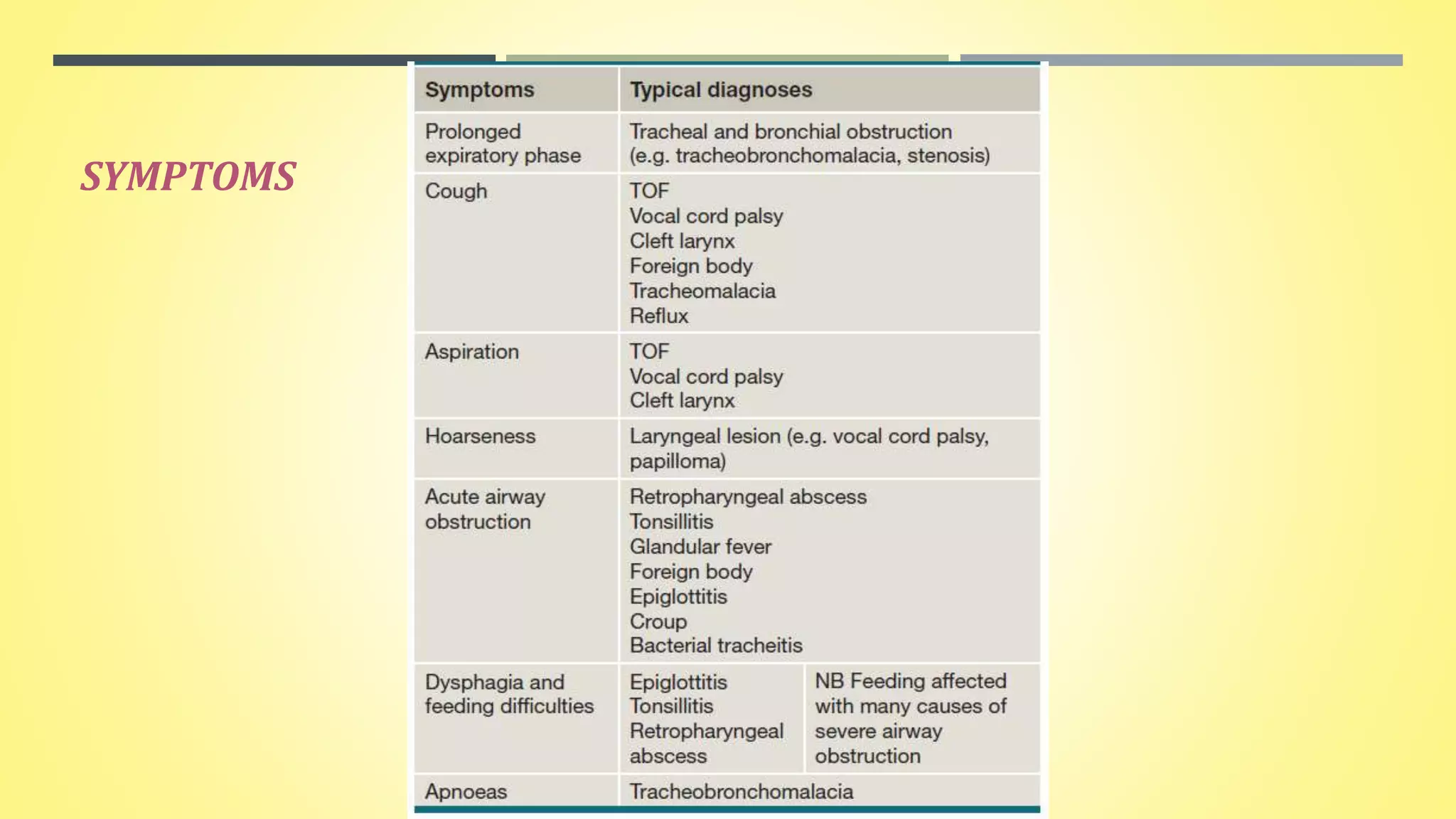
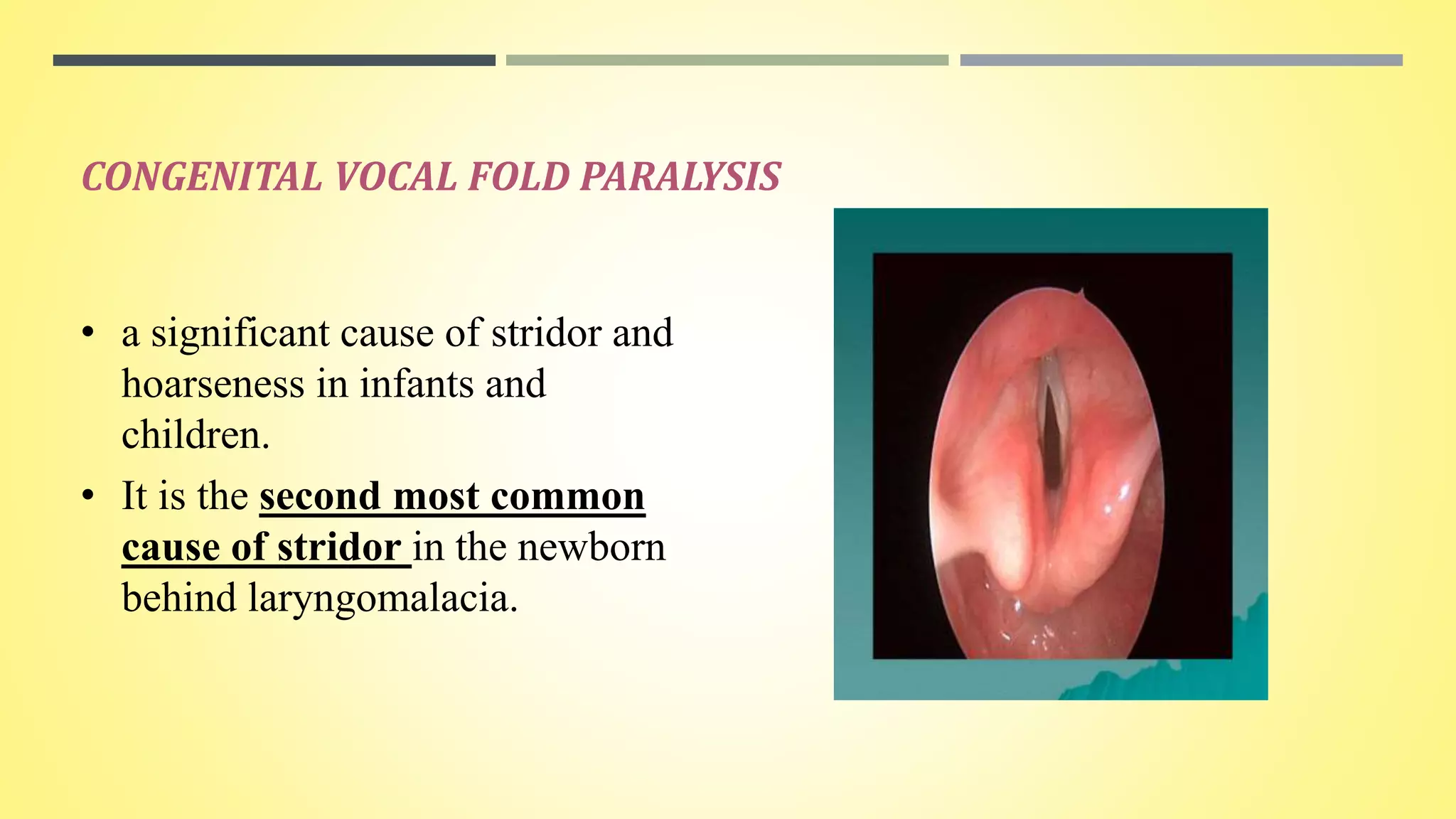
Pediatric stridor can have various causes related to the anatomy and development of the infant airway. The document discusses several congenital lesions that can cause stridor, including laryngomalacia, the most common cause. It involves the partial or complete collapse of the supraglottic structures during inspiration. Other discussed lesions are laryngeal cysts, bifid epiglottis, laryngeal webs, and congenital vocal fold paralysis. Flexible laryngoscopy is important for diagnosis and management may involve observation, procedures like supraglottoplasty, or tracheostomy for severe cases.