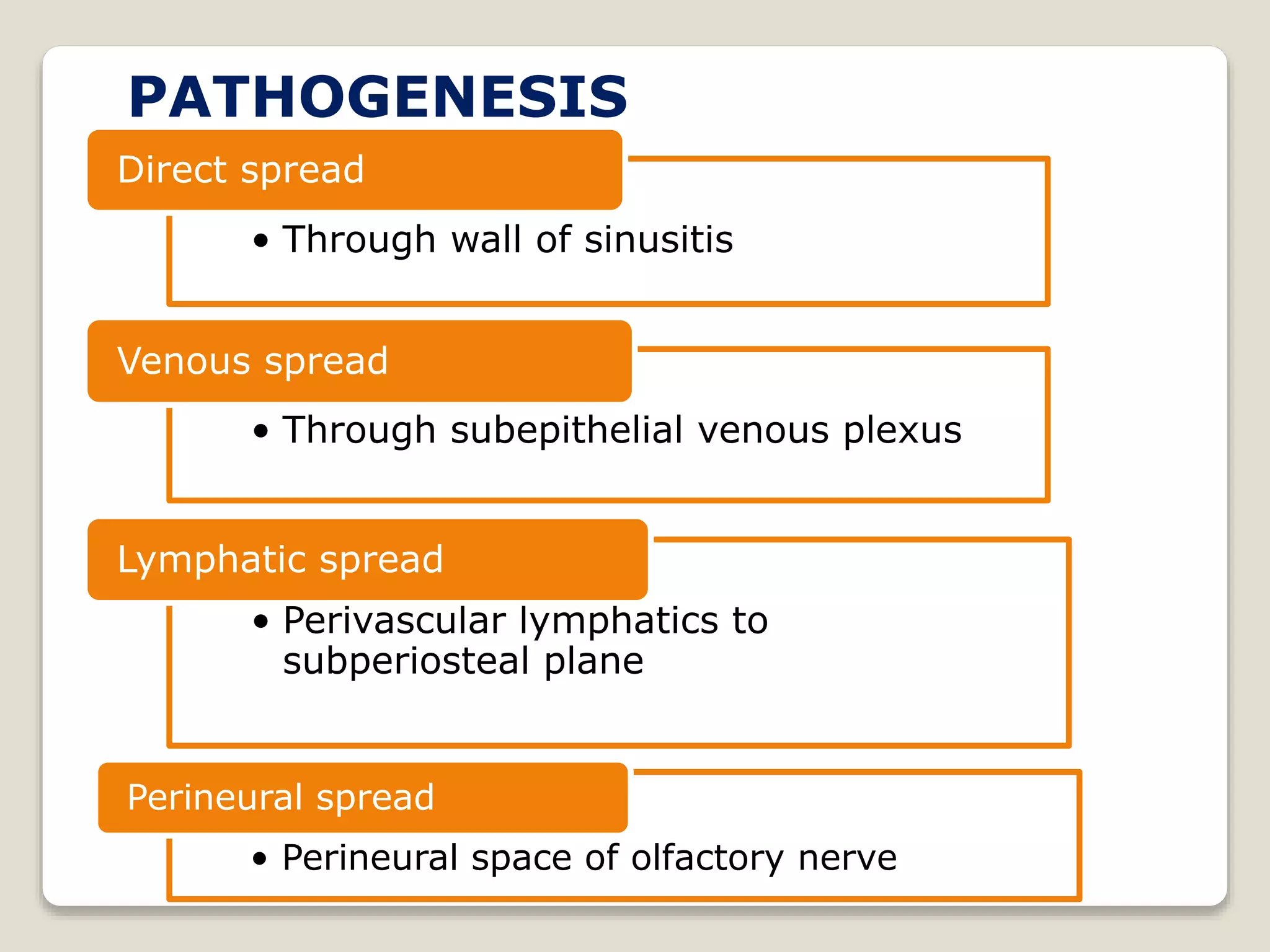
