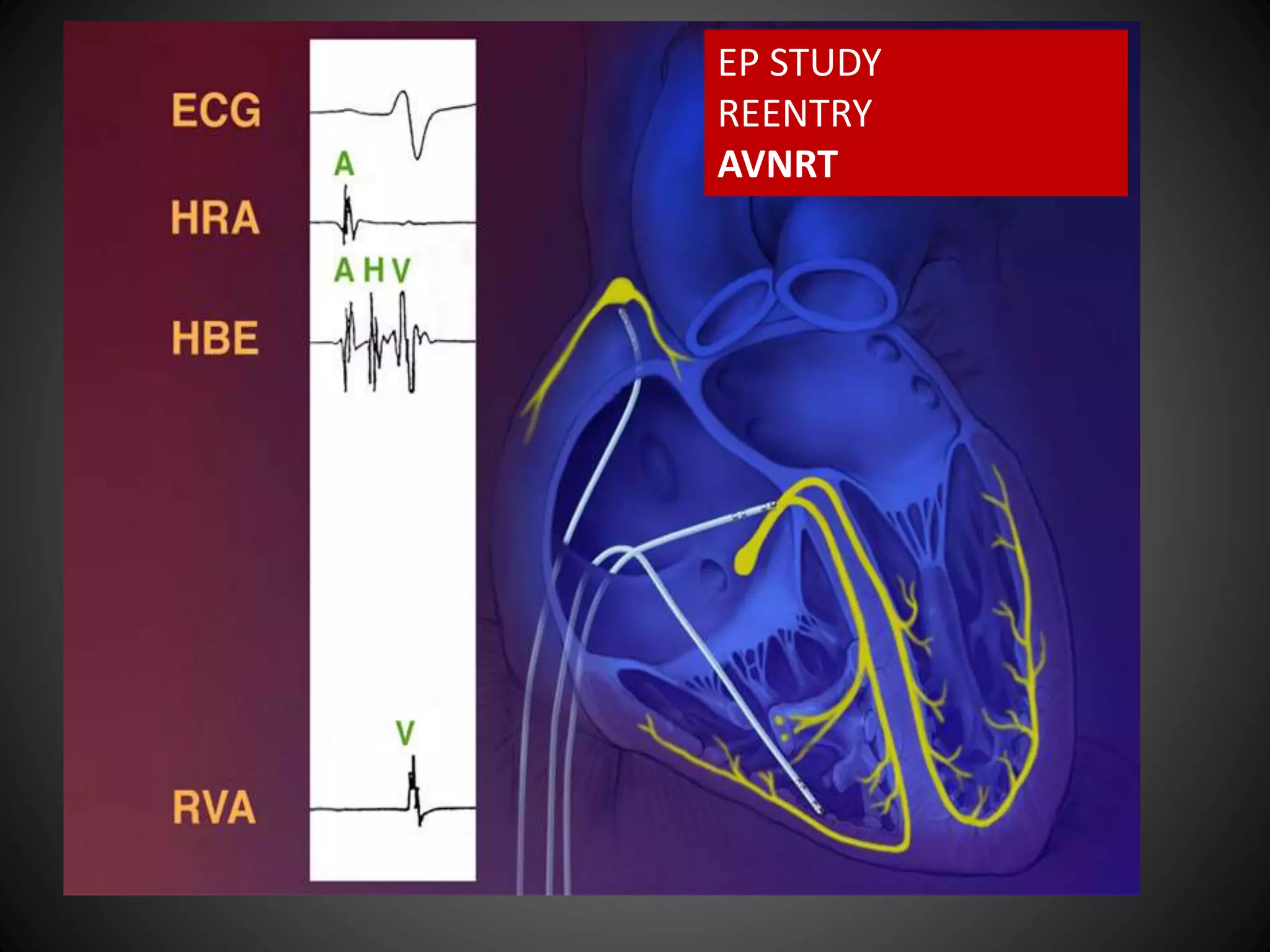
This document provides an overview of AV nodal reentrant tachycardia (AVNRT) including its mechanisms, diagnosis using electrophysiology study techniques, and treatment with catheter ablation. It discusses the criteria for diagnosing dual AV nodal physiology, how AVNRT is initiated via programmed stimulation, its characteristic surface ECG patterns, and how the arrhythmia responds to different tests such as atrial and ventricular stimulation. The document emphasizes that AVNRT is the most common type of supraventricular tachycardia and is due to reentry involving slow and fast pathways in the AV node.