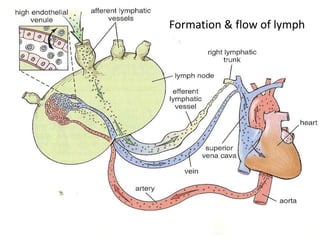
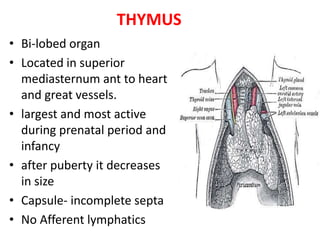
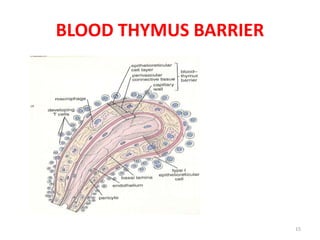
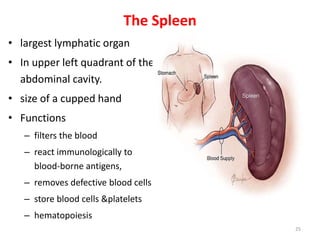
The lymphatic system consists of lymph, lymph nodes, lymph vessels, the spleen, thymus, tonsils, bone marrow and skin-associated lymphoid tissues. The main cells of the lymphatic system are lymphocytes such as B cells, T cells, natural killer cells, and supporting cells that interact with and present antigens to lymphocytes. The lymphatic system protects the body from foreign materials, assists in fluid circulation, and transports dietary fats. The thymus gland aids in the maturation of T cells while the spleen filters blood and mounts an immune response to antigens. Lymph nodes are located around arteries and veins and filter lymph fluid draining tissues.