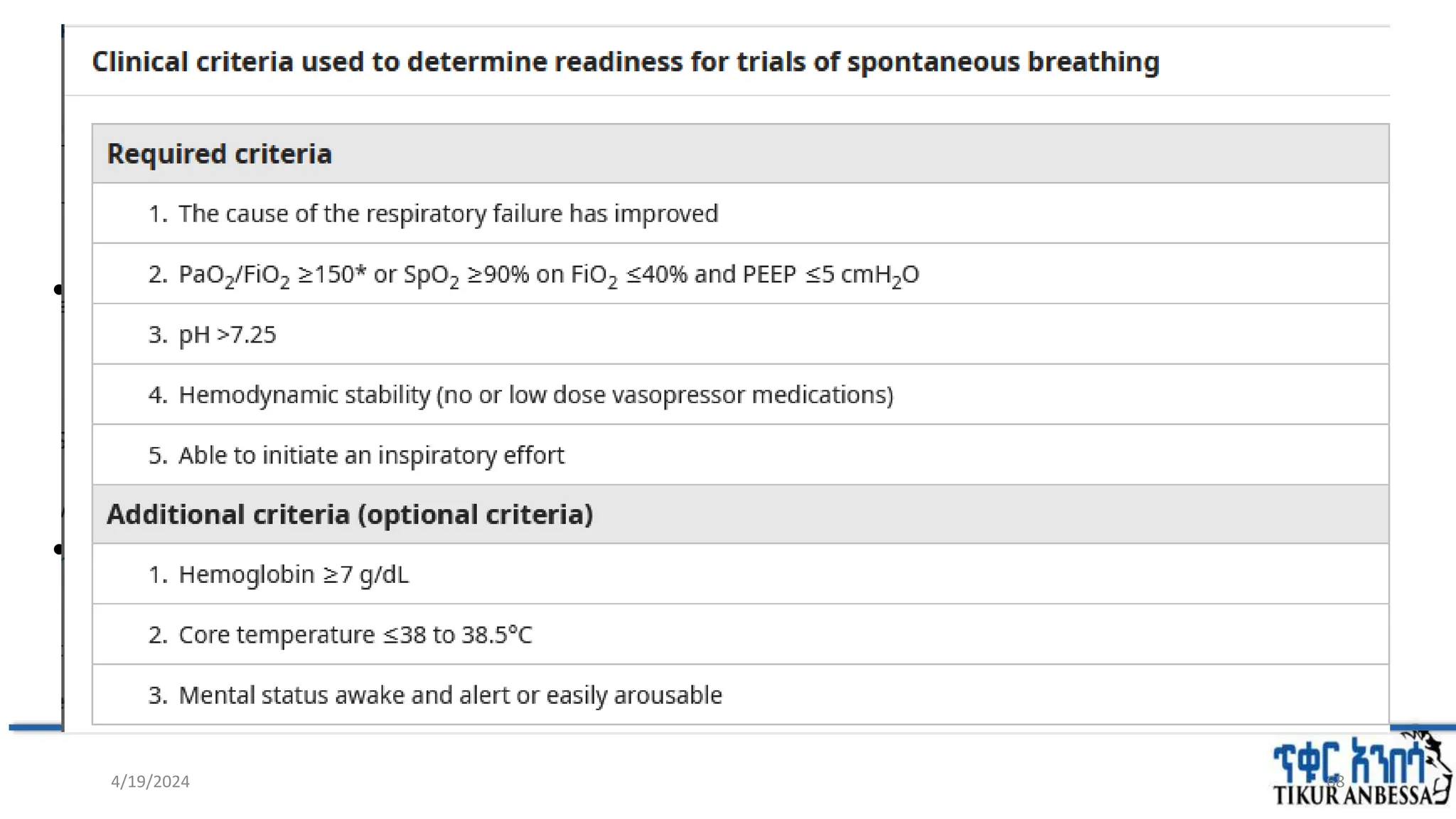
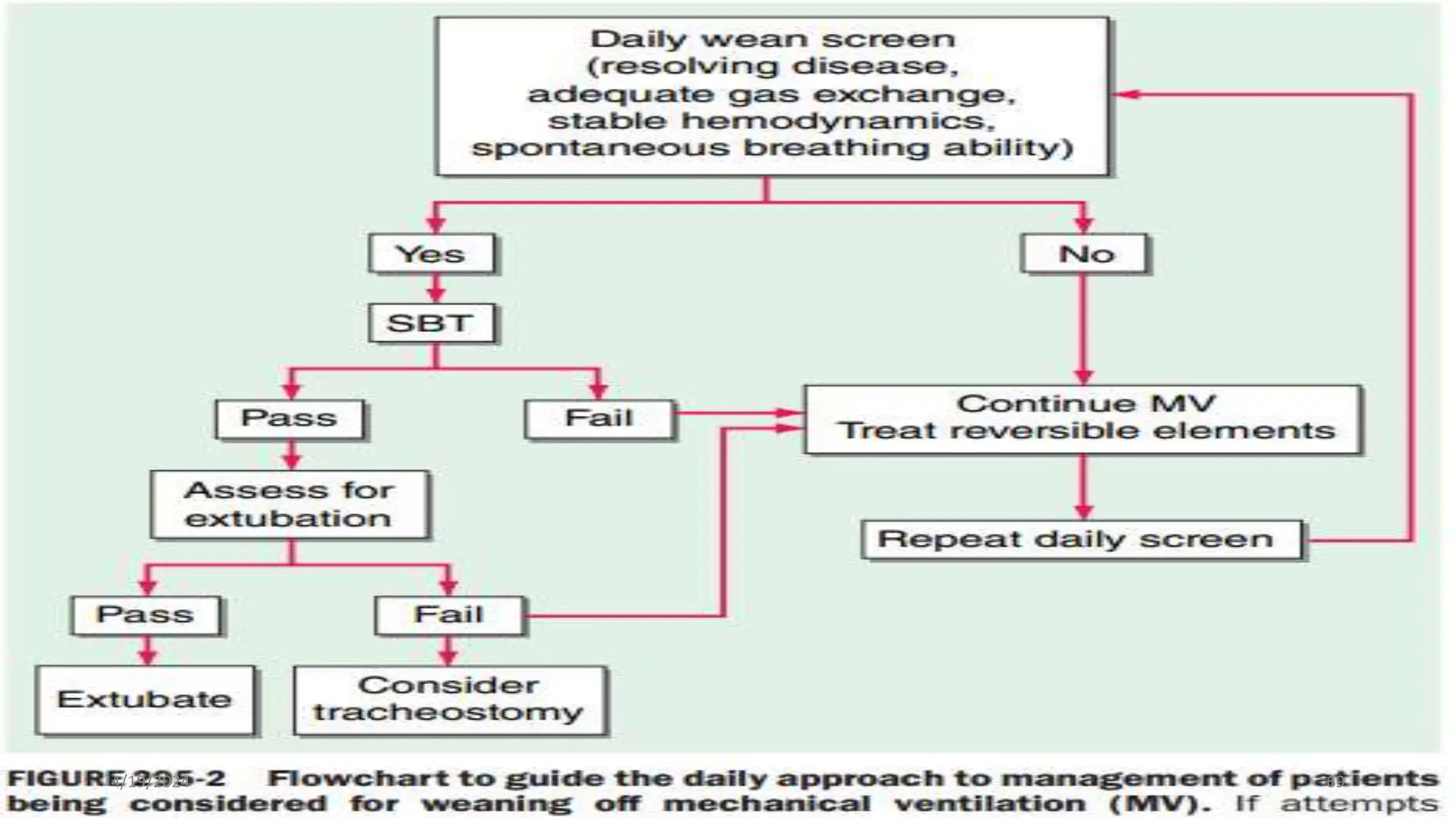
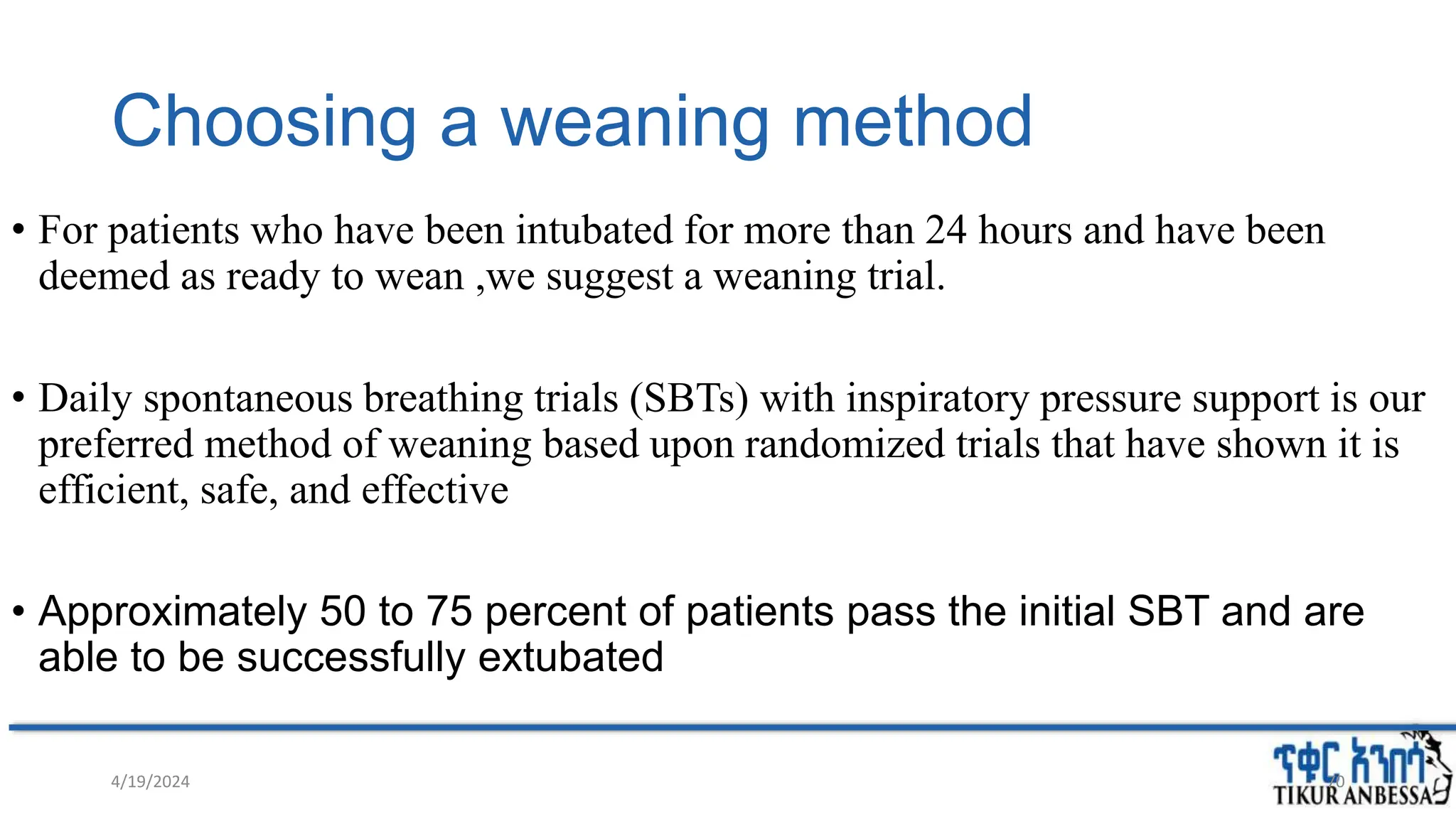
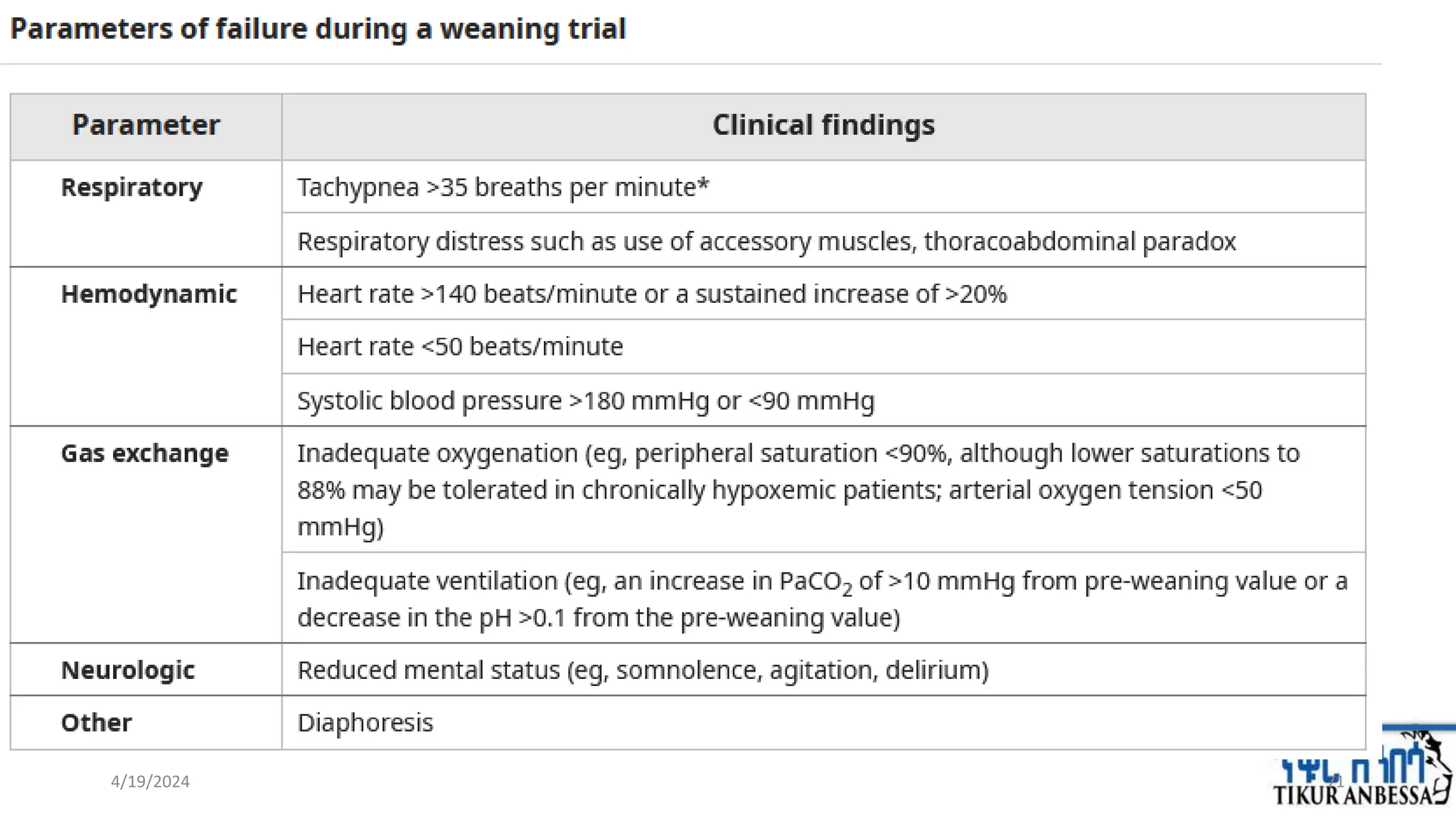
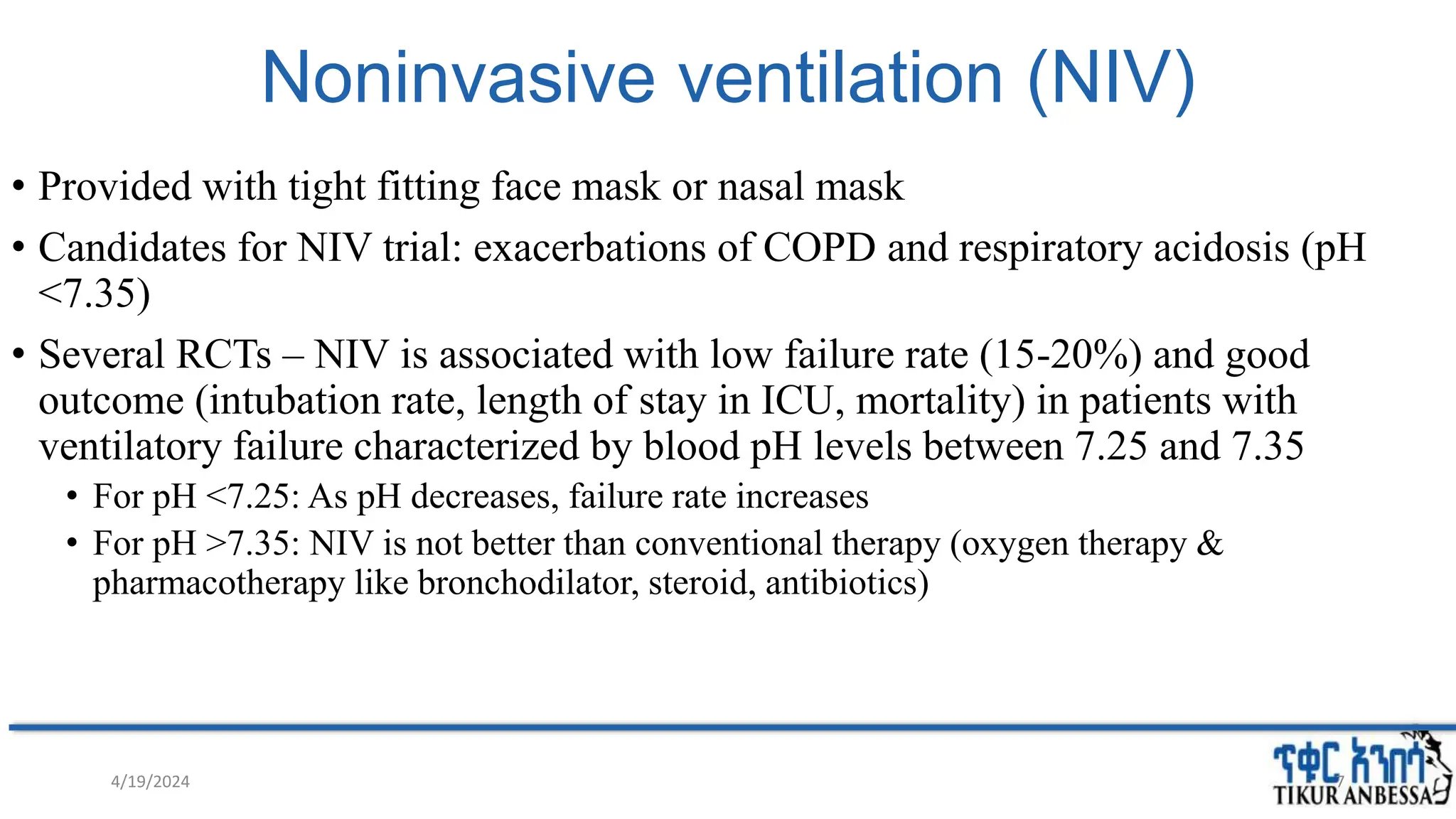
