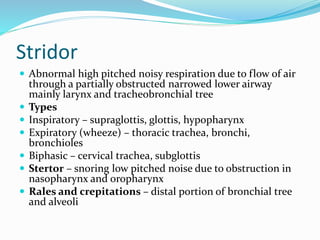
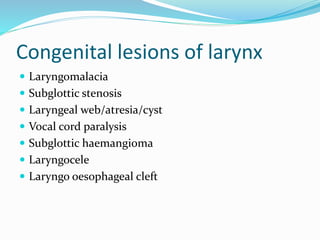
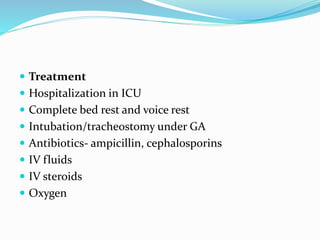
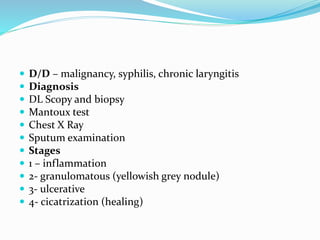
This document discusses various causes of stridor, which is an abnormal high pitched respiratory noise caused by partial airway obstruction. It covers different types of stridor and their etiologies in neonates, children and adults. Key causes discussed include laryngomalacia, vocal cord paralysis, croup, epiglottitis, diphtheria, tumors and foreign body obstruction. The document provides details on clinical assessment, investigations and management approaches for different stridor conditions.