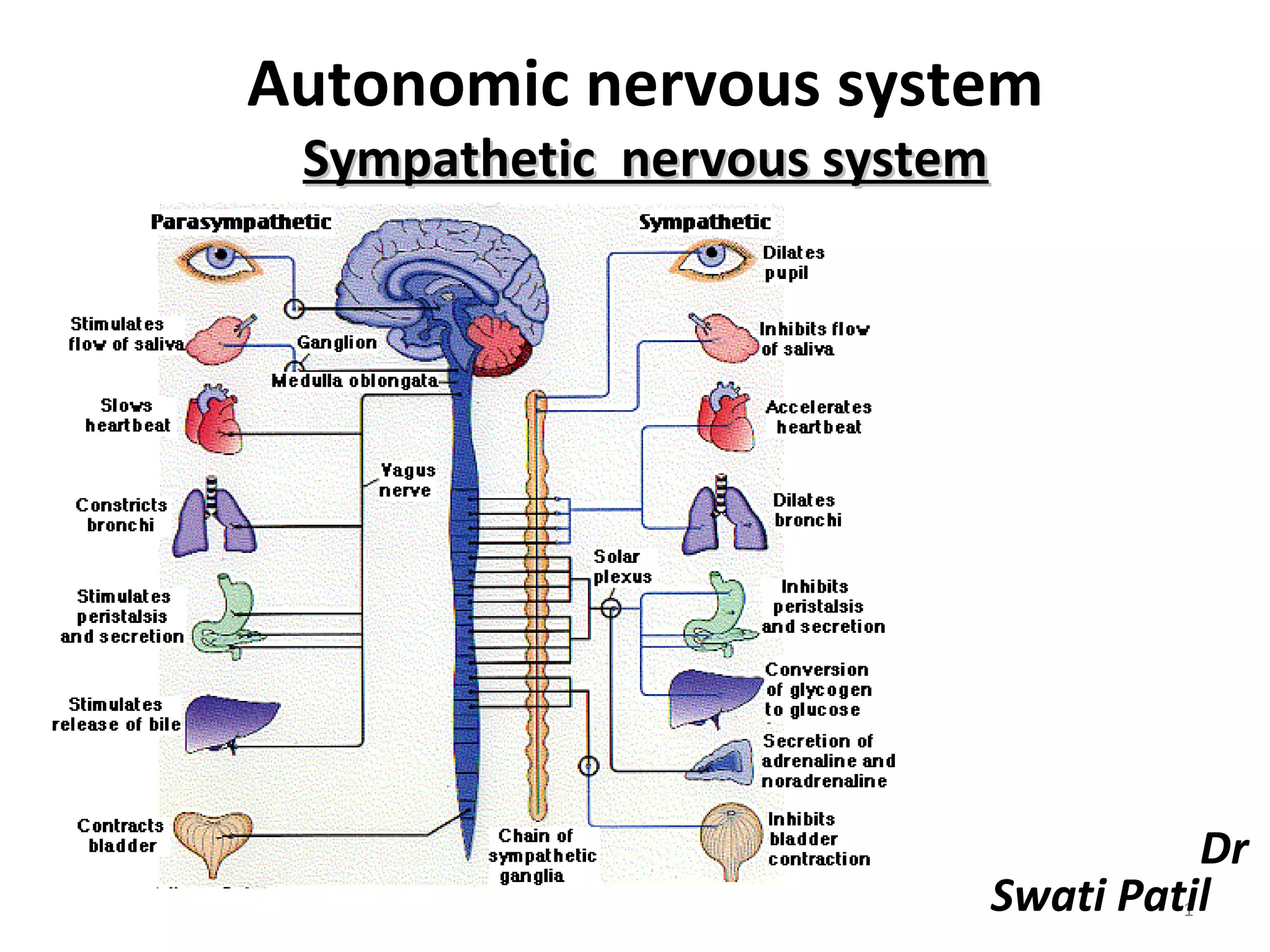
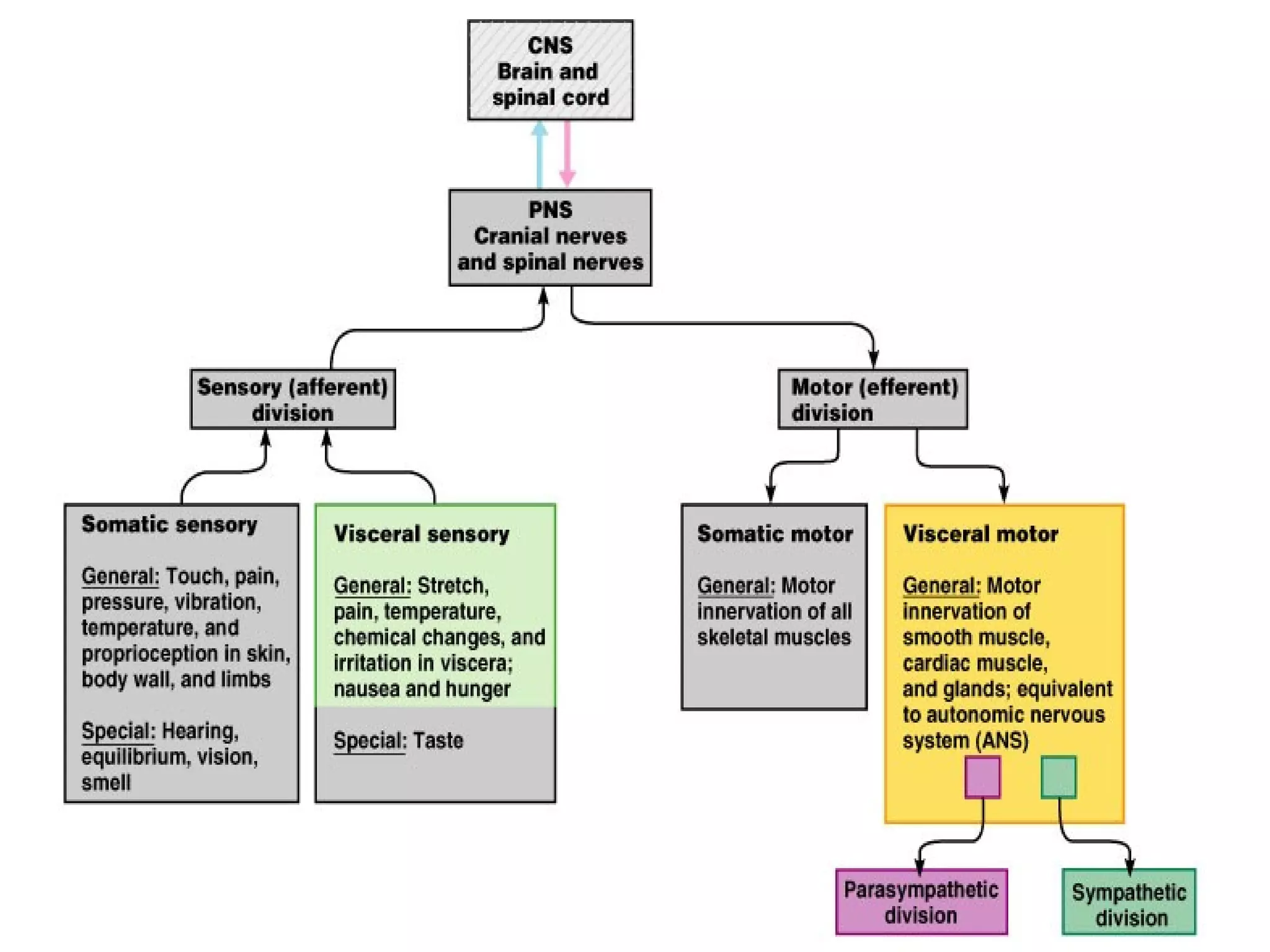
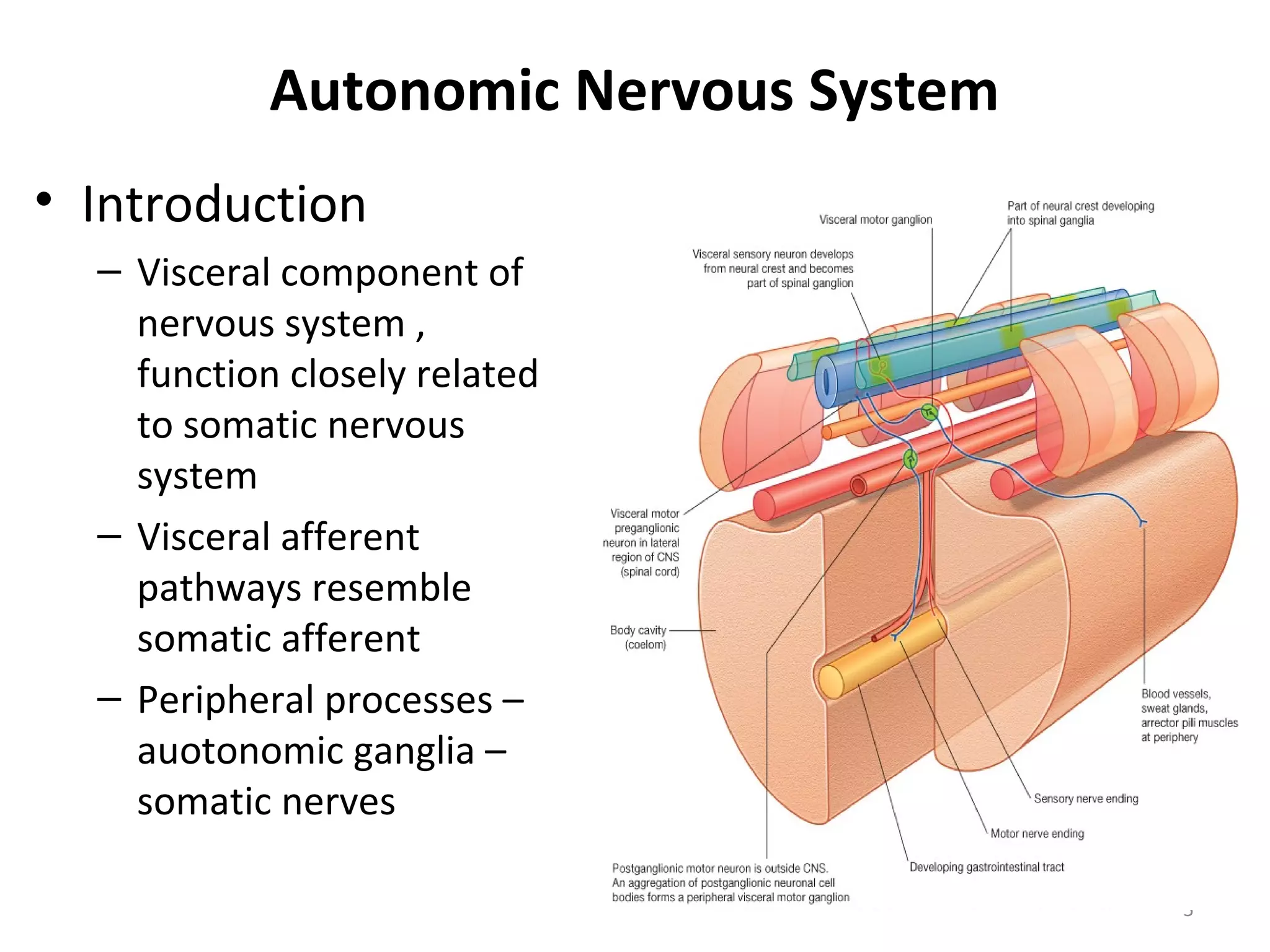
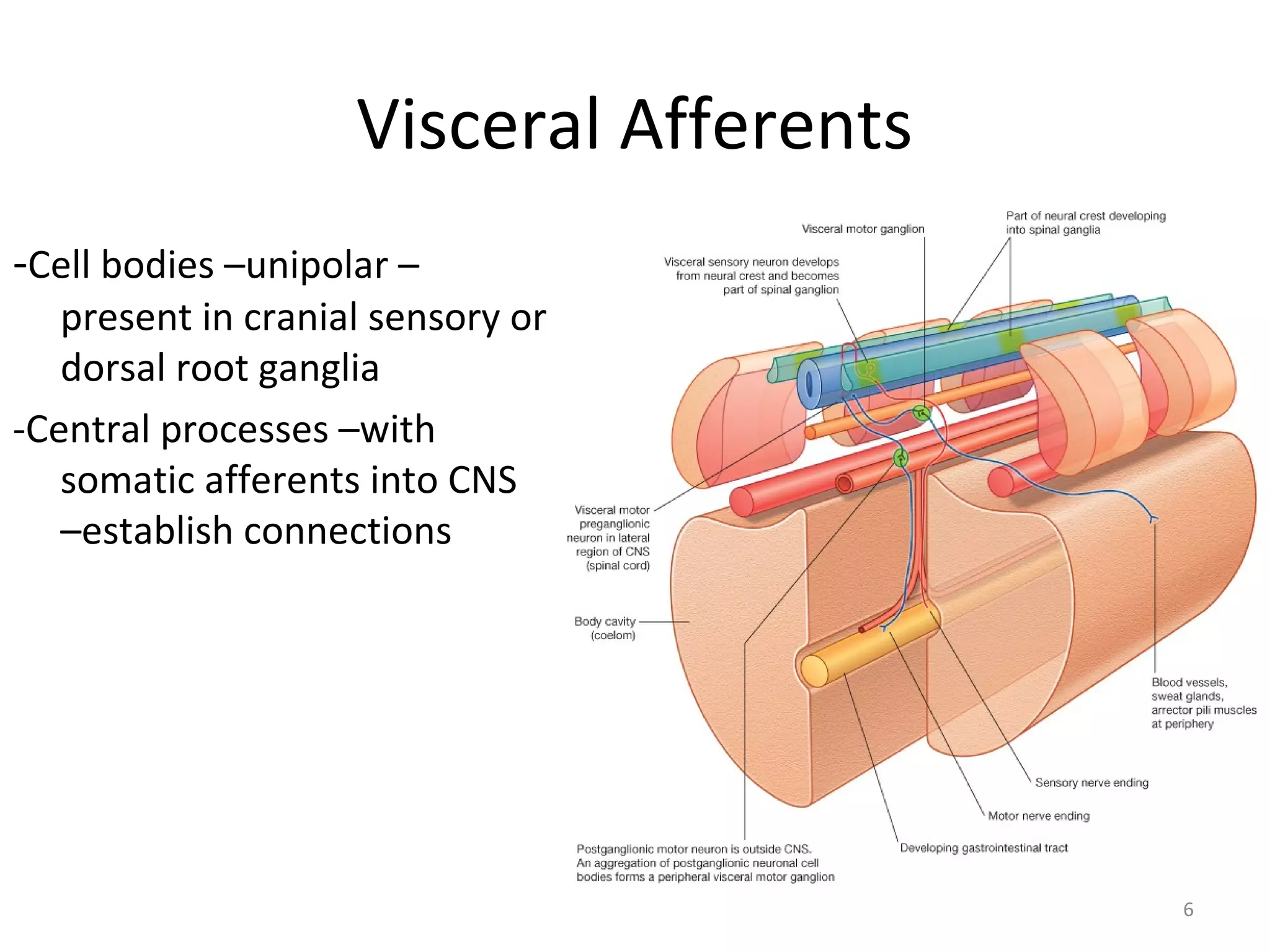
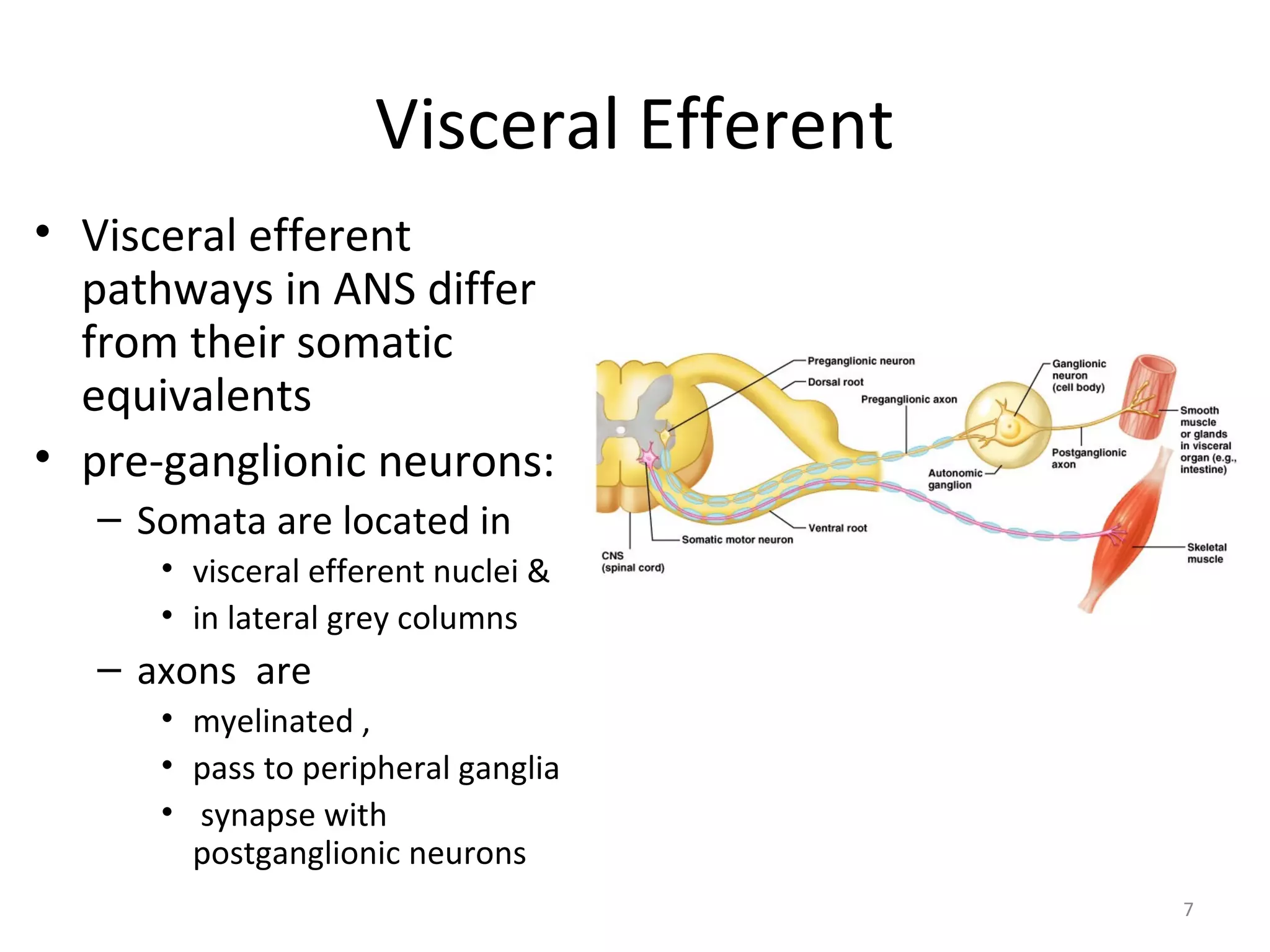
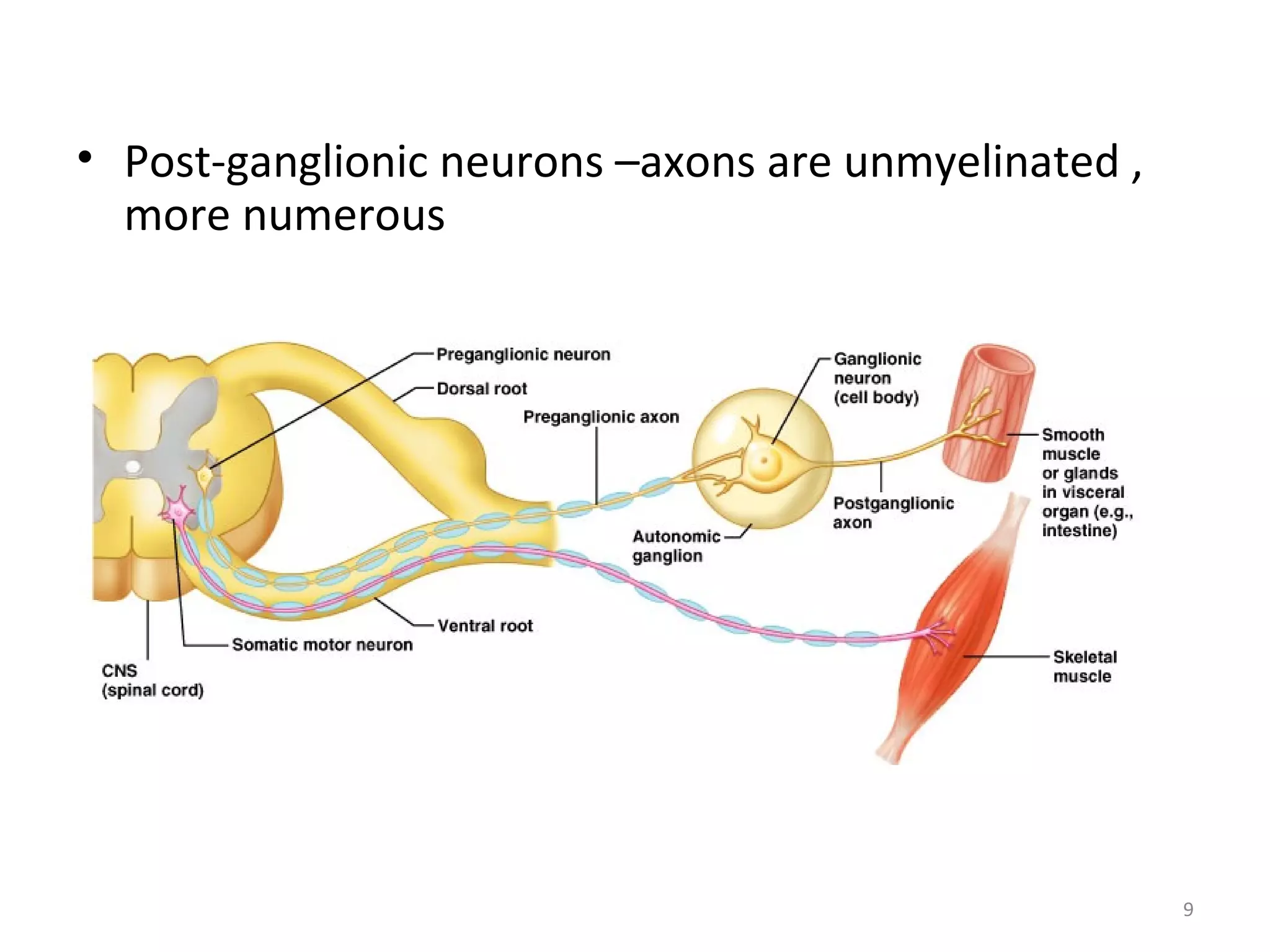
