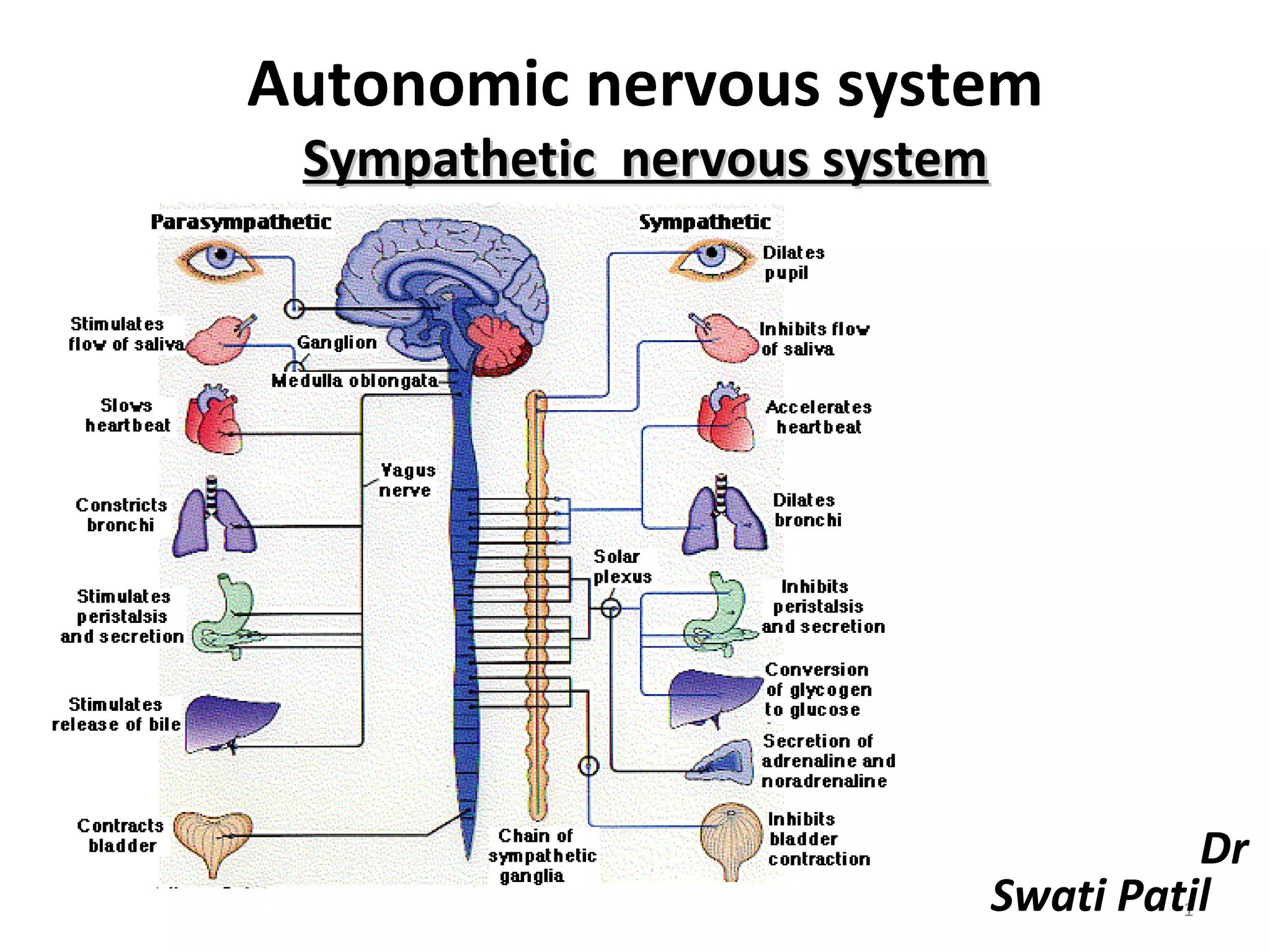
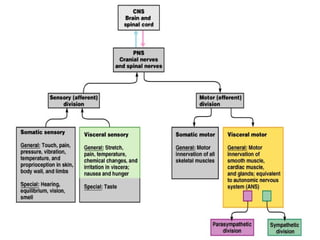
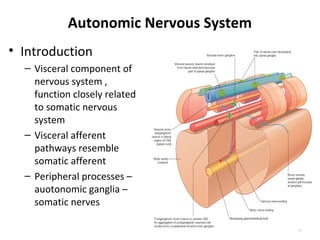
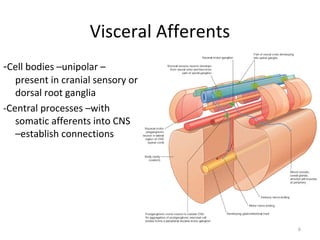
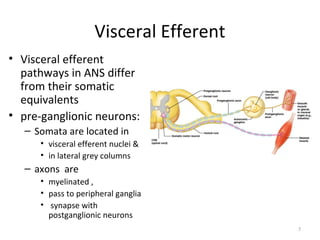
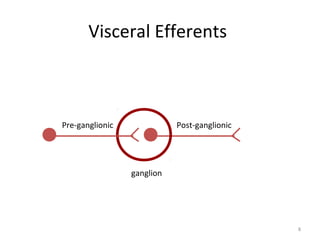
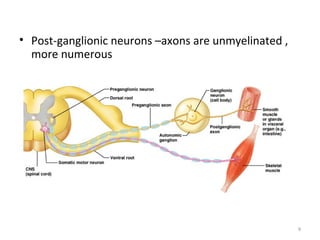
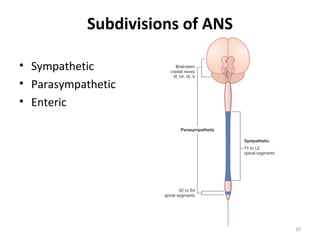
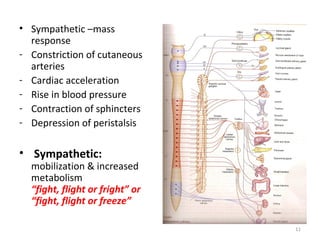
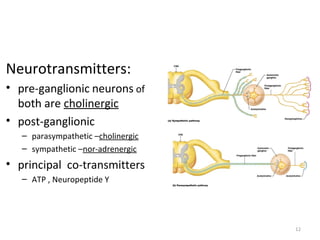
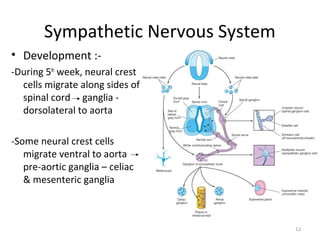
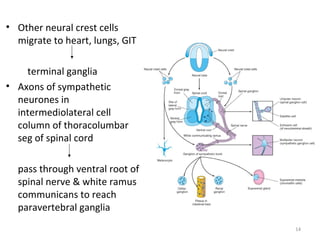
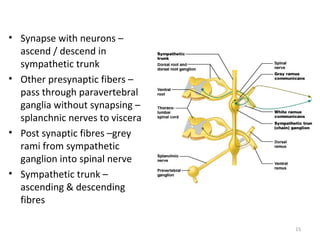
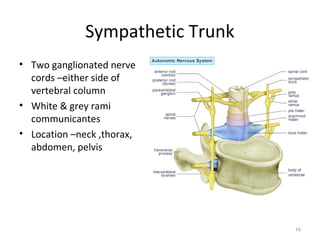
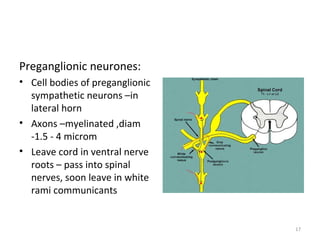
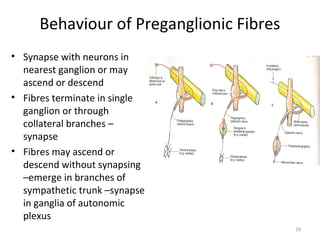
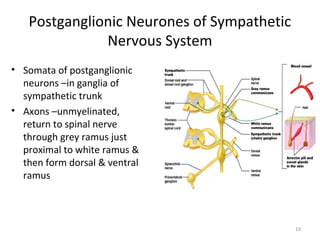
