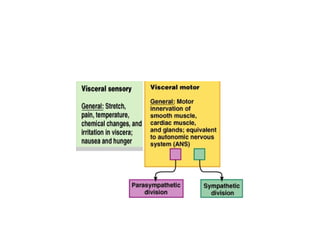
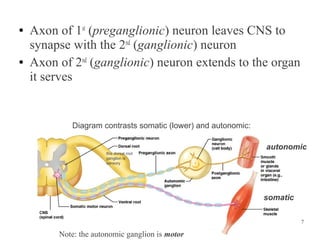
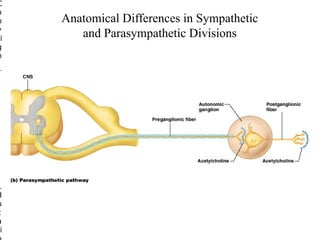
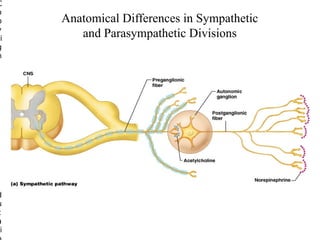
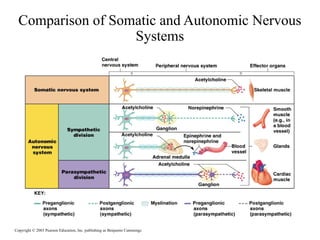
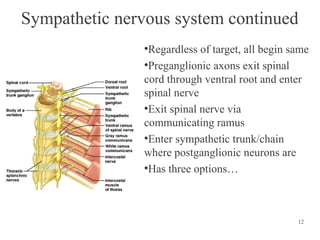
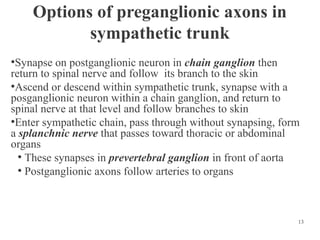
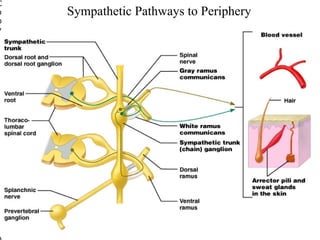
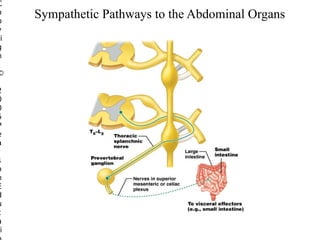
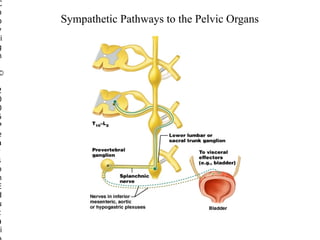
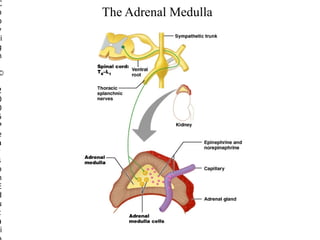
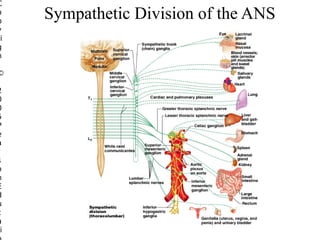
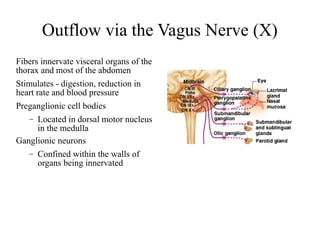
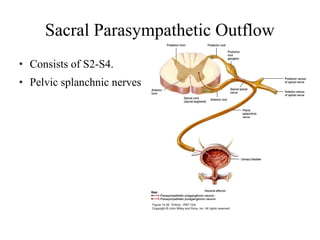
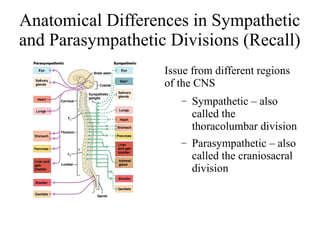
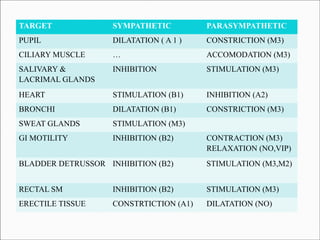
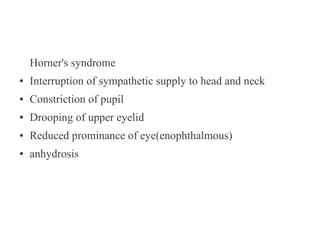
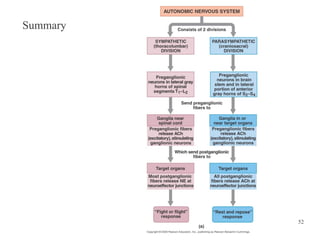
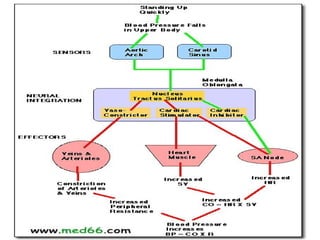
The autonomic nervous system regulates involuntary body functions and is divided into the sympathetic and parasympathetic nervous systems. It contains two neurons, with the preganglionic neuron cell body in the CNS and the postganglionic neuron cell body in autonomic ganglia. The sympathetic division is responsible for the fight or flight response and generally opposes the effects of the parasympathetic division, which is responsible for rest and digest functions. The enteric nervous system also helps control the gastrointestinal system independently.