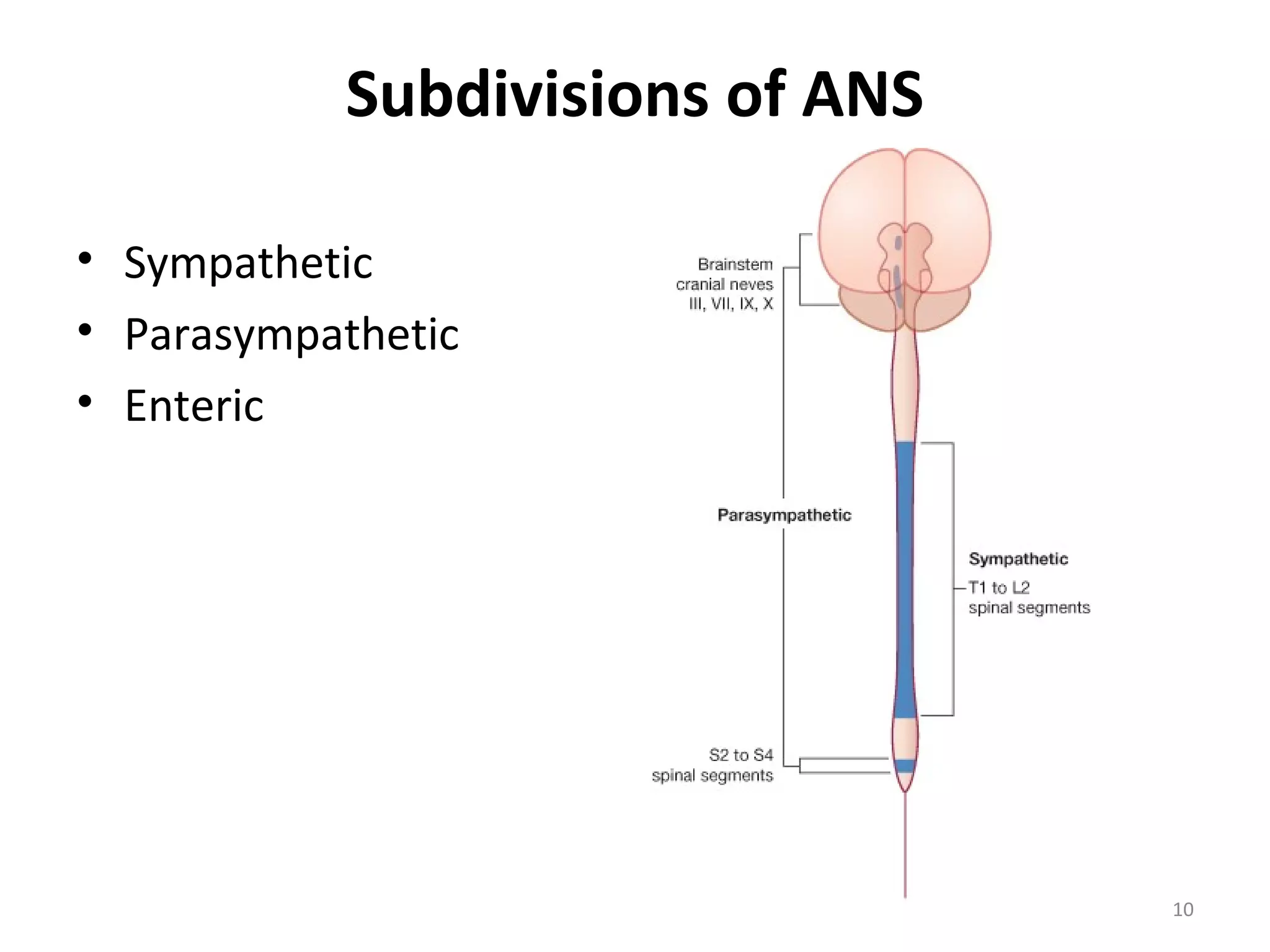
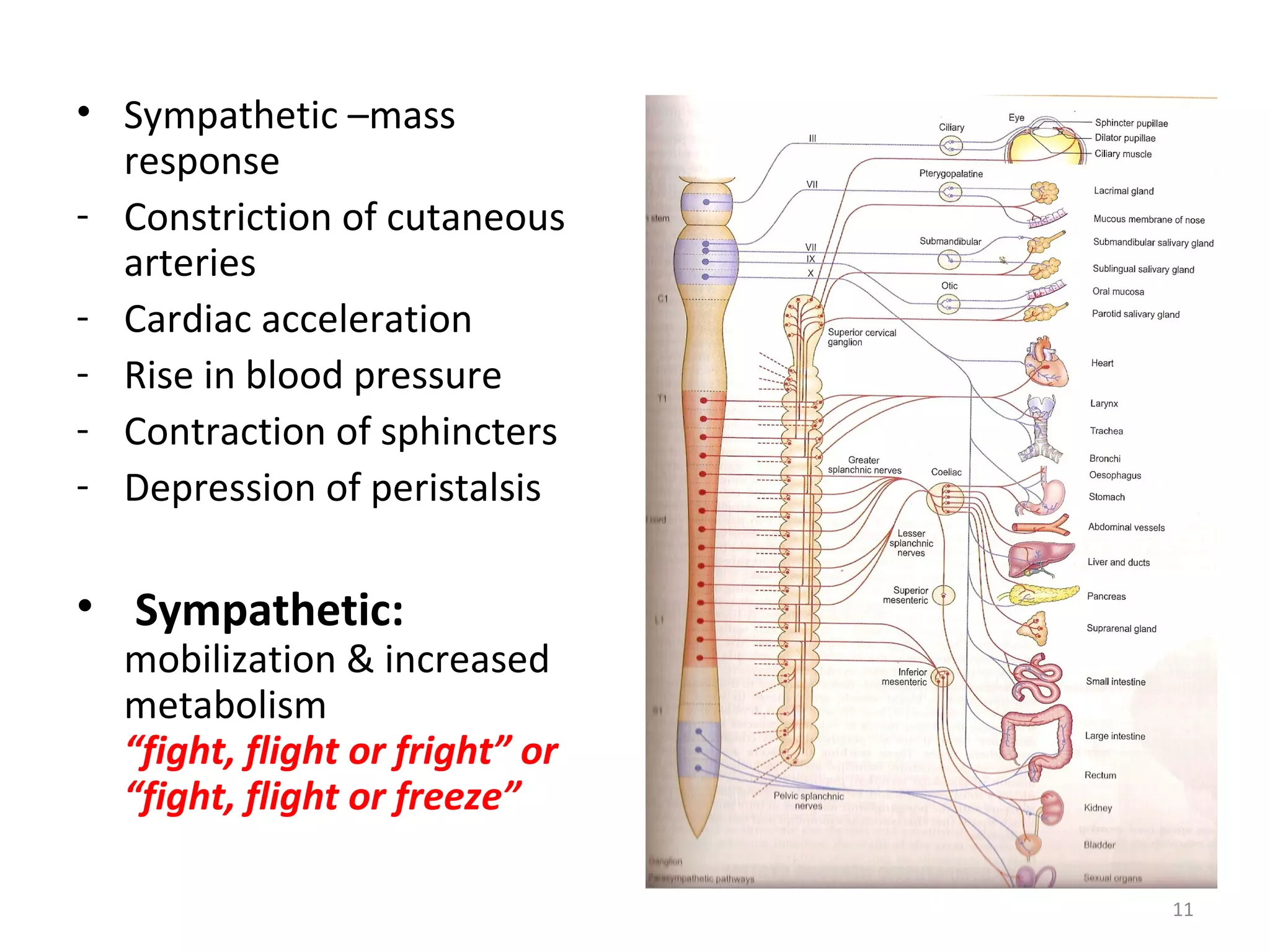
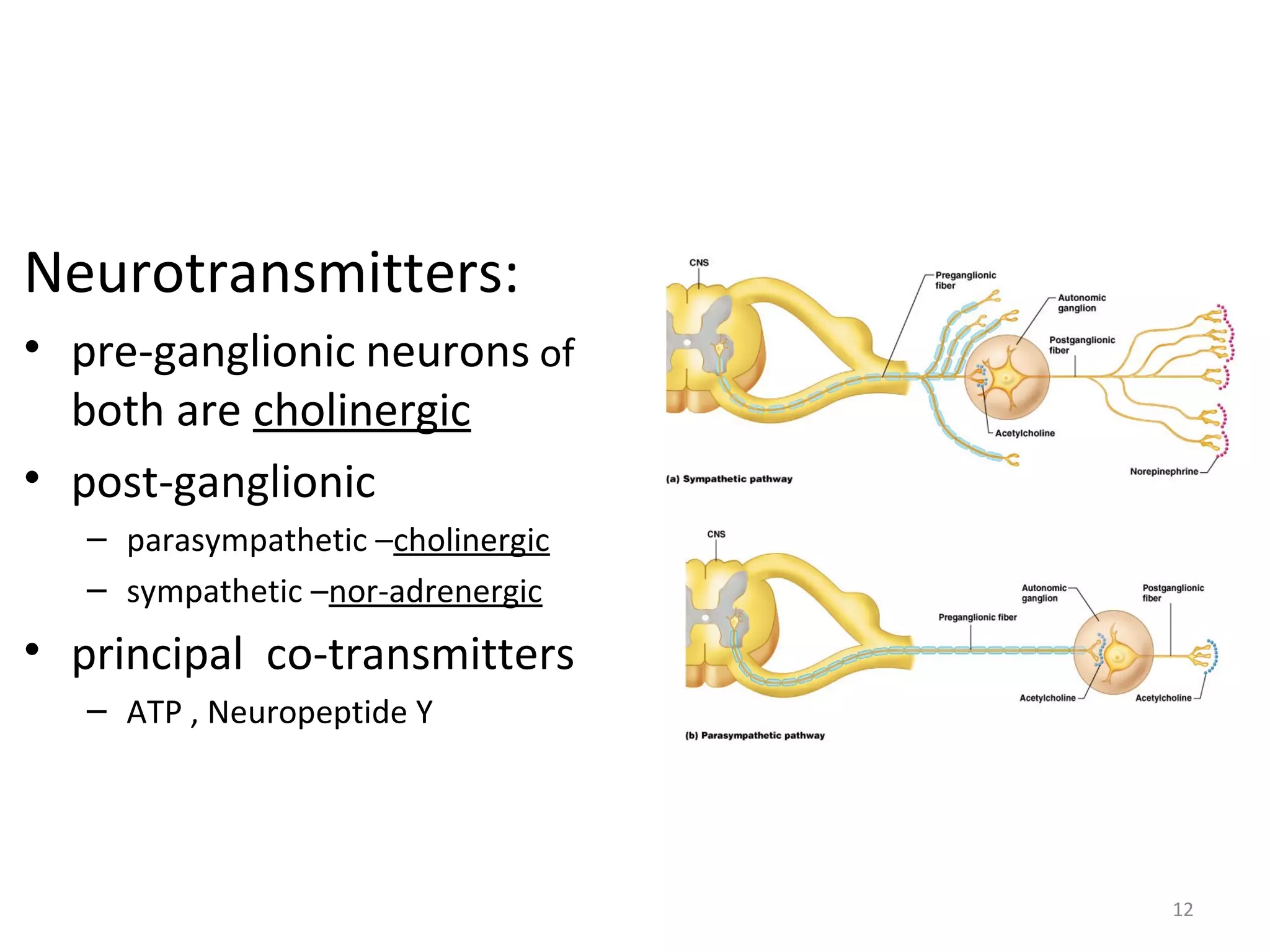
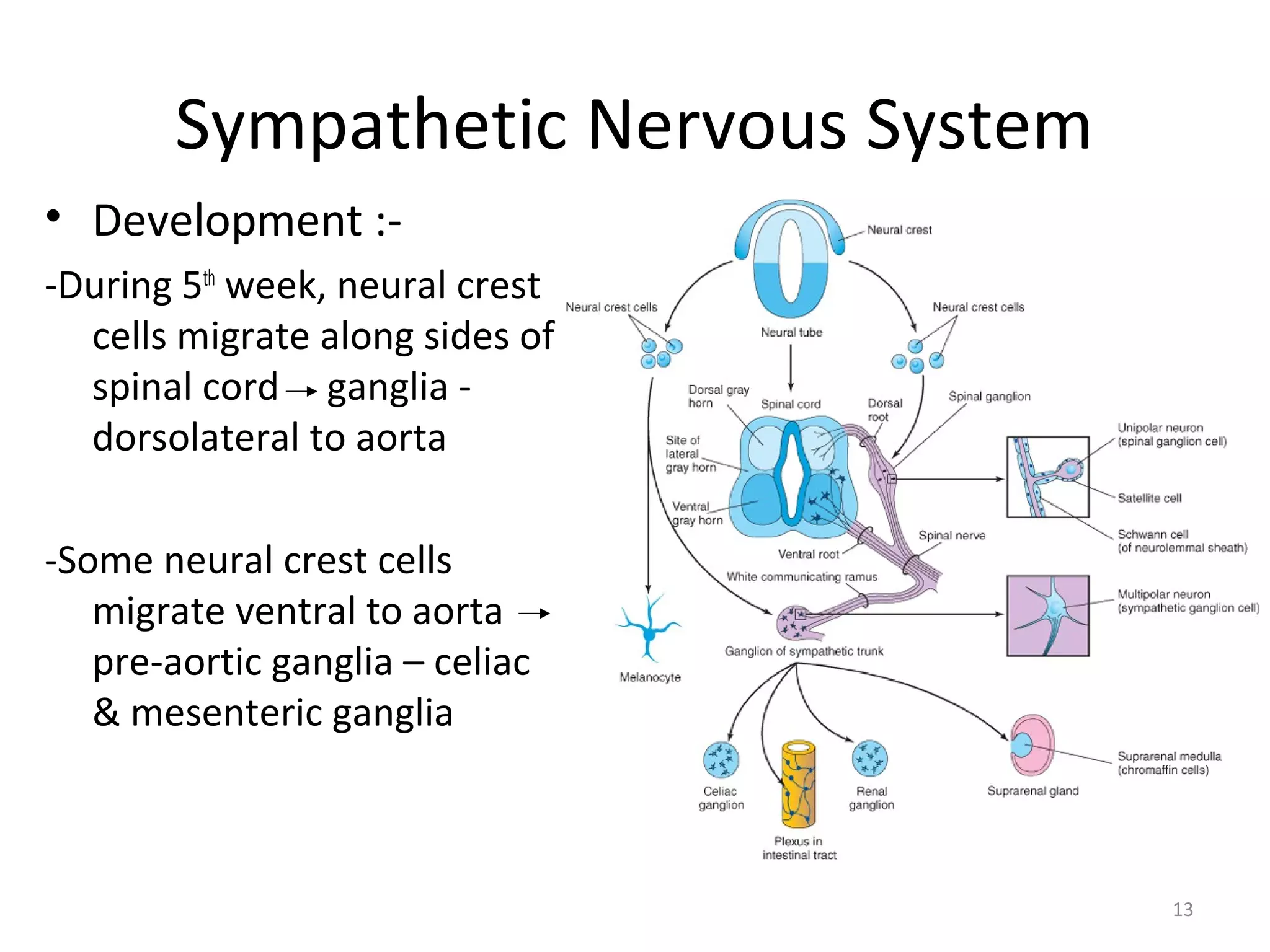
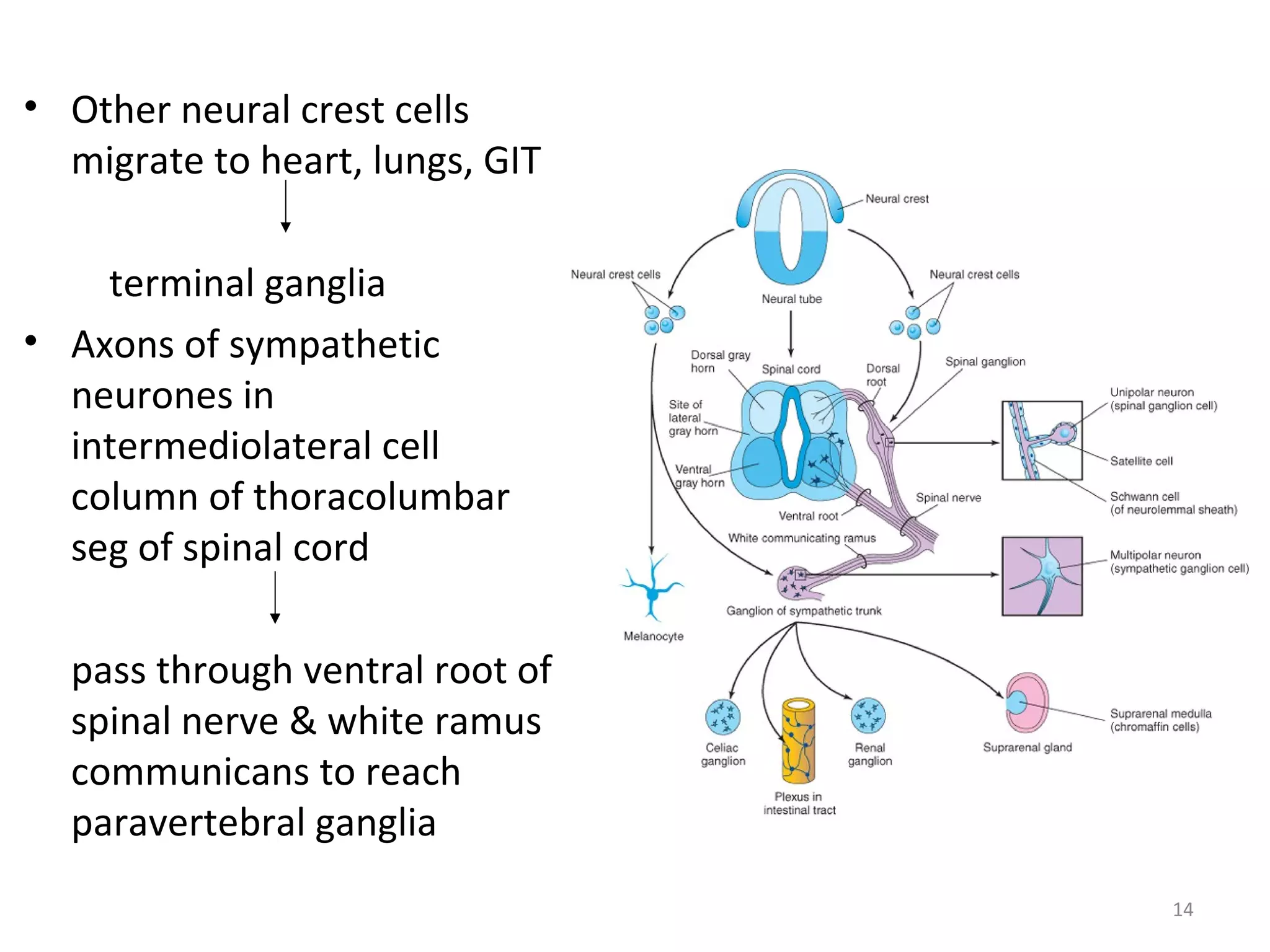
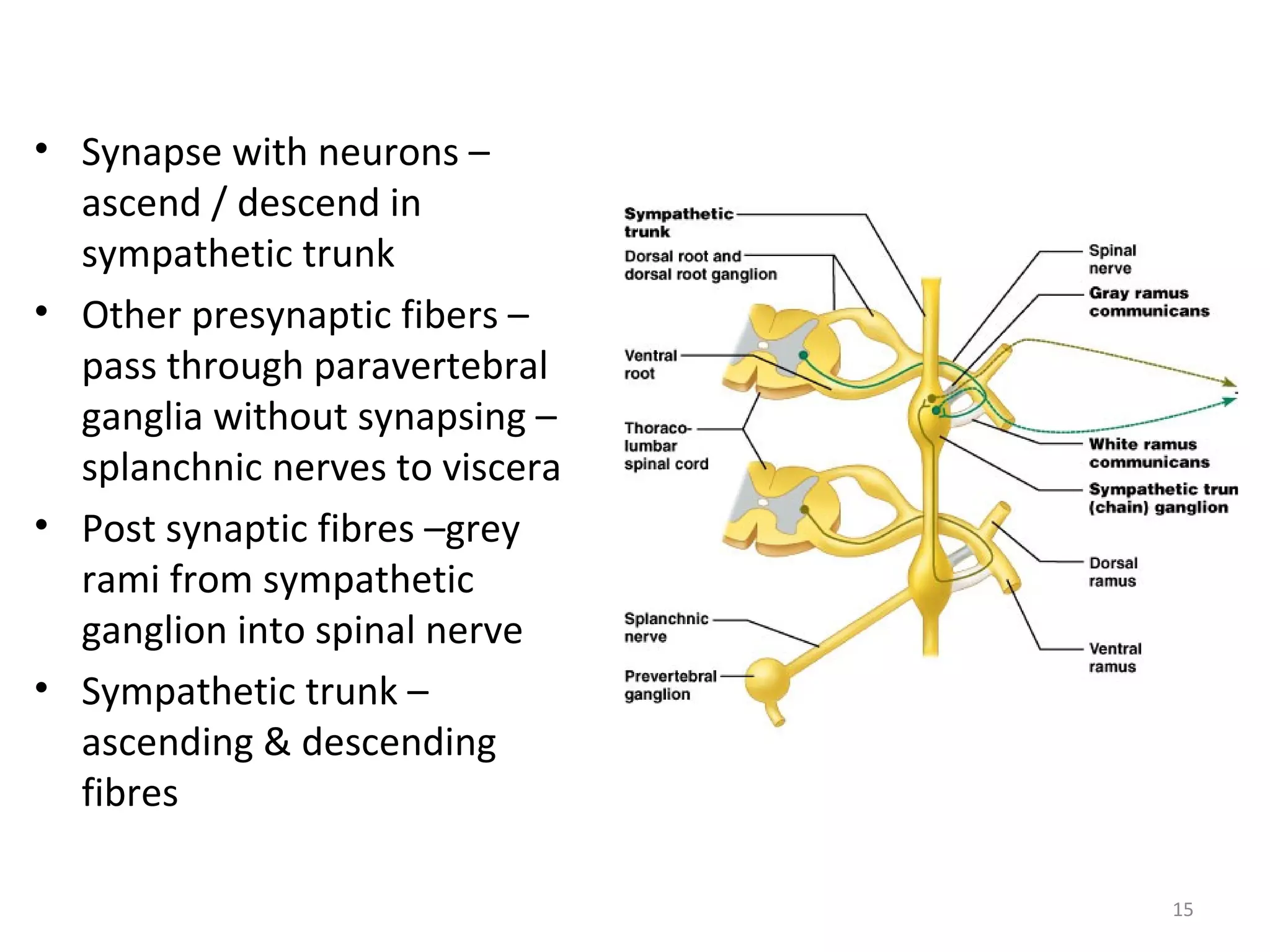