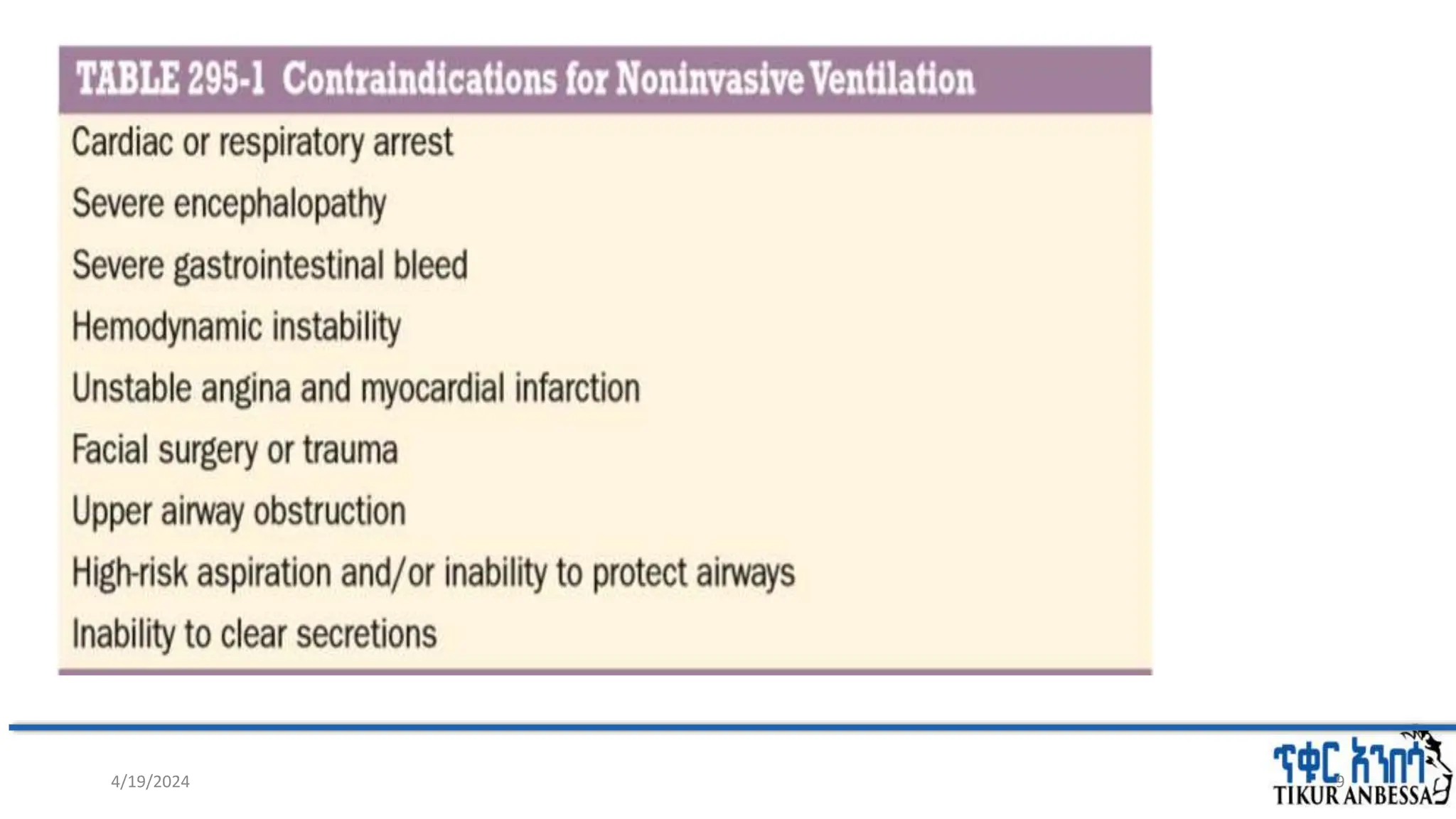
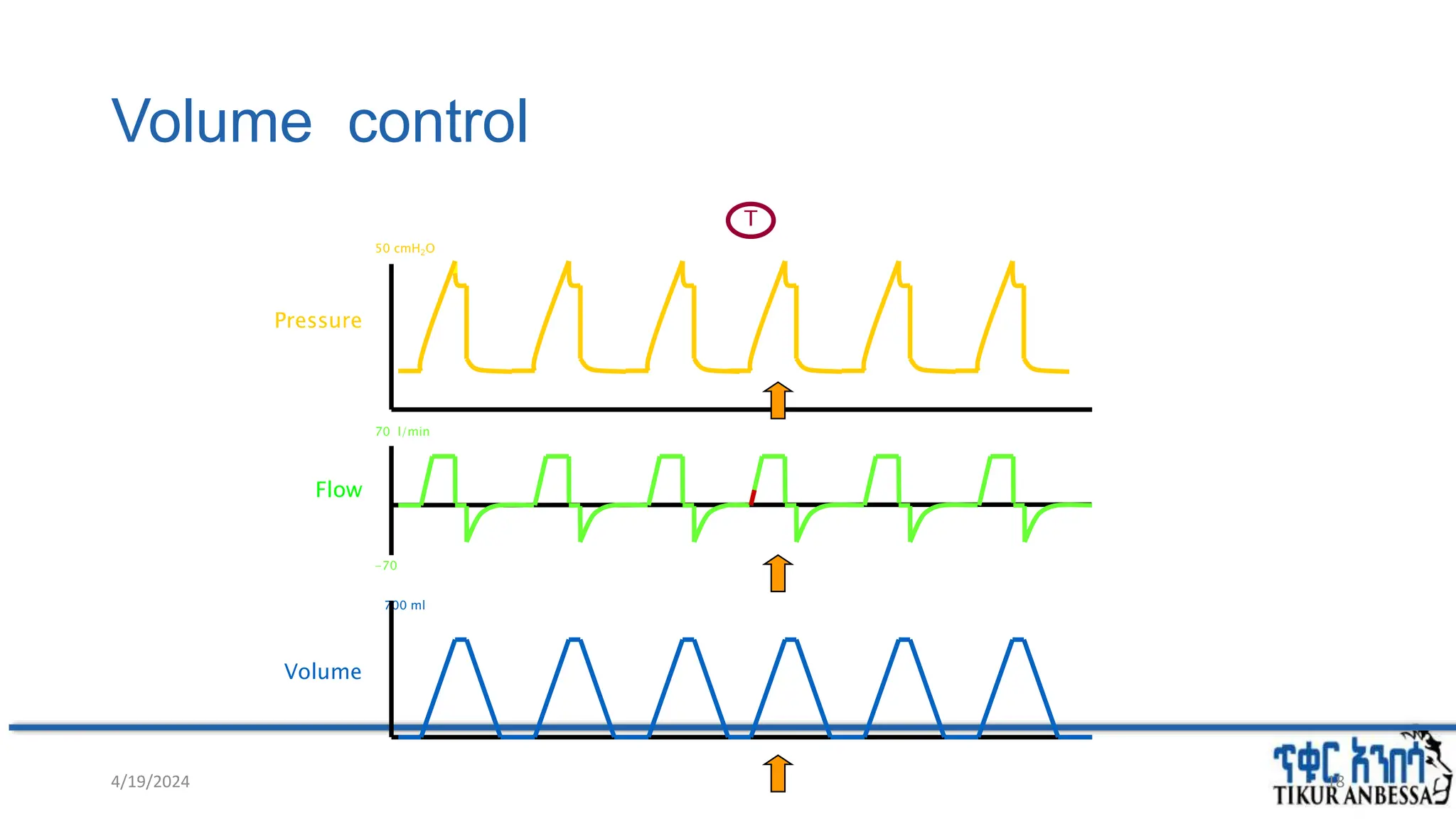
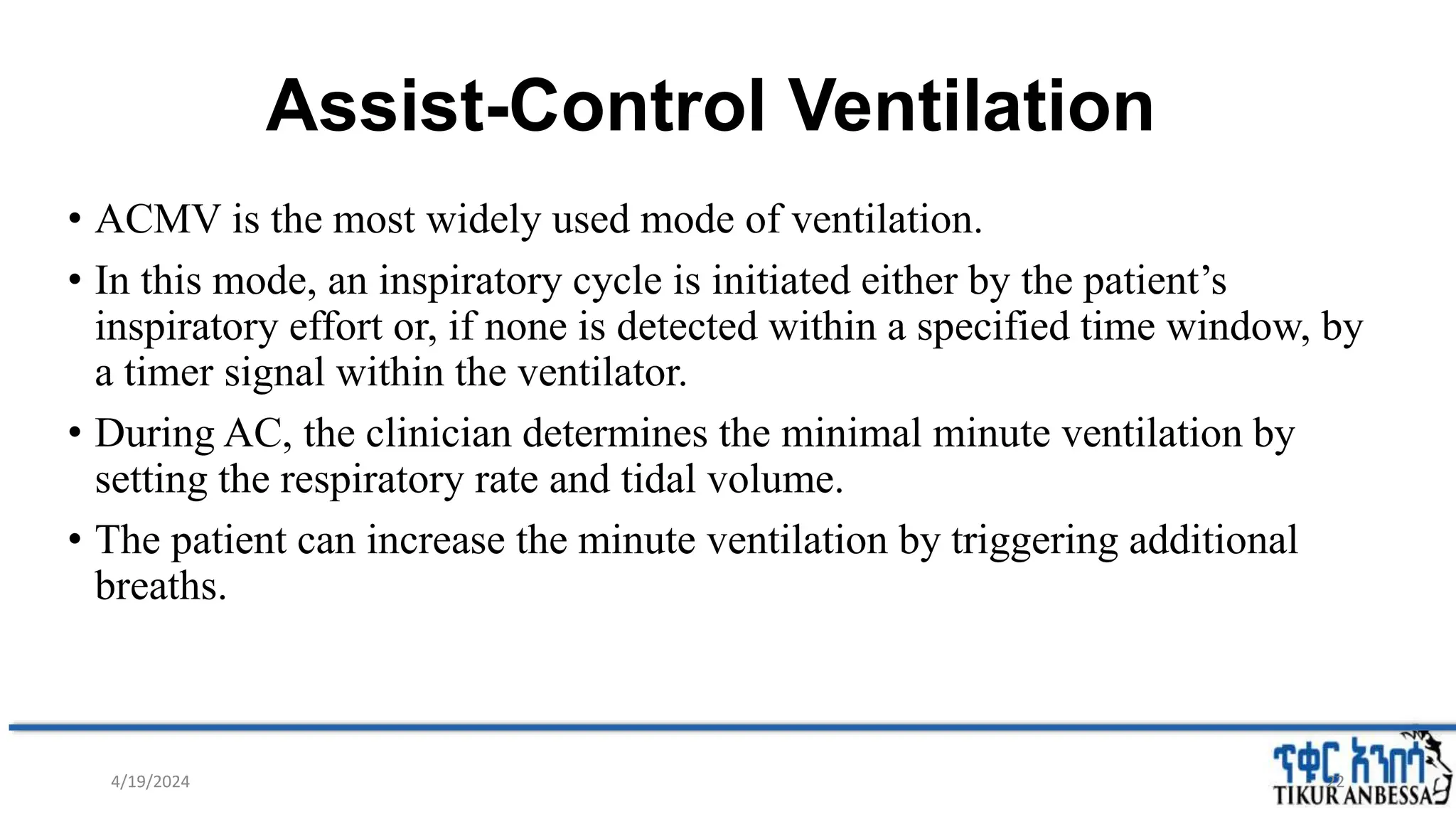
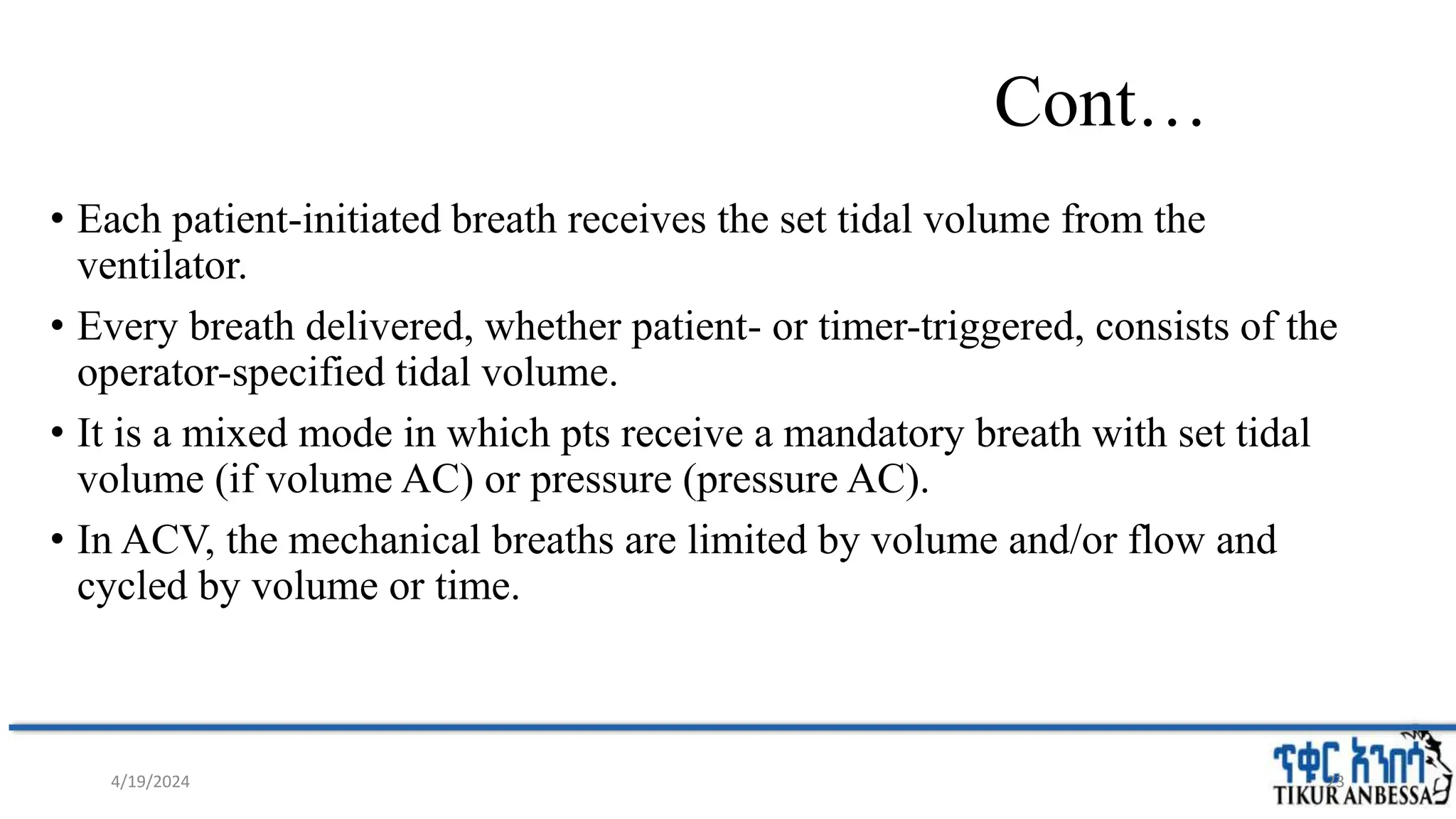
