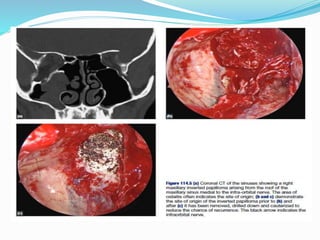
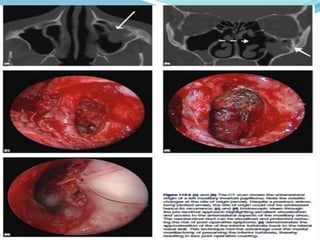
1. Inverted papilloma is a benign epithelial tumor originating from the Schneiderian membrane of the nasal cavity and paranasal sinuses.
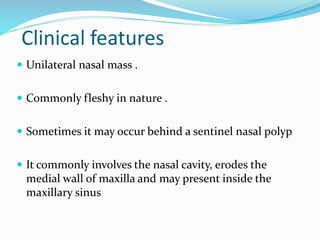
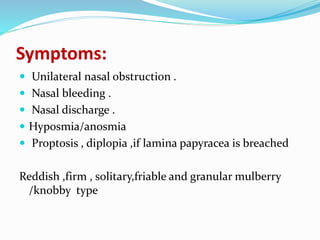
2. It most commonly affects males ages 30-50 and presents as a unilateral nasal mass, obstruction, and bleeding.
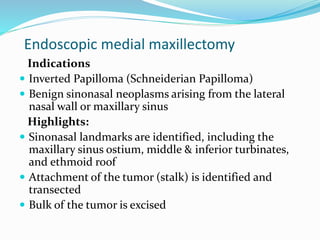
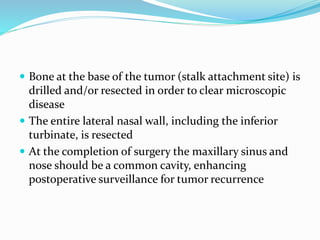
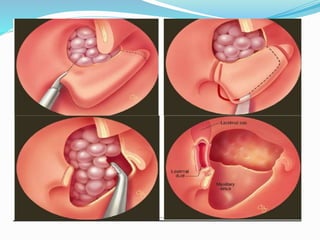
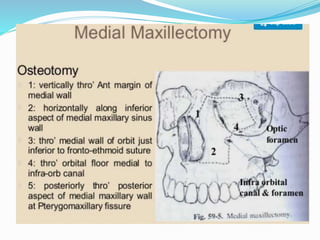
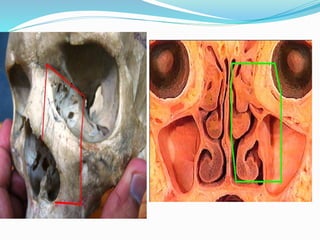
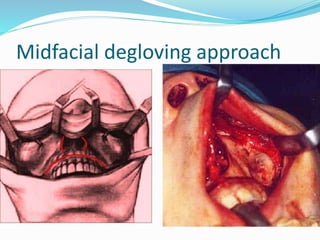
3. Treatment involves surgical resection, typically an endoscopic medial maxillectomy to remove the entire lateral nasal wall and clear the tumor attachment site.