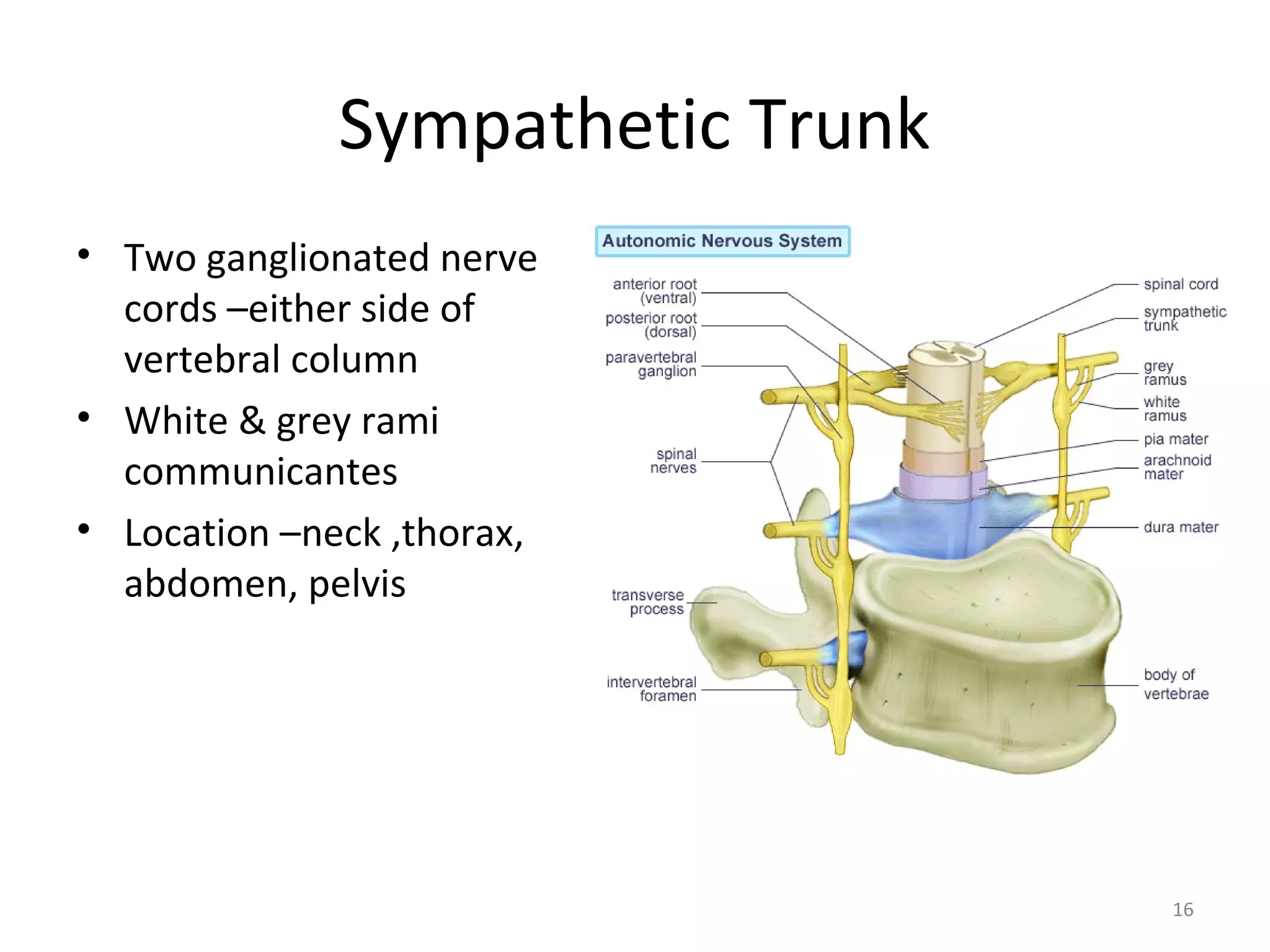
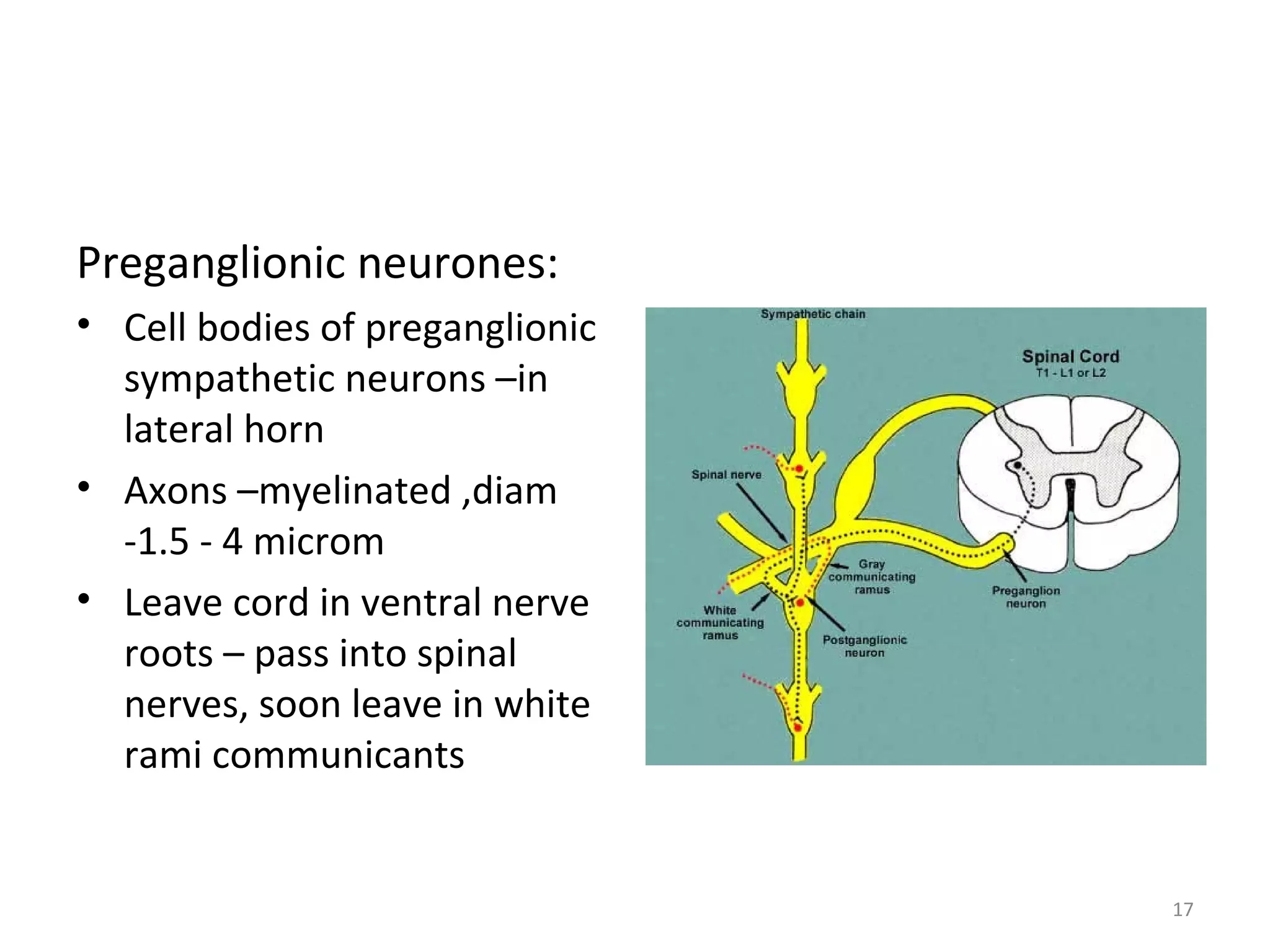
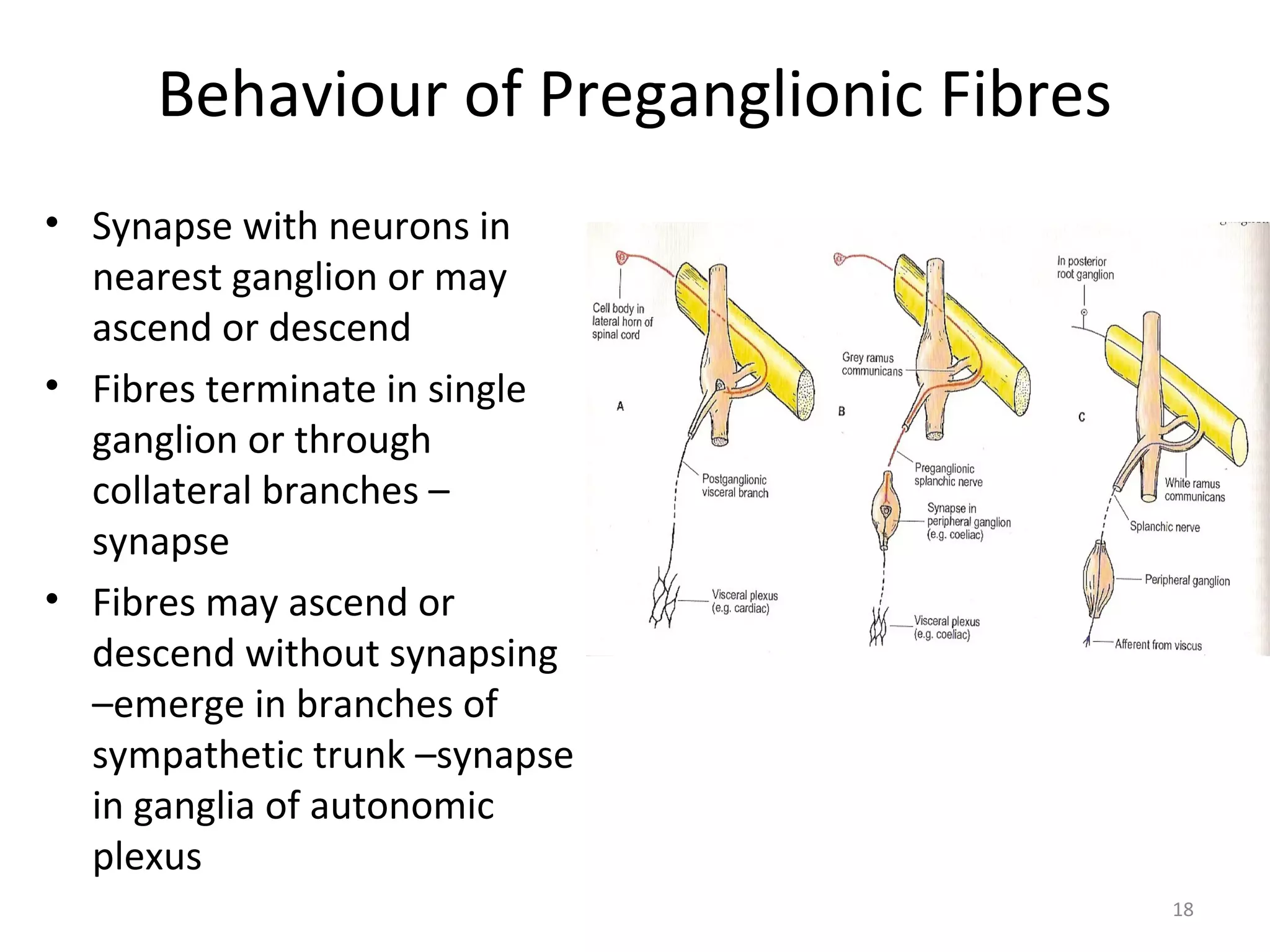
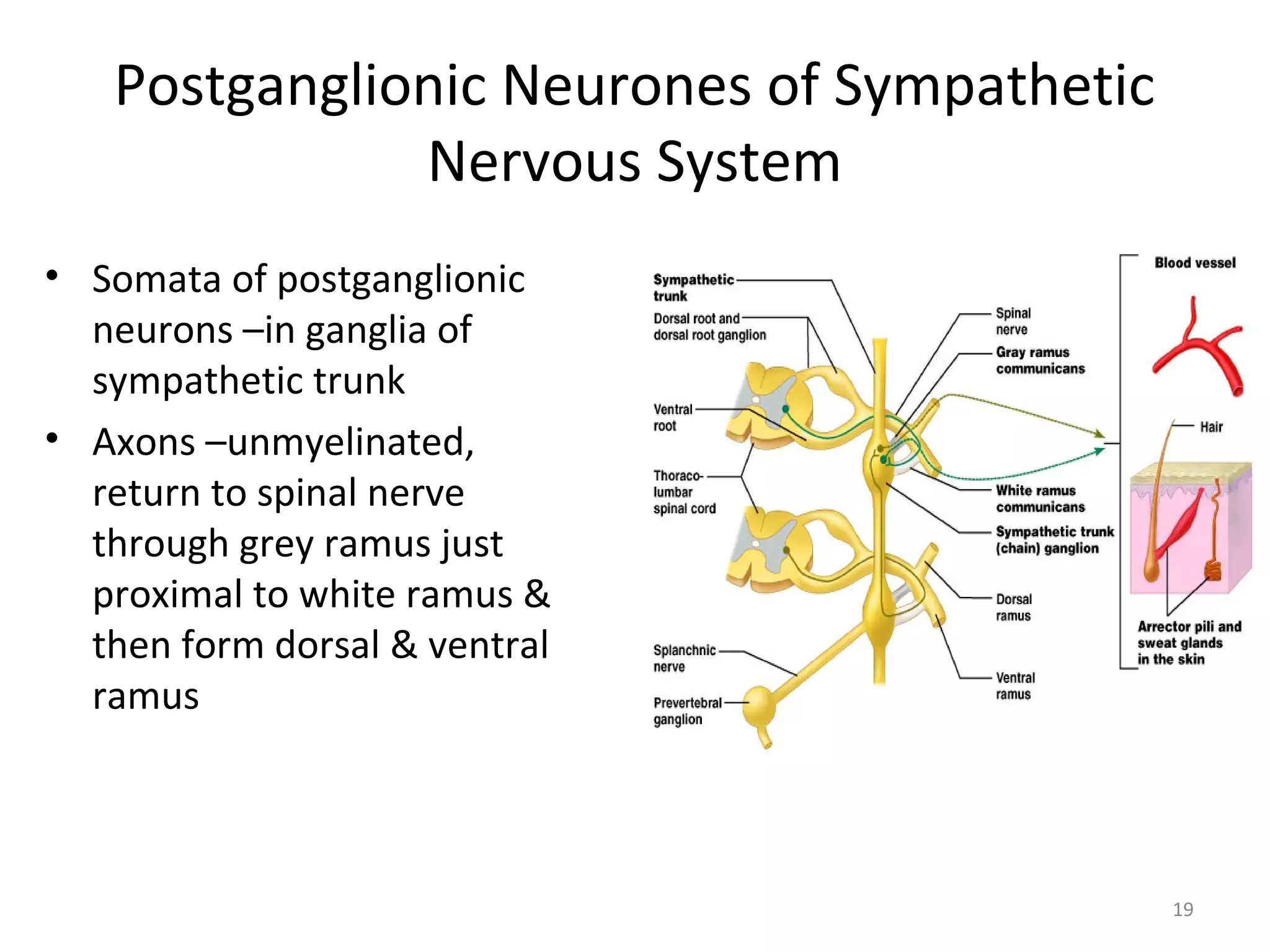
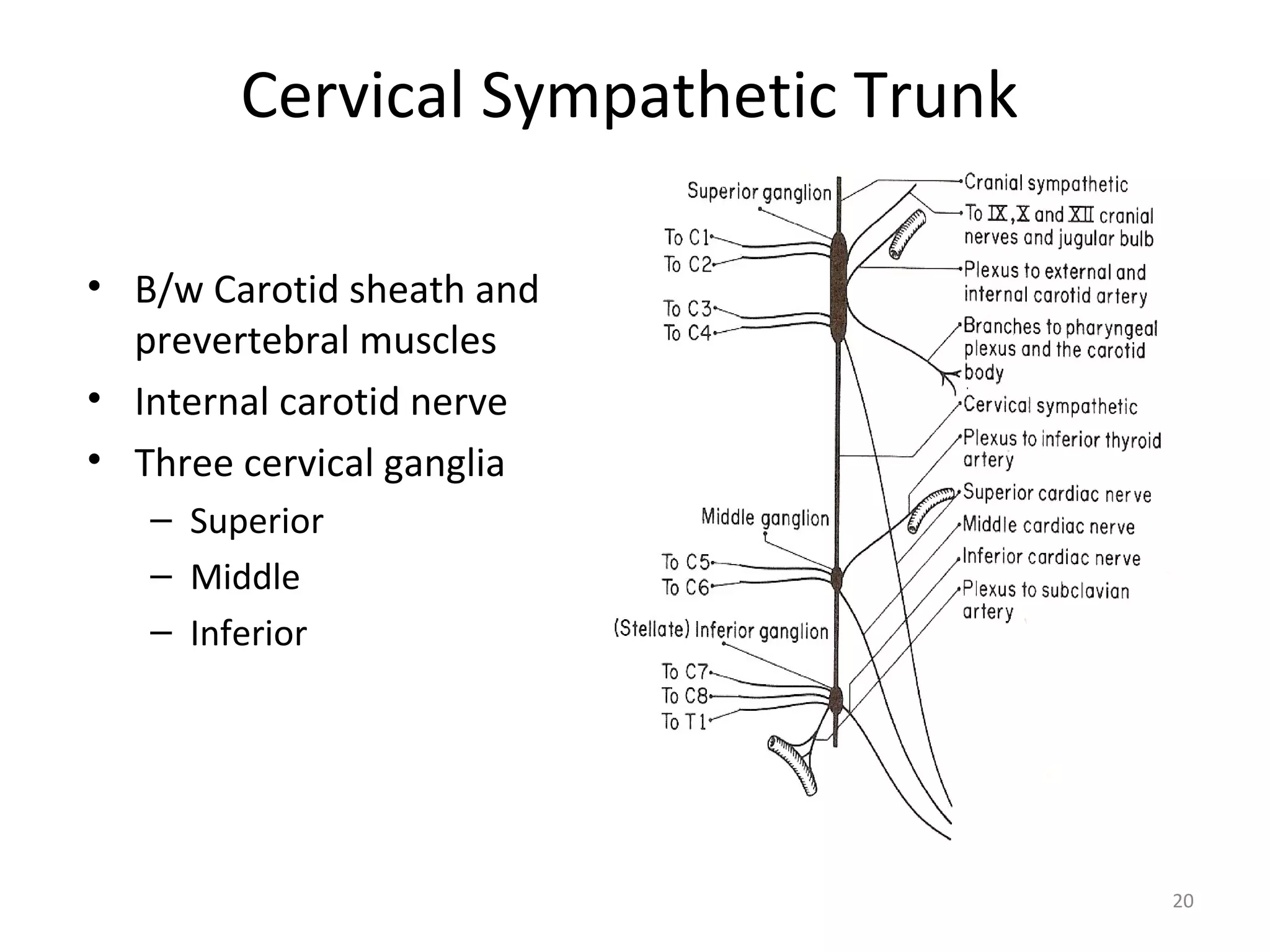
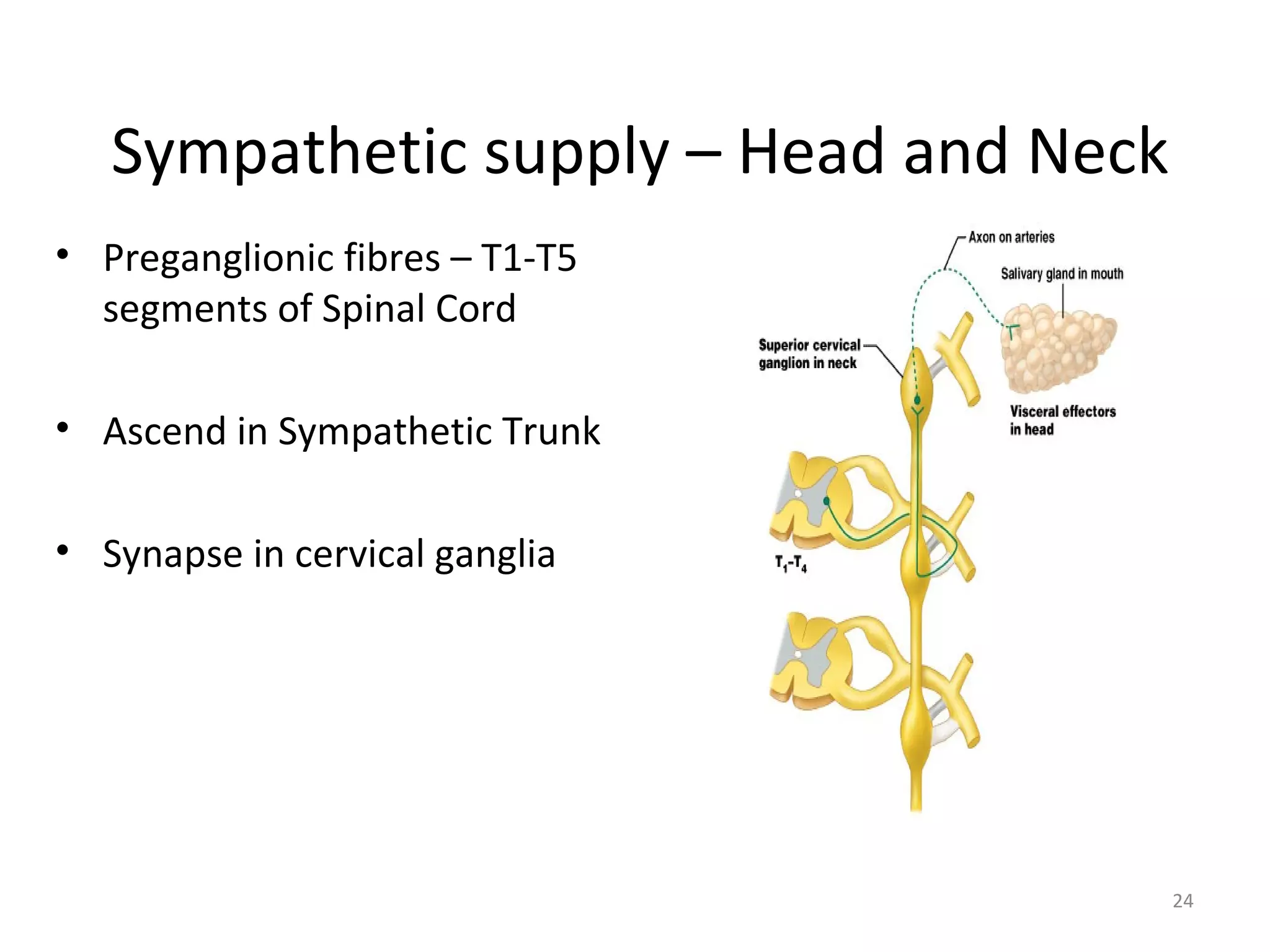
