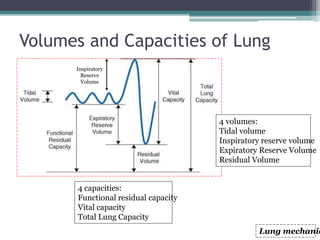
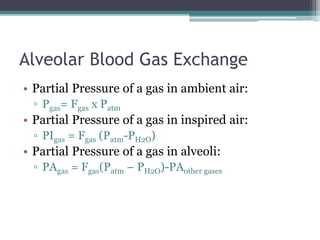
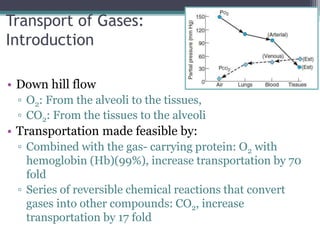
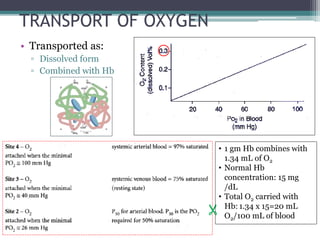
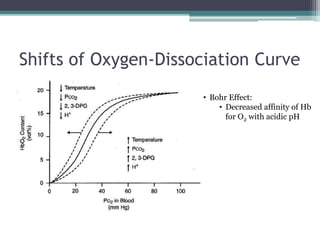
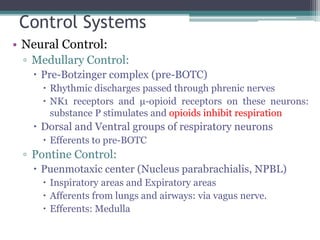
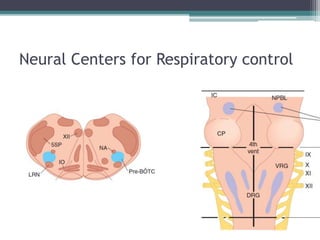
The document is a comprehensive presentation on respiratory physiology delivered by Dr. Pravin Prasad, covering key topics such as lung mechanics, gas exchange, and regulation of respiration. It details the various volumes and capacities of the lungs, mechanisms of gas transport, and factors affecting oxygen and carbon dioxide concentrations in the blood. Additionally, it addresses conditions like hypoxemia and includes discussions on respiratory acidosis and alkalosis, as well as control systems for respiration.



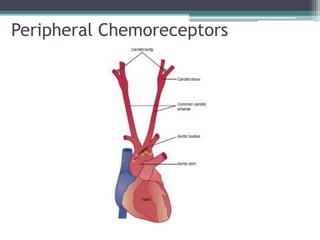
![Receptors
• Central Chemo-receptors
▫ Stimulated by CSF [H+] and CO2
▫ Adaptation occurs
▫ Insensitive to PO2 and arterial H+
• Peripheral Chemo-receptors
▫ Carotid bodies:
near carotid sinus, afferents to CN IX
▫ Aortic bodies:
Aortic arch, afferents to CN X
▫ Contains:
H+/CO2 receptors: less sensitive, but maintains the normal
drive.
Po2 receptors: responds to PO2 (dissolved O2) and not to total
oxygen content(bound to Hb).
Do not contribute to normal drive.
Activated if PaO2 <50-60 mmHg
▫ Do not adapt.](https://image.slidesharecdn.com/respiratoryphysiology-151225163624/85/Respiratory-physiology-33-320.jpg)