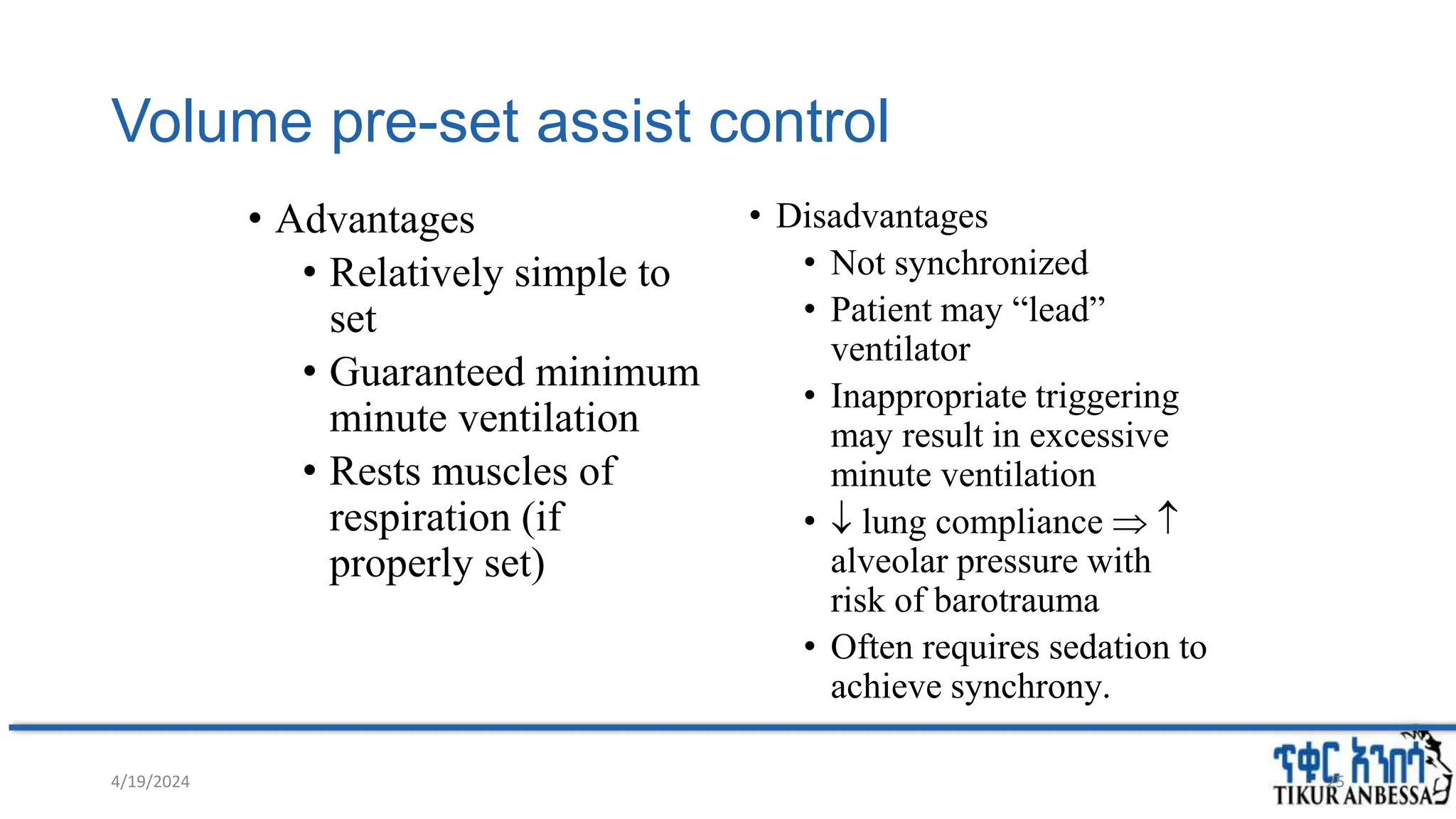
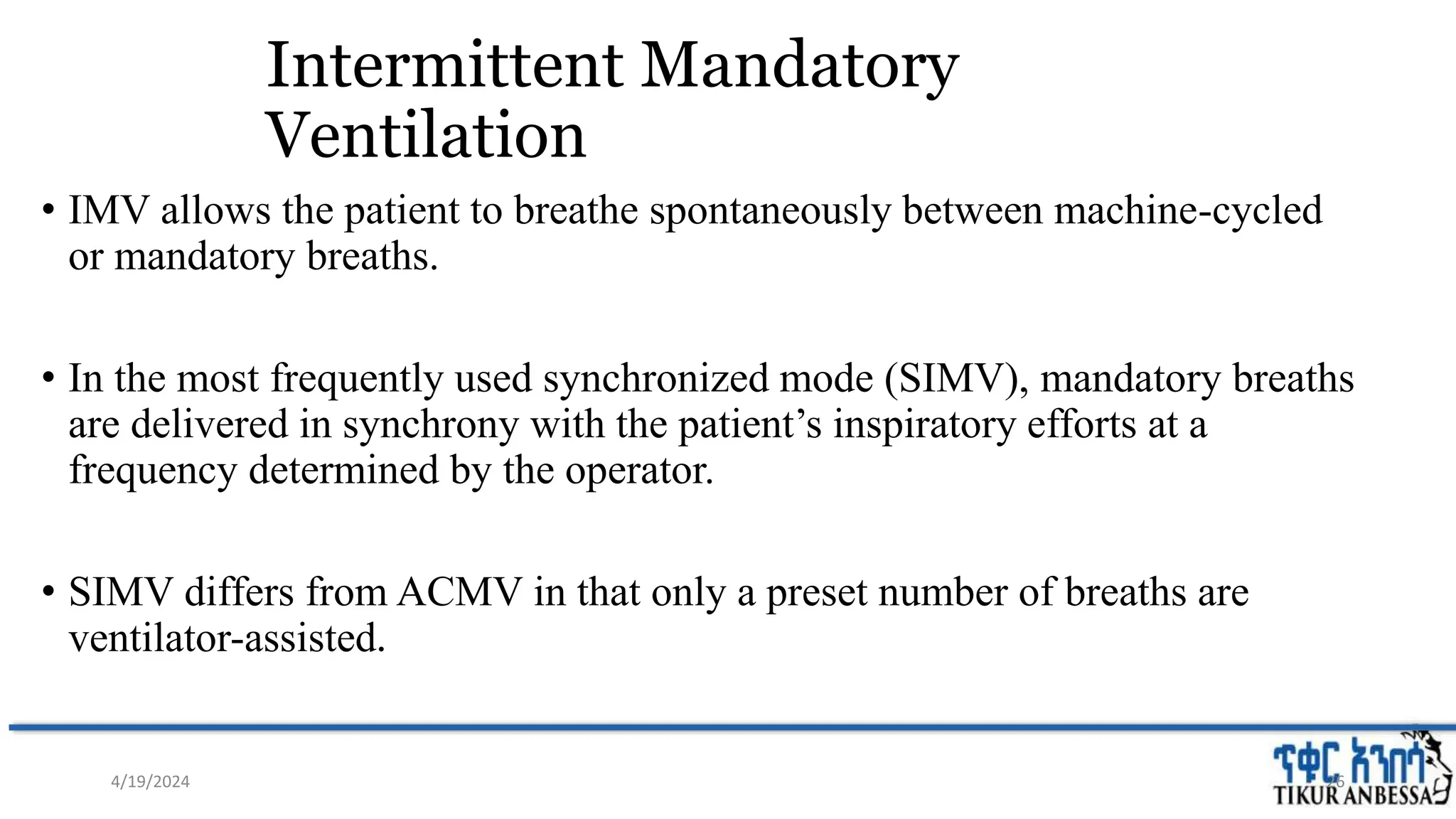
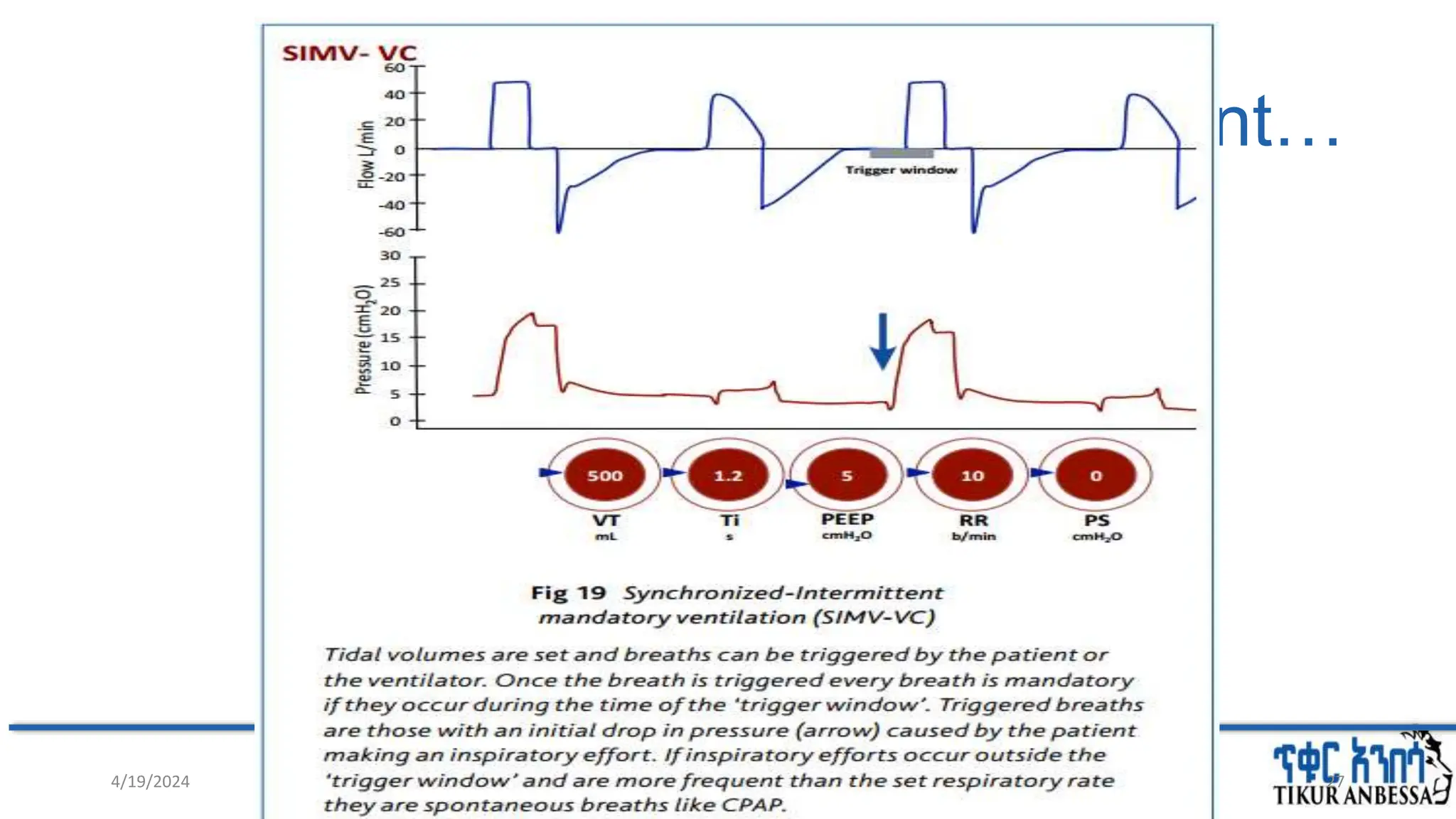
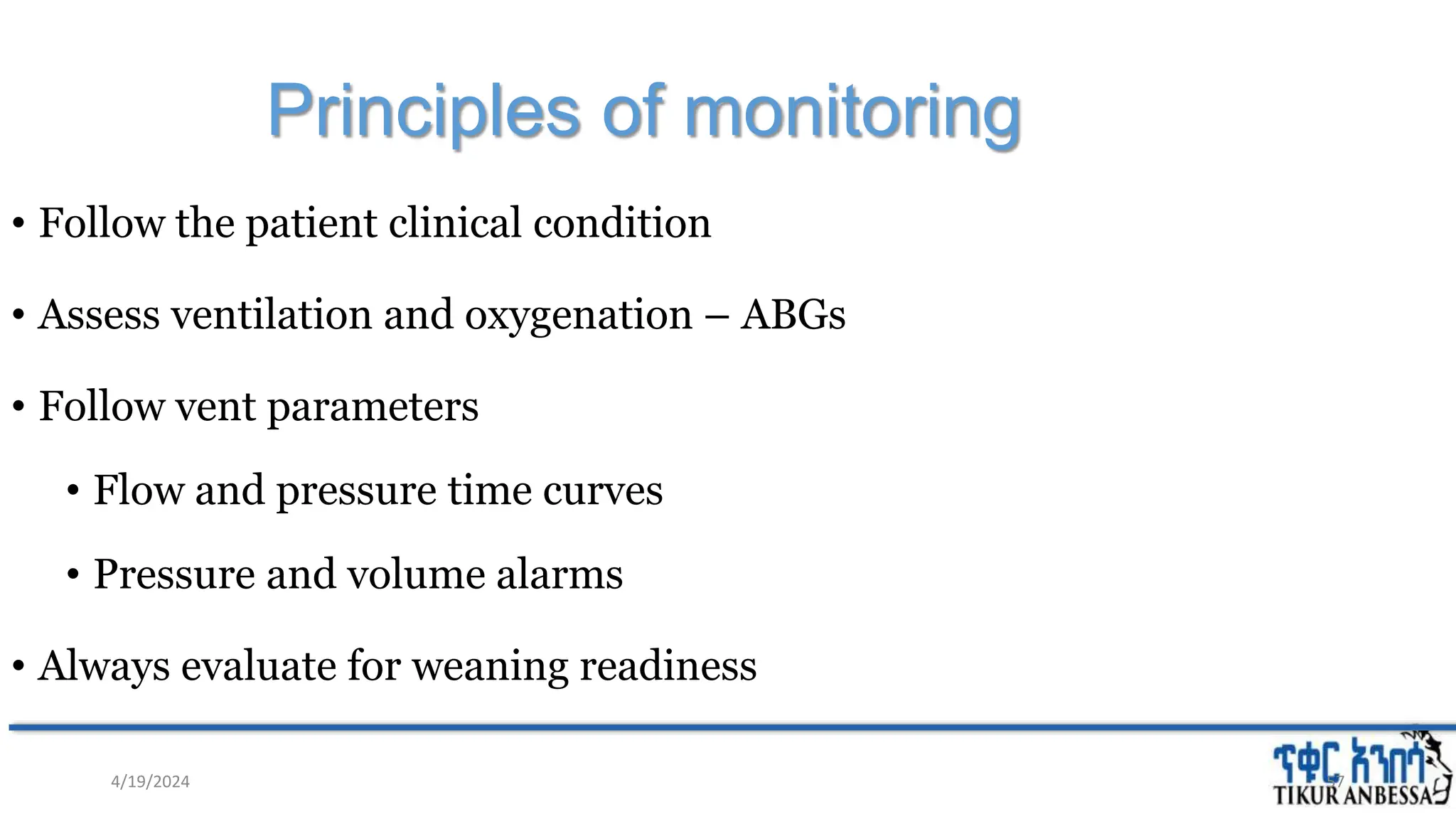
The document discusses mechanical ventilation, outlining its purpose, types, indications, modes, and complications. It details the evolution of ventilatory systems from negative to positive pressure ventilation, alongside various modes such as controlled mechanical ventilation and pressure support. Monitoring, ventilator settings, and the importance of weaning are also highlighted to optimize patient outcomes during mechanical ventilation.



![Oxygen toxicity
• Inappropriate O2 supplementation is deleterious
• Hyperoxia ↑reactive oxygen species (superoxide anion, hydroxyl radical,
H2O2) [+depleted antioxidant system] cellular injury
• There is no single threshold of FiO2 defining a safe upper limit for prevention of
oxygen toxicity.
• Reducing FiO2 to lowest tolerable limit is a good principle for all patients
4/19/2024 64](https://image.slidesharecdn.com/myseminaronmv-240419211539-9af7571b/75/Seminar-on-basics-of-mechanical-ventilation-64-2048.jpg)