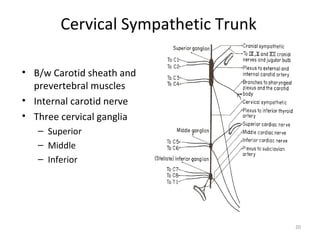
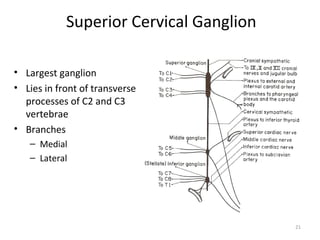
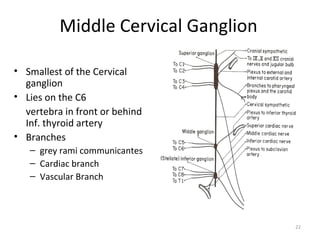
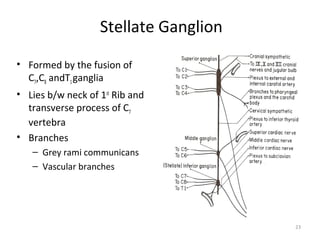
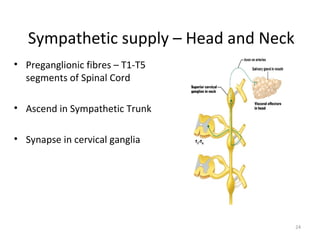
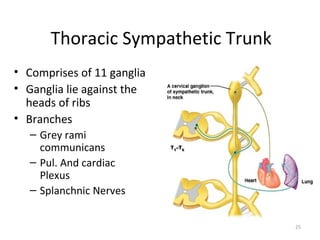
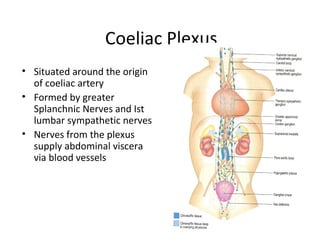
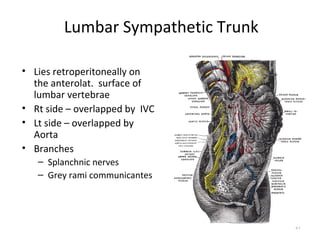
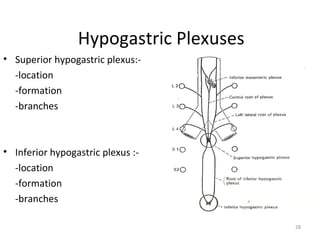
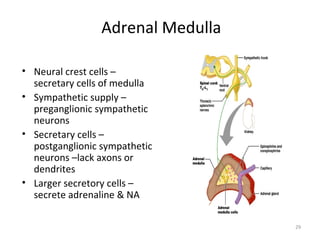
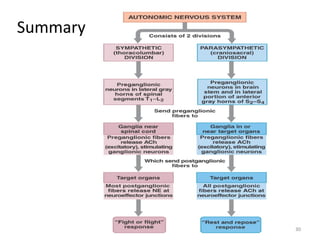
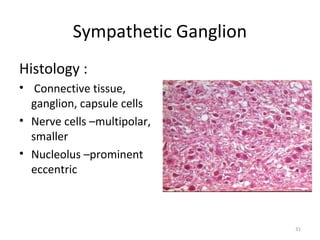
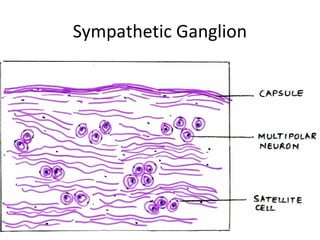
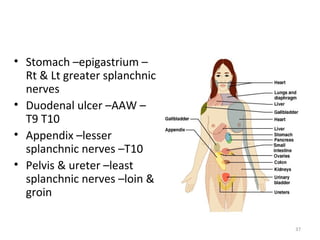
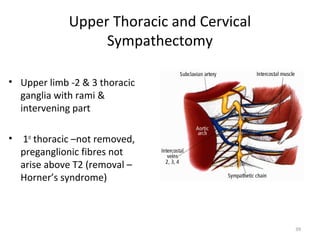
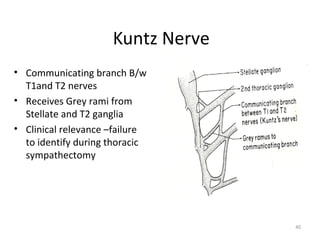
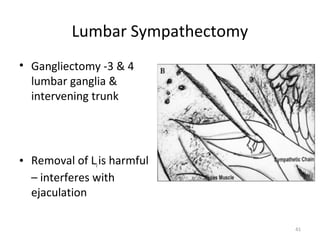
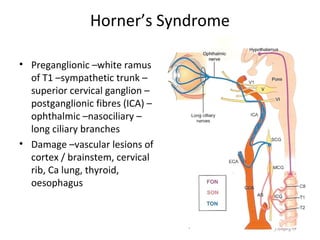
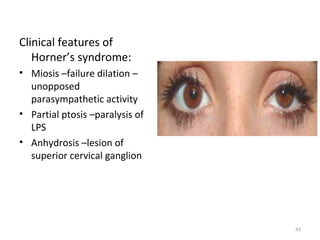
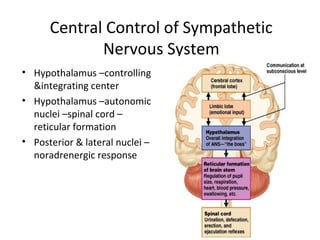
The document provides an overview of the autonomic nervous system, with a focus on the sympathetic nervous system. It discusses the history and subdivisions of the autonomic nervous system. For the sympathetic nervous system specifically, it describes the development of ganglia from neural crest cells, the pathways of preganglionic and postganglionic neurons, and the locations and branches of sympathetic ganglia along the spinal cord and for different organ systems. It also reviews histology of ganglia, surgical sympathectomy procedures, and Horner's syndrome.