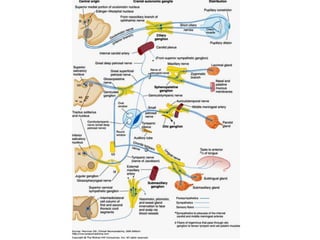
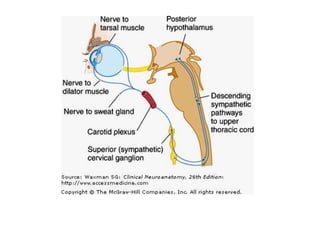
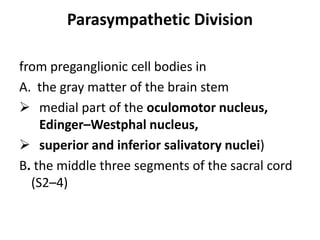
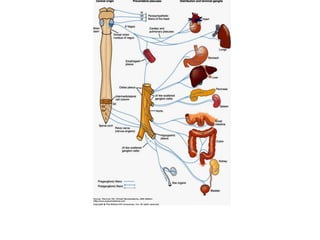
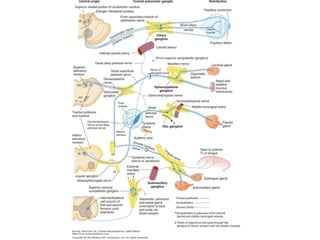
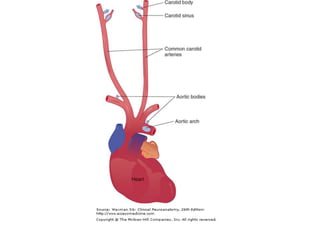
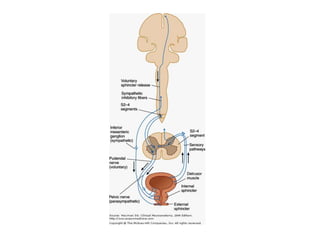
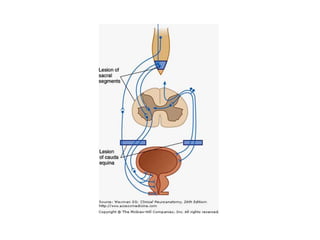
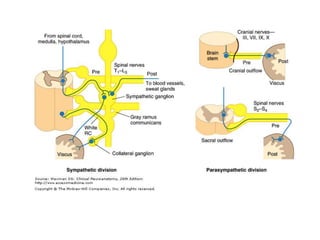
The autonomic nervous system consists of sympathetic and parasympathetic divisions that regulate organs through two-neuron chains. The sympathetic division originates in the spinal cord and targets organs like the heart and blood vessels. The parasympathetic division originates in the brainstem and sacral spinal cord and targets the digestive system. Sensory fibers carry visceral sensation to the CNS while the autonomic plexuses distribute efferent fibers to target organs.

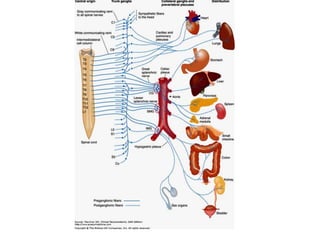
![• Vasomotor branches from the upper five
thoracic ganglia →thoracic aorta → posterior
pulmonary plexus→bronchi[dilatation]](https://image.slidesharecdn.com/ans-120330114051-phpapp02/85/Autonomic-nervous-system-by-DR-ARSHAD-28-320.jpg)