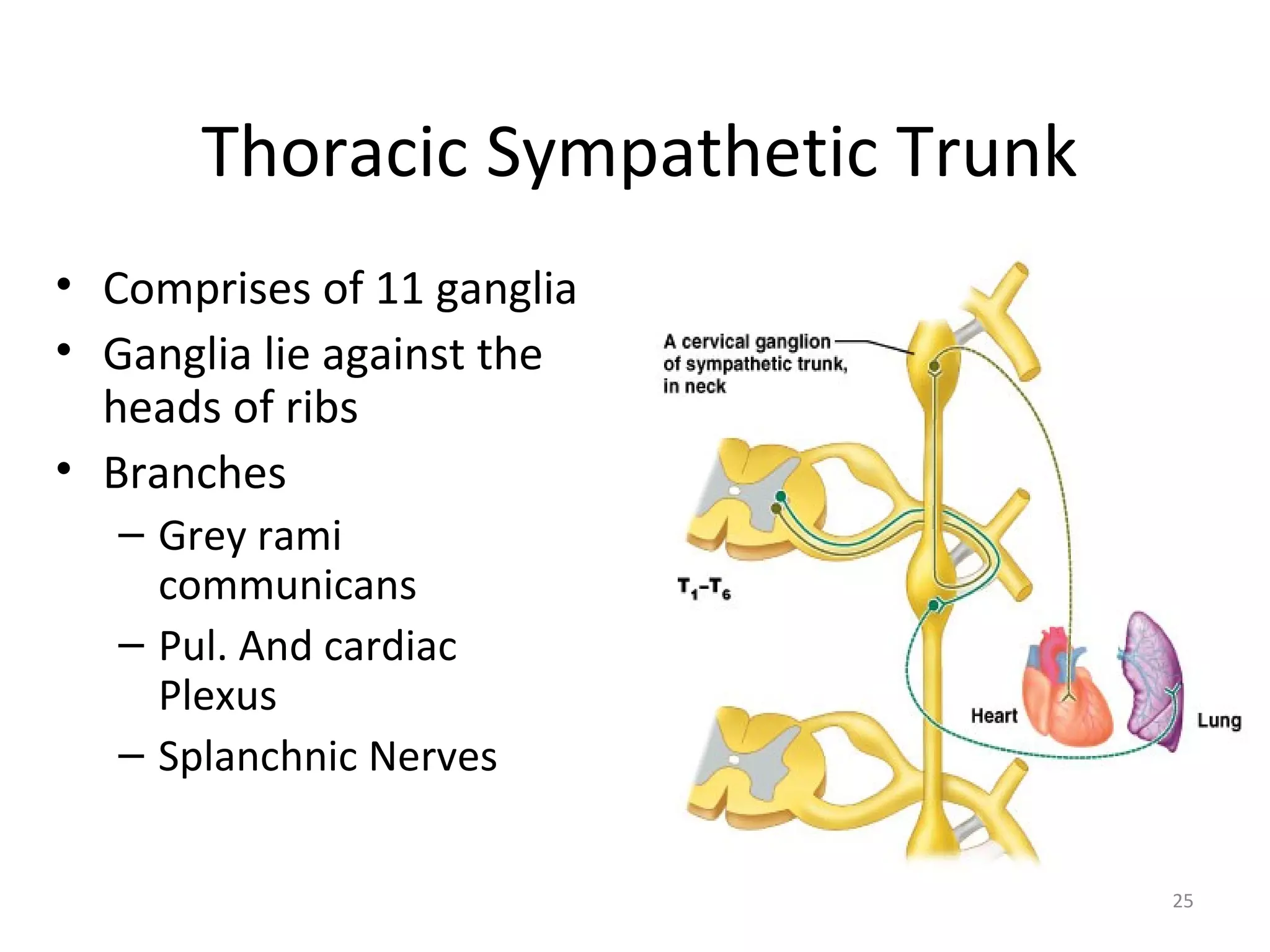
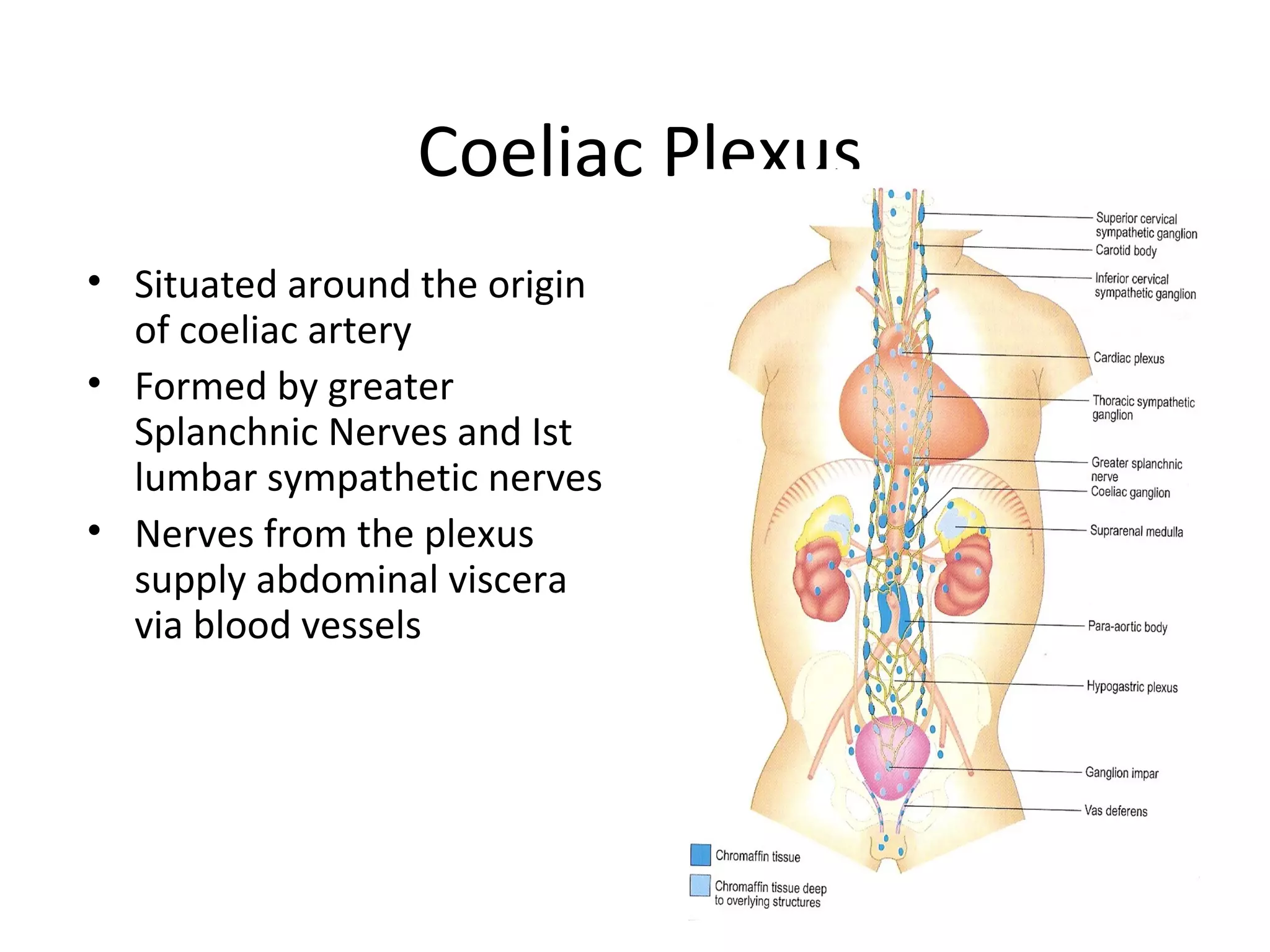
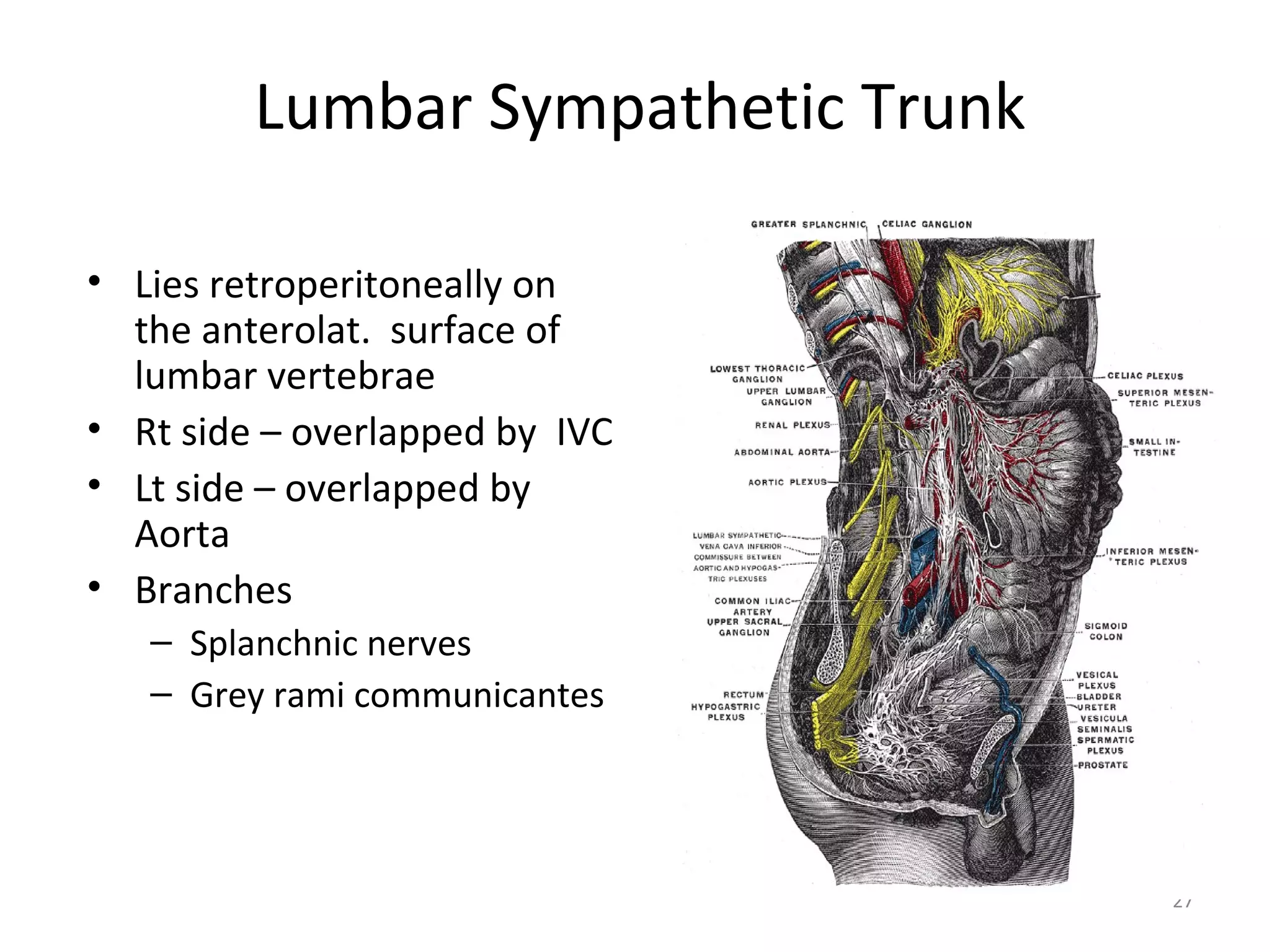
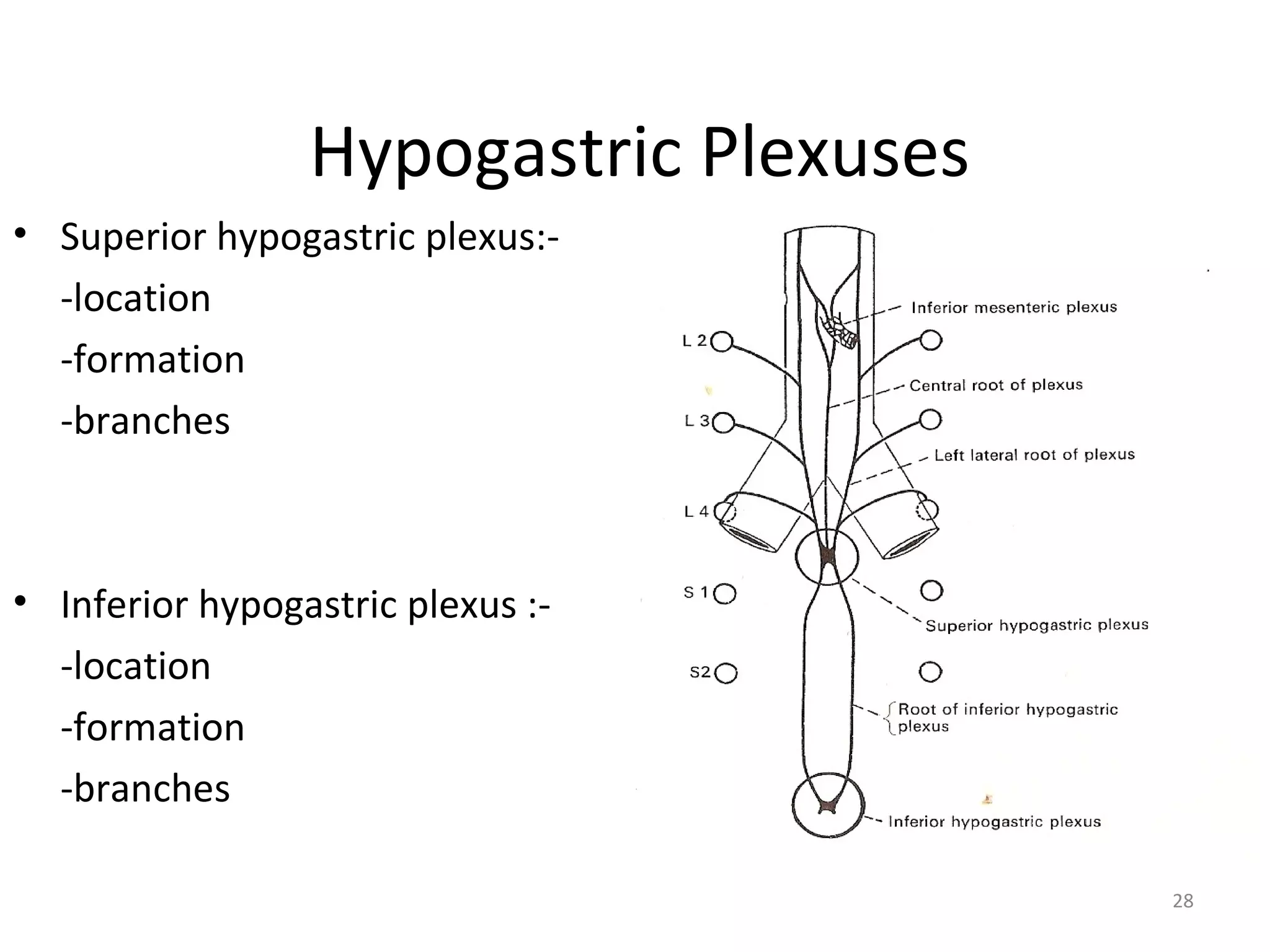
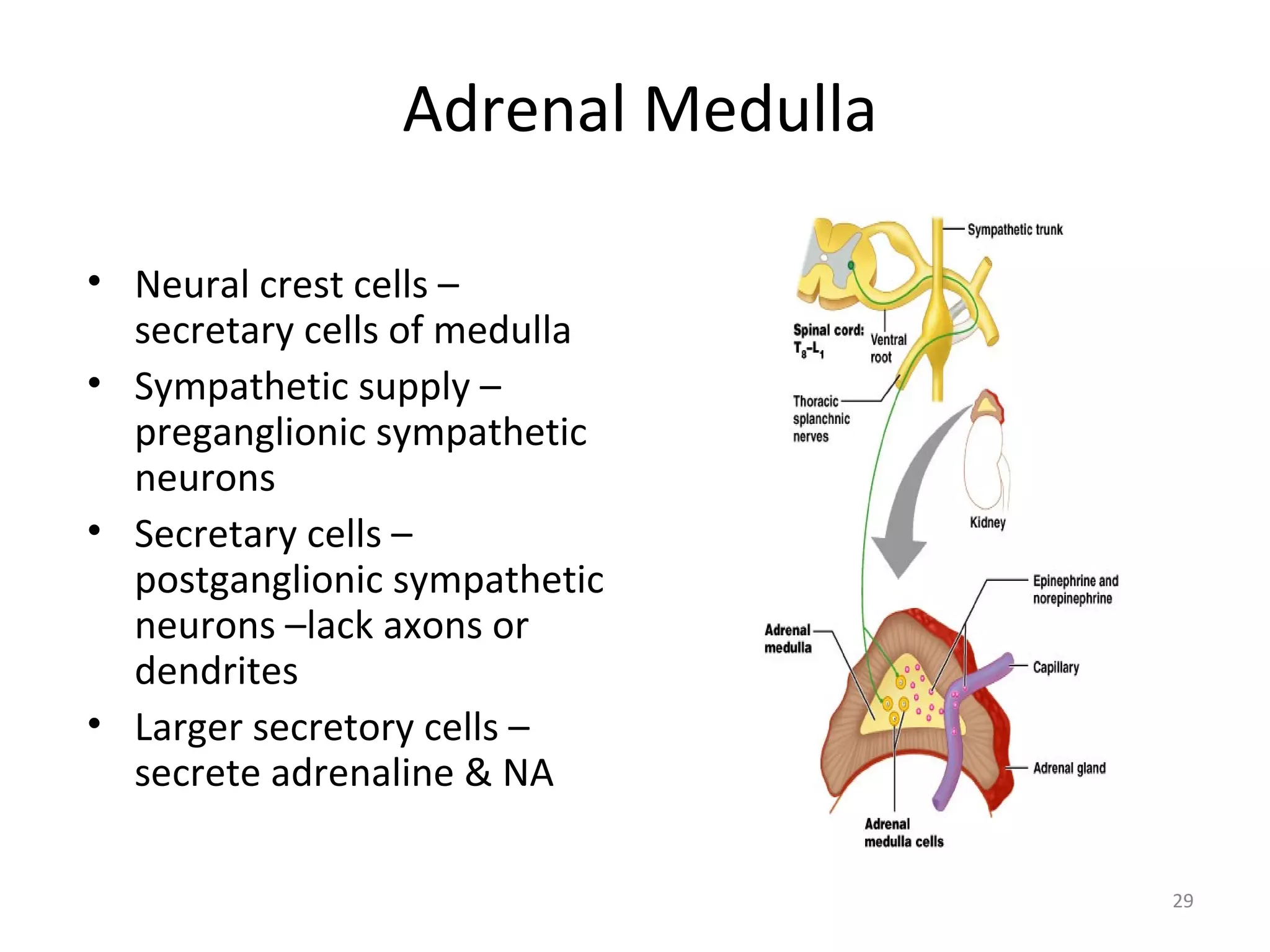
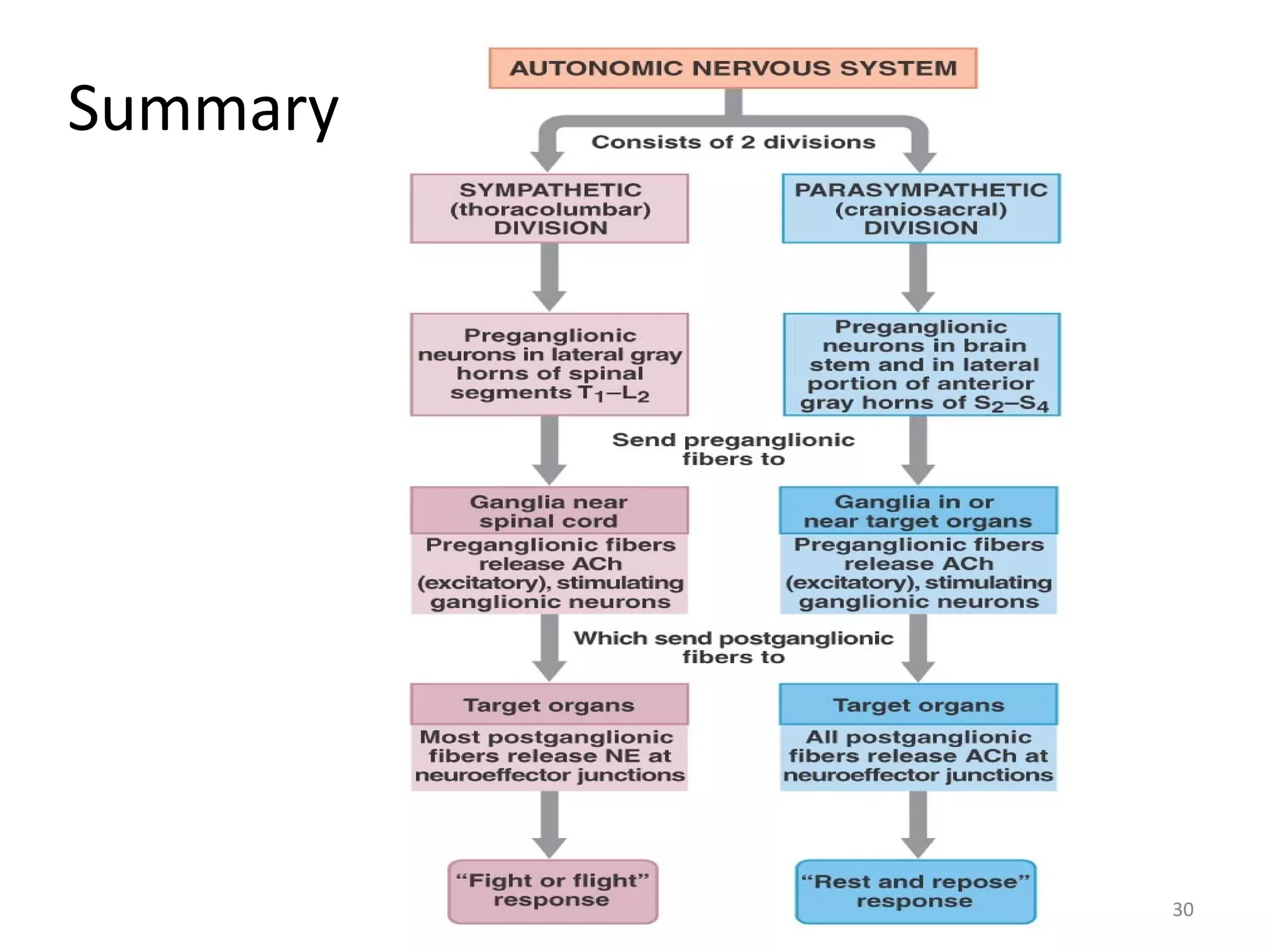
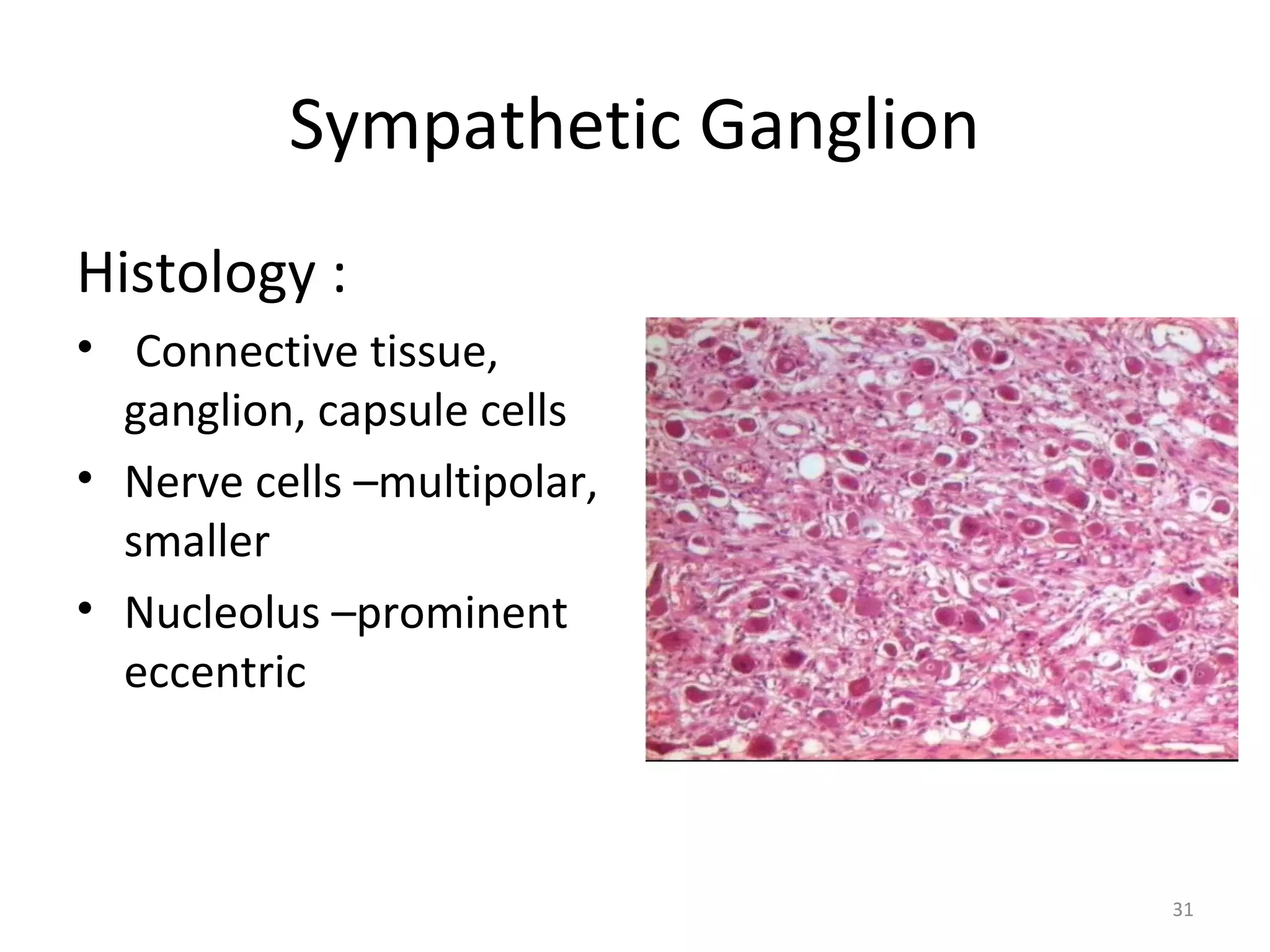
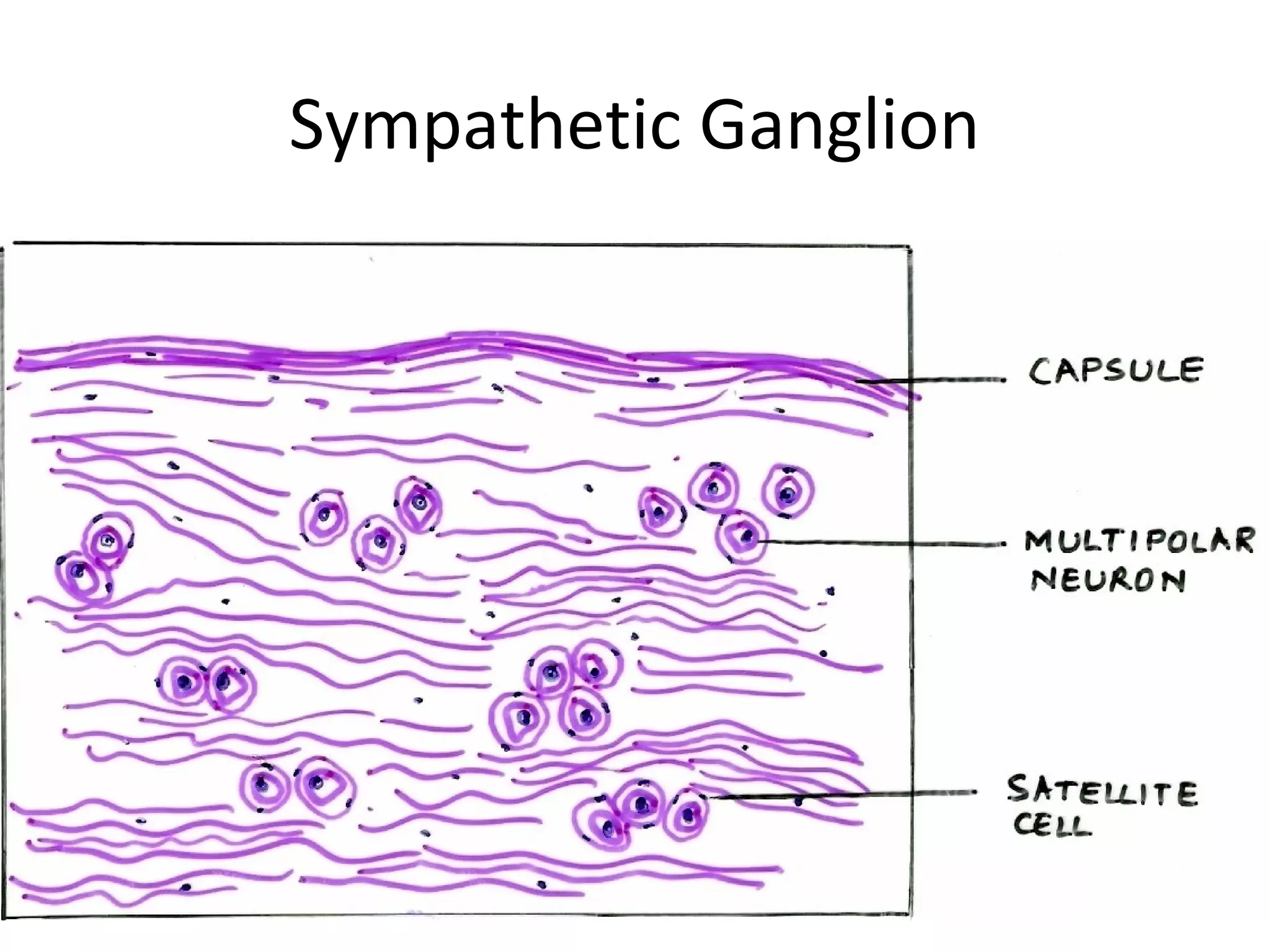
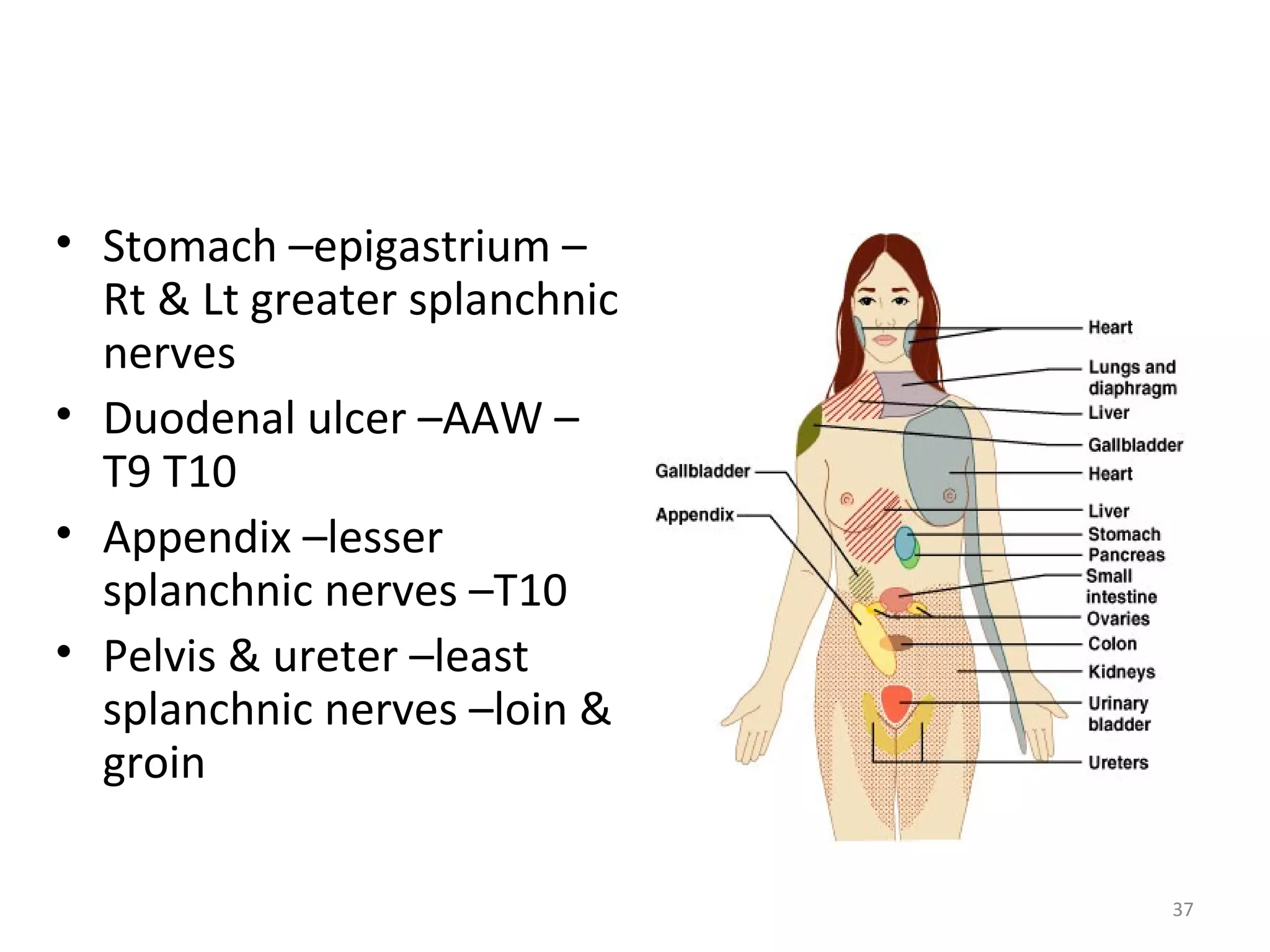
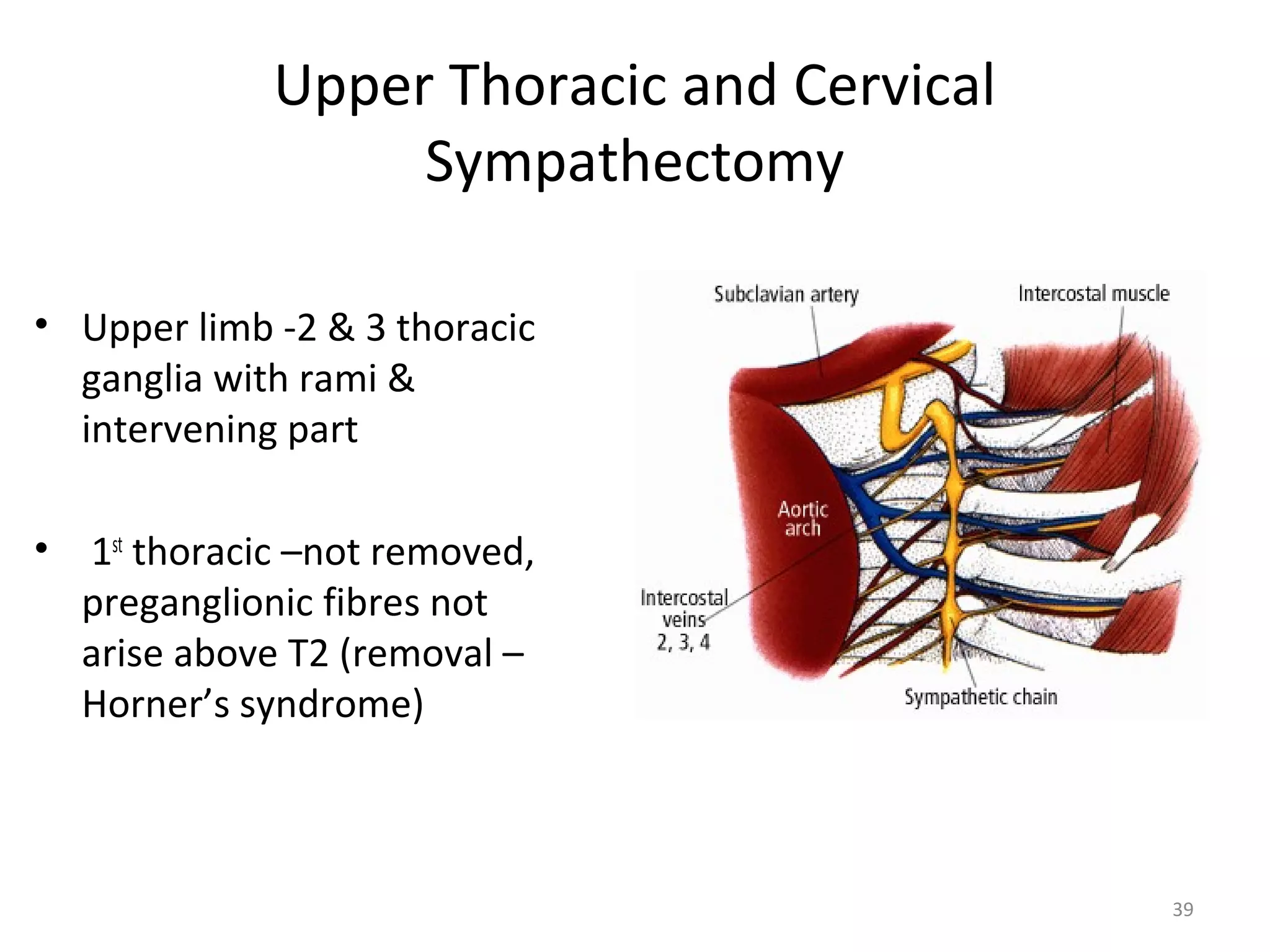
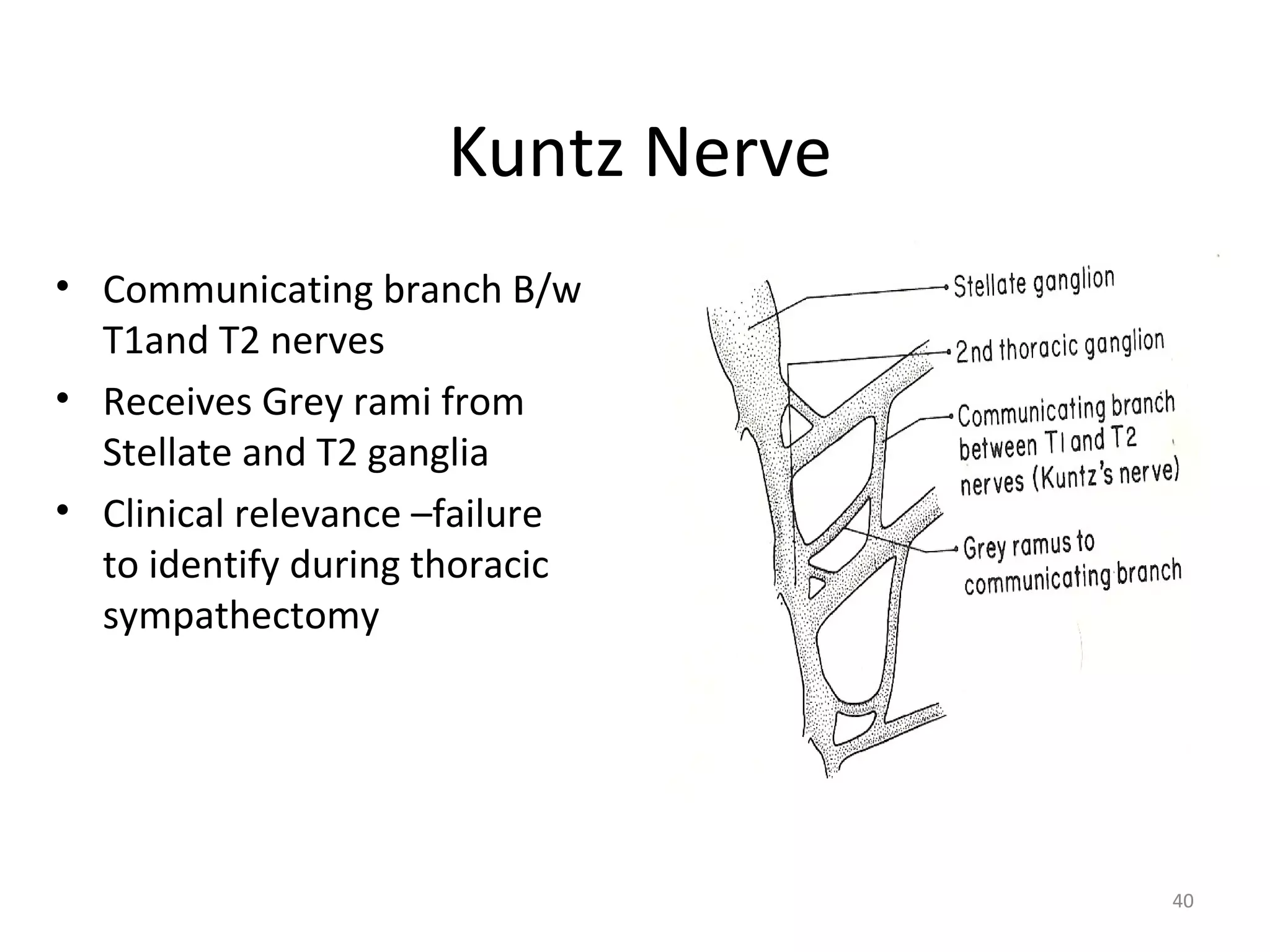
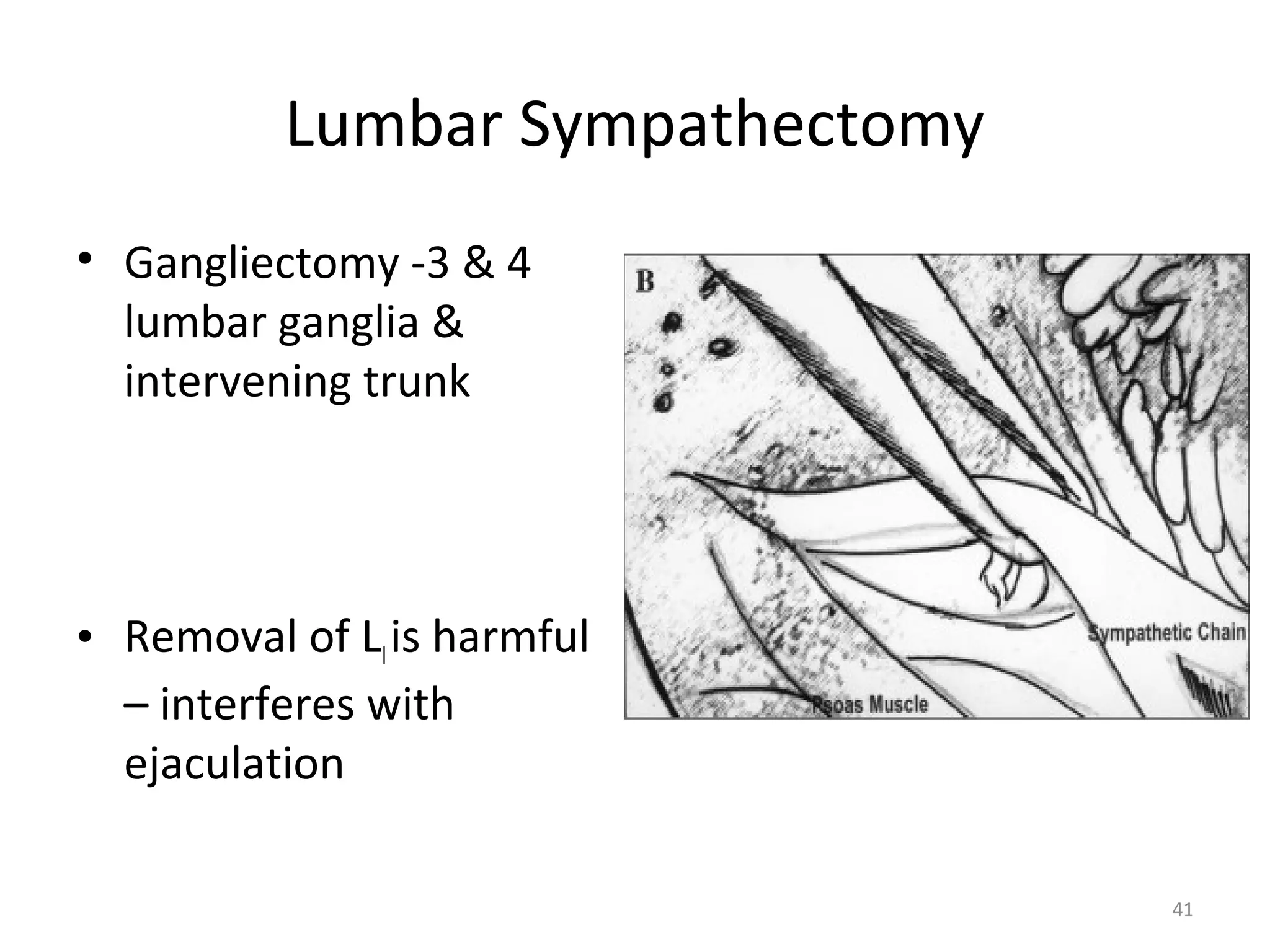
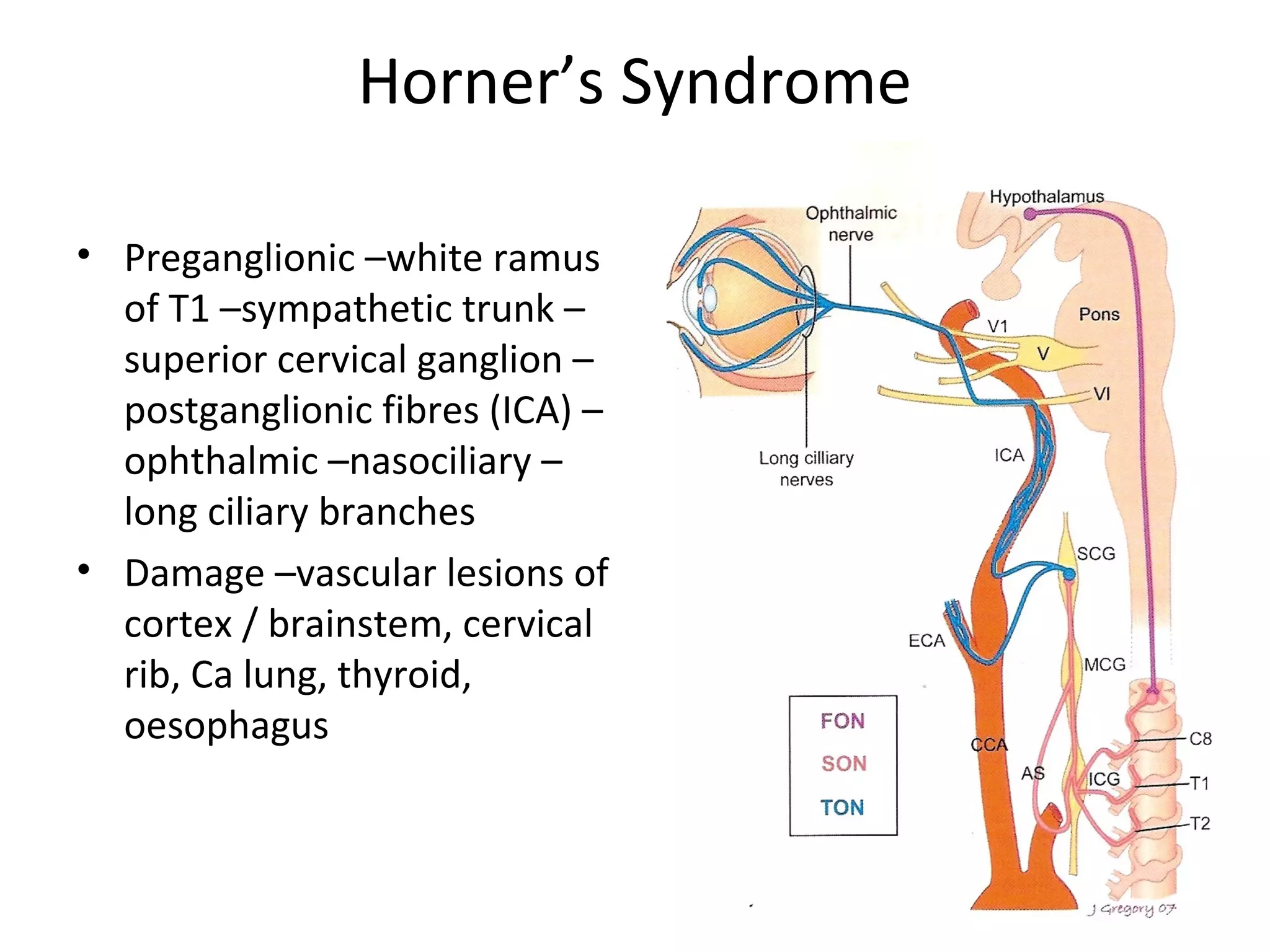
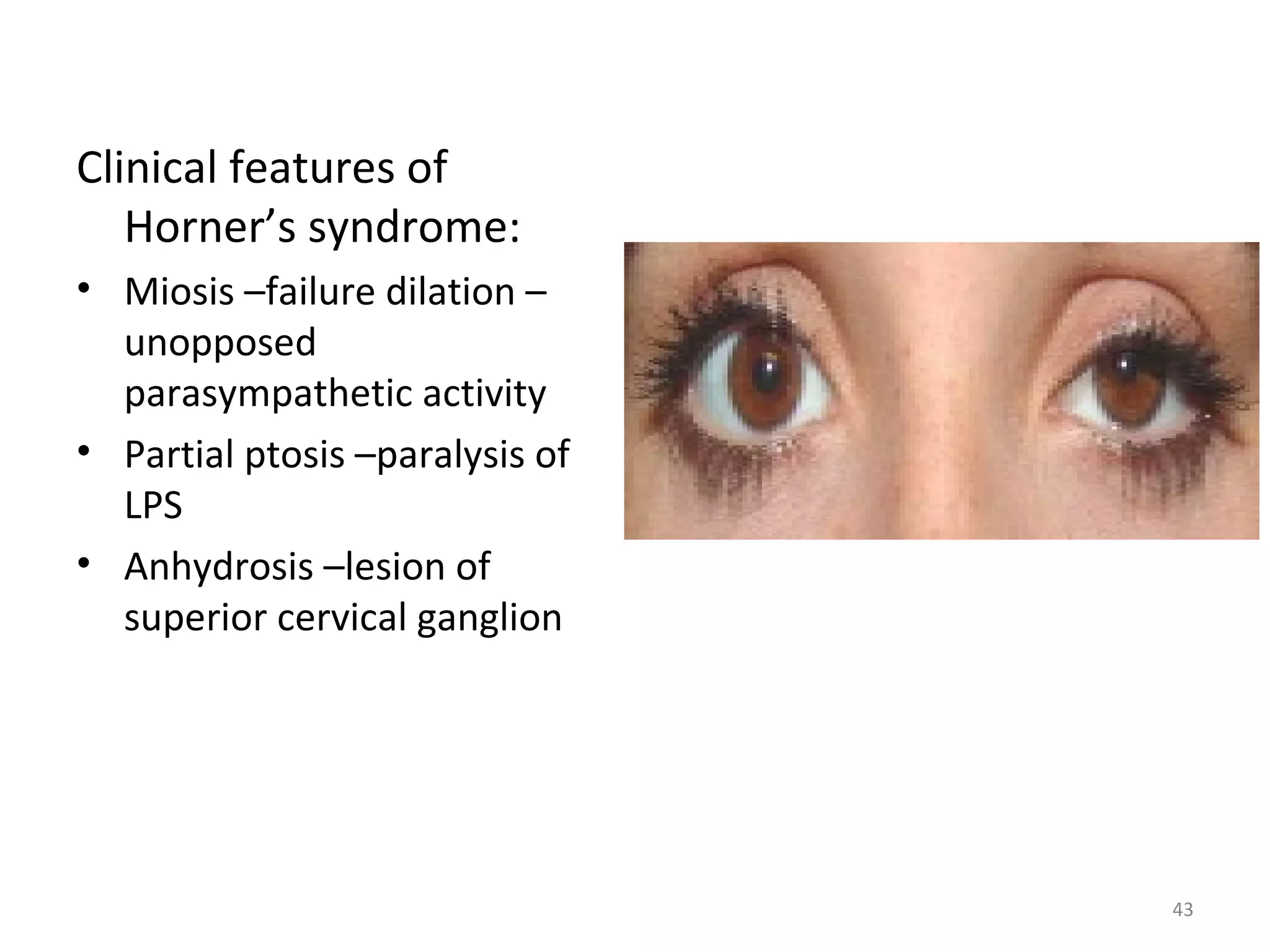
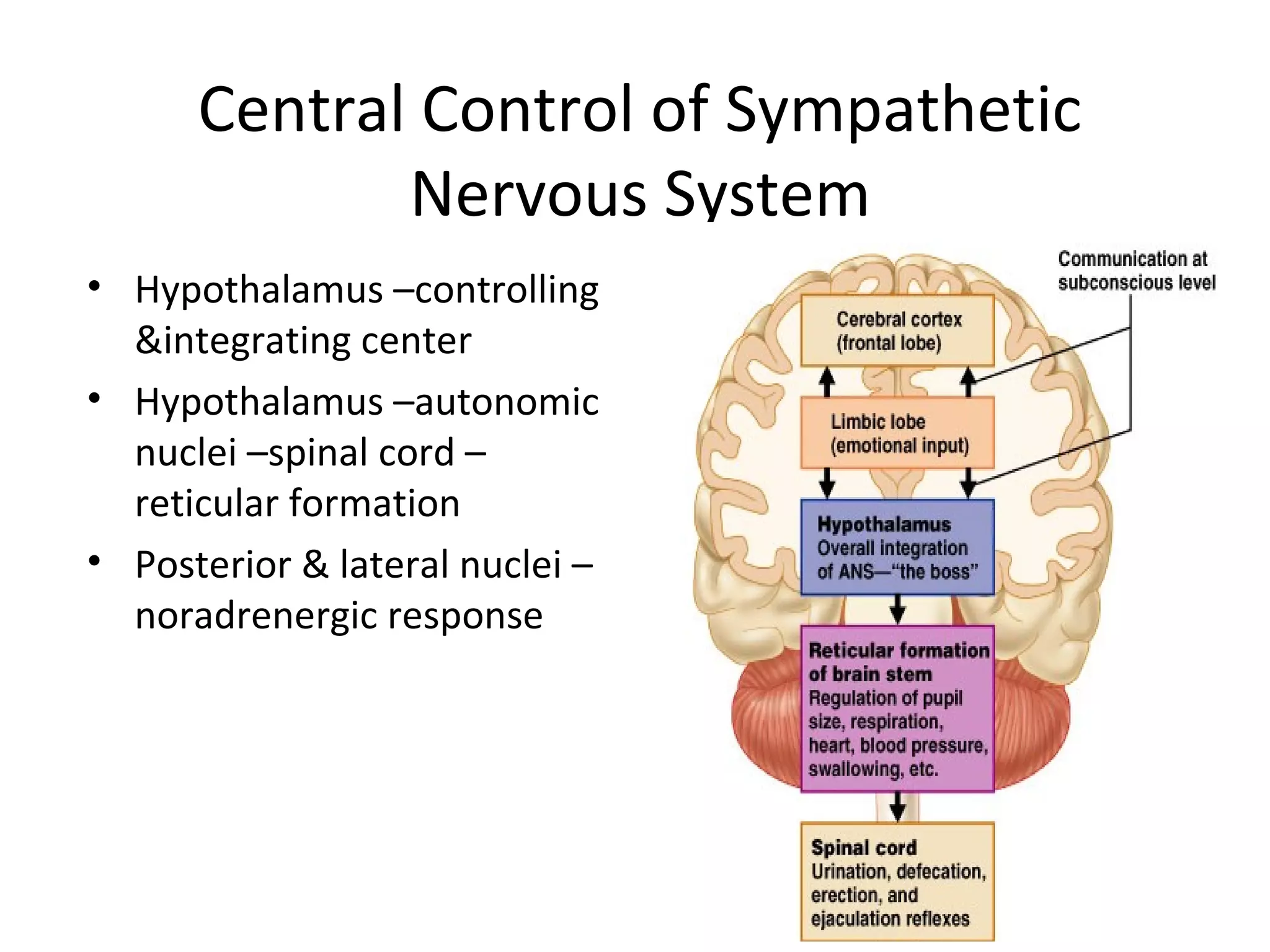
The autonomic nervous system consists of the sympathetic and parasympathetic nervous systems. The sympathetic nervous system is responsible for the fight or flight response and mobilizes the body during stress. It develops from neural crest cells that migrate along the spinal cord and form ganglia. Preganglionic neurons are located in the spinal cord and connect to postganglionic neurons in ganglia. The postganglionic neurons release norepinephrine to activate tissues. Surgical removal of sympathetic ganglia can help treat conditions like hyperhidrosis or peripheral vascular disease.