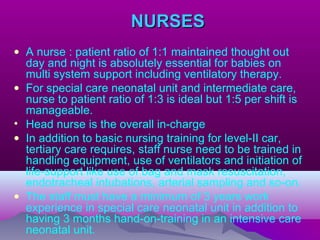
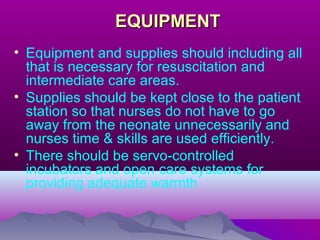
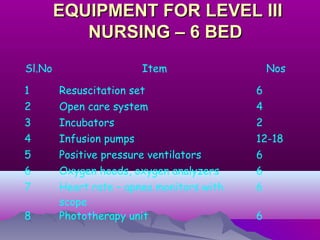
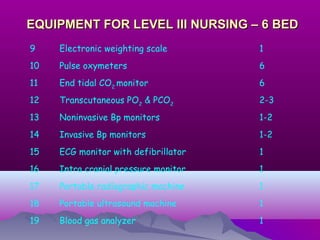
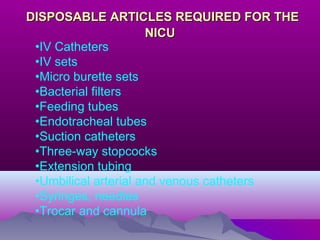
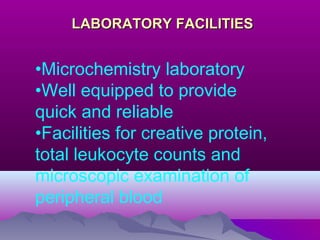
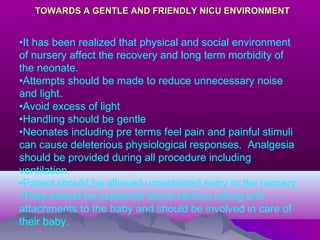
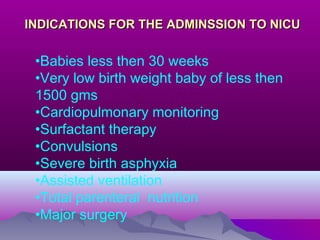
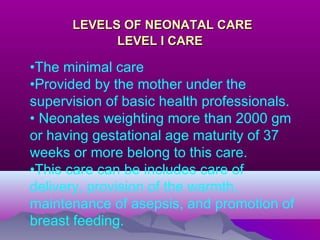
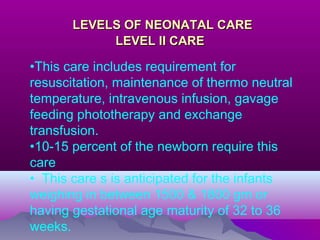
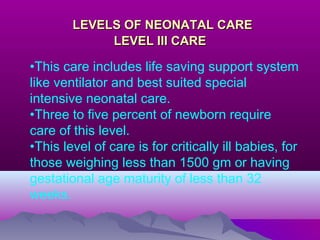
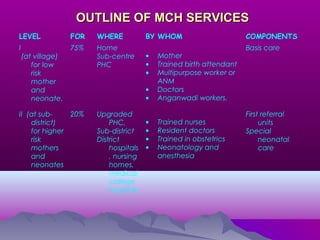
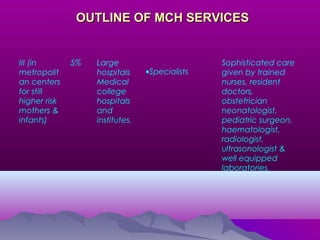
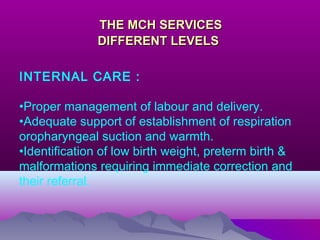
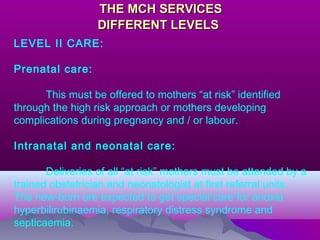
The document discusses the organization and setup of a Neonatal Intensive Care Unit (NICU). It describes the necessary physical space, facilities, equipment, staffing, and organization of care into three levels - basic, high-level, and intensive care. Key requirements for the NICU include appropriate space per bed, ventilation, lighting, environmental controls, and isolation rooms. Staffing must include neonatologists, nurses, and other medical experts. A full range of life-saving equipment is also needed to provide different levels of neonatal care for critically ill newborns.