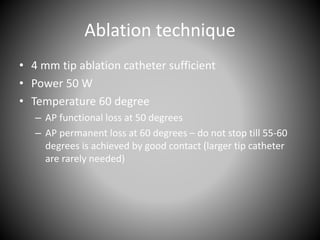
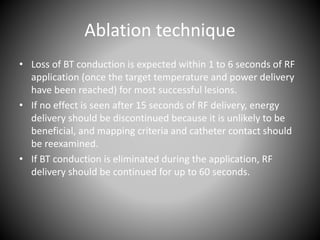
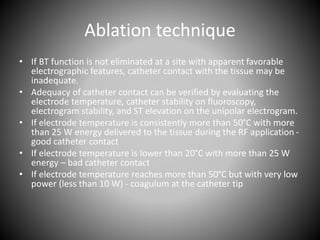
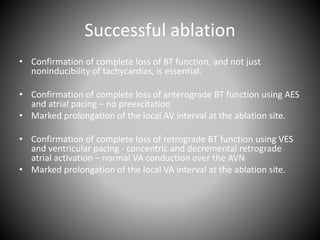
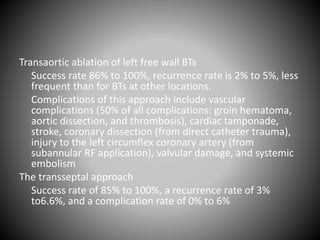
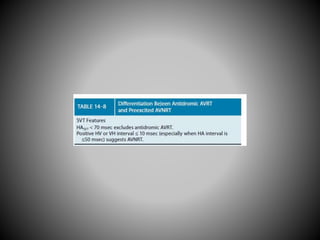
This document discusses electrophysiological diagnosis and management of atrioventricular reentrant tachycardia (AVRT). It describes the historical discovery of Wolff-Parkinson-White syndrome and mechanisms of tachyarrhythmias including reentry. Characteristics of orthodromic and antidromic AVRT are provided along with techniques for evaluating accessory pathways including baseline observations, programmed stimulation, and catheter ablation. Precise localization of accessory pathways is important for successful ablation.