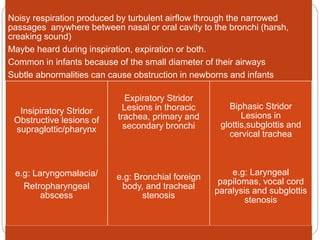
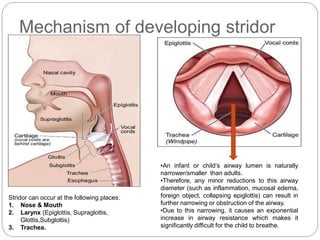
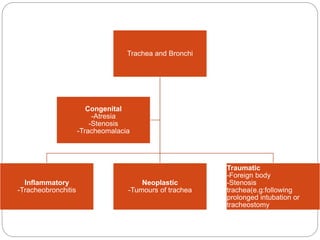
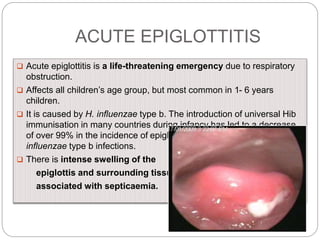
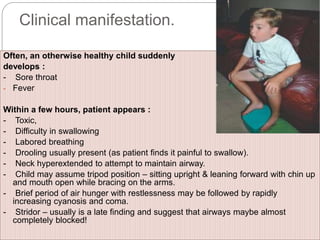
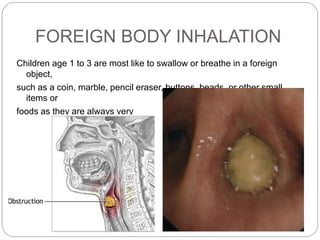
Stridor is a harsh sound produced by turbulent airflow through a narrowed airway. It can occur from the nose to the bronchi. Common causes in infants include laryngomalacia, vocal cord paralysis, and subglottic stenosis. Acute causes of stridor include croup, epiglottitis, foreign body inhalation, and retropharyngeal abscess. A thorough clinical exam and diagnostic imaging can help identify the specific site and cause of airway obstruction producing the stridor. Timely diagnosis and treatment are important to prevent respiratory distress.