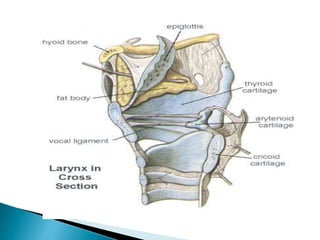
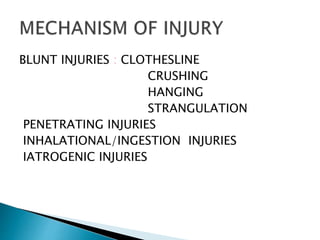
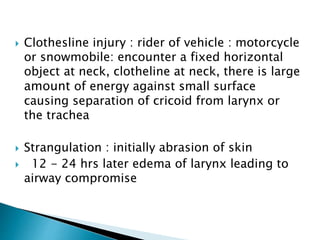
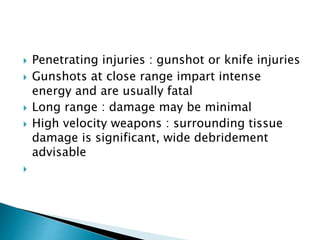
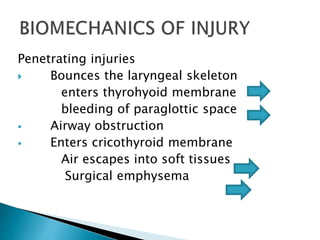
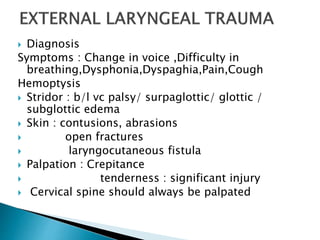
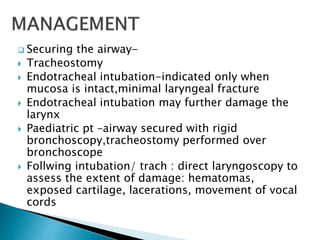
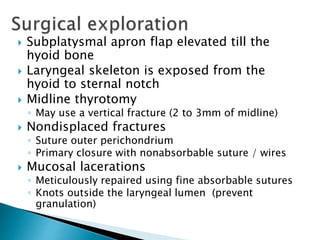
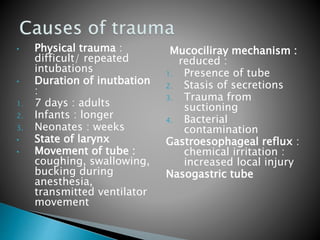
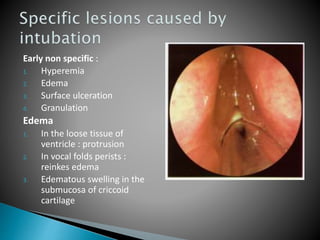
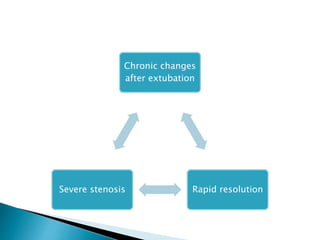
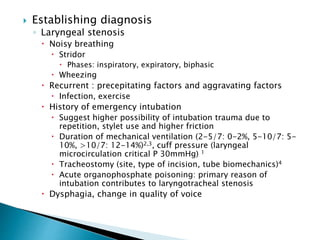
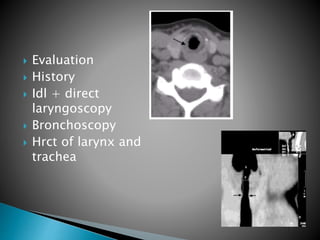
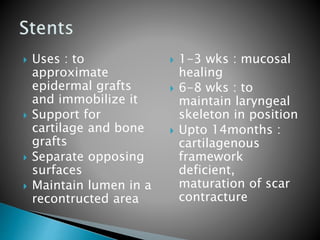
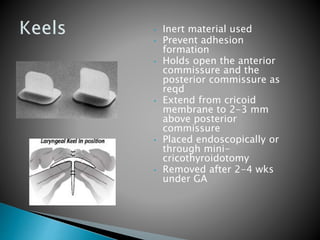
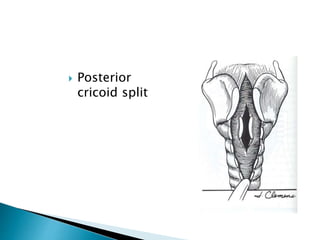
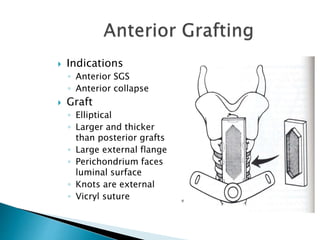
This document discusses laryngeal trauma. The larynx functions to protect the airway and enable phonation. Laryngeal trauma is rare, usually resulting from motor vehicle accidents, strangulation, or penetrating injuries. Injuries can range from minor bruising to fractures or separation of the laryngeal framework. Treatment involves securing the airway, usually through intubation or tracheostomy. Minor injuries are managed conservatively while more severe injuries involving exposed cartilage or vocal fold immobility require surgical exploration and repair. Endolaryngeal stents may be used in very severe cases to support the laryngeal structure during healing.