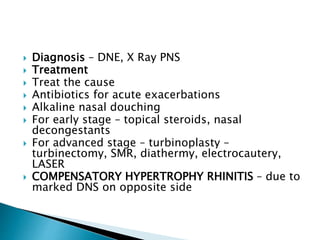
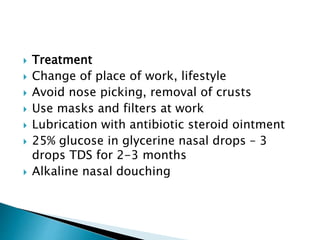
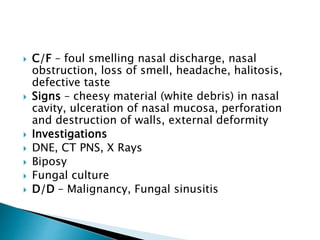
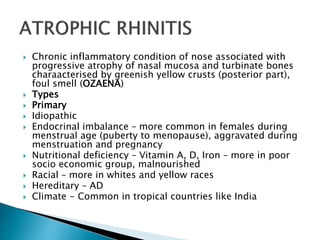
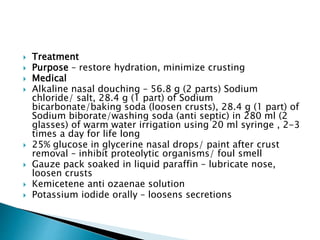
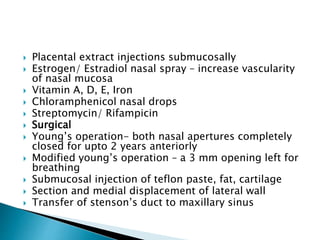
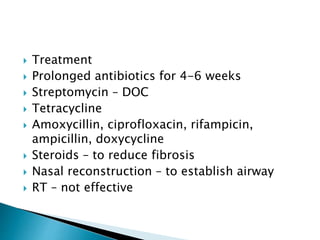
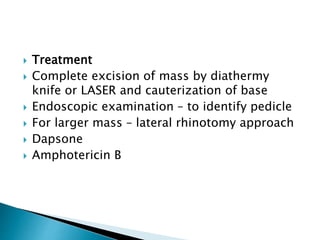
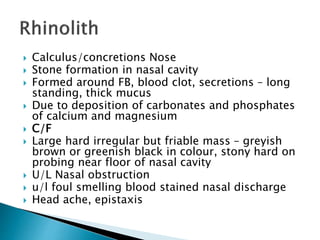
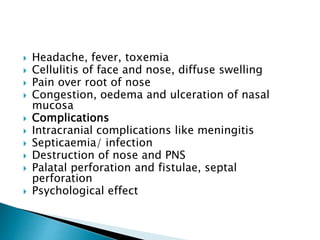
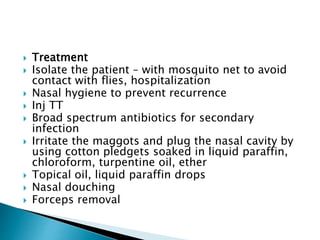
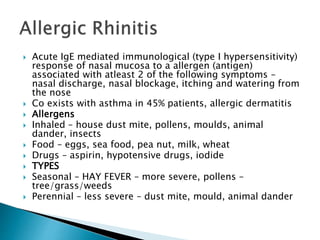
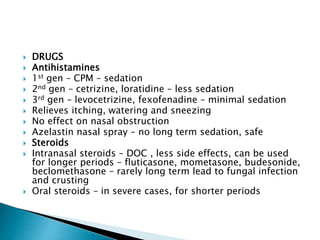
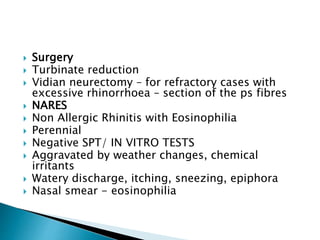
The document describes various types of rhinitis including infective causes like the common cold from viruses like rhinovirus and influenza. It also discusses chronic rhinitis, which can be simple or hypertrophic. Non-infective causes like allergic rhinitis are mentioned. Specific conditions involving the nasal mucosa are outlined such as atrophic rhinitis, ozaena, rhinoscleroma, and nasal cholesteatoma. Causes, symptoms, examinations, and treatments are provided for each condition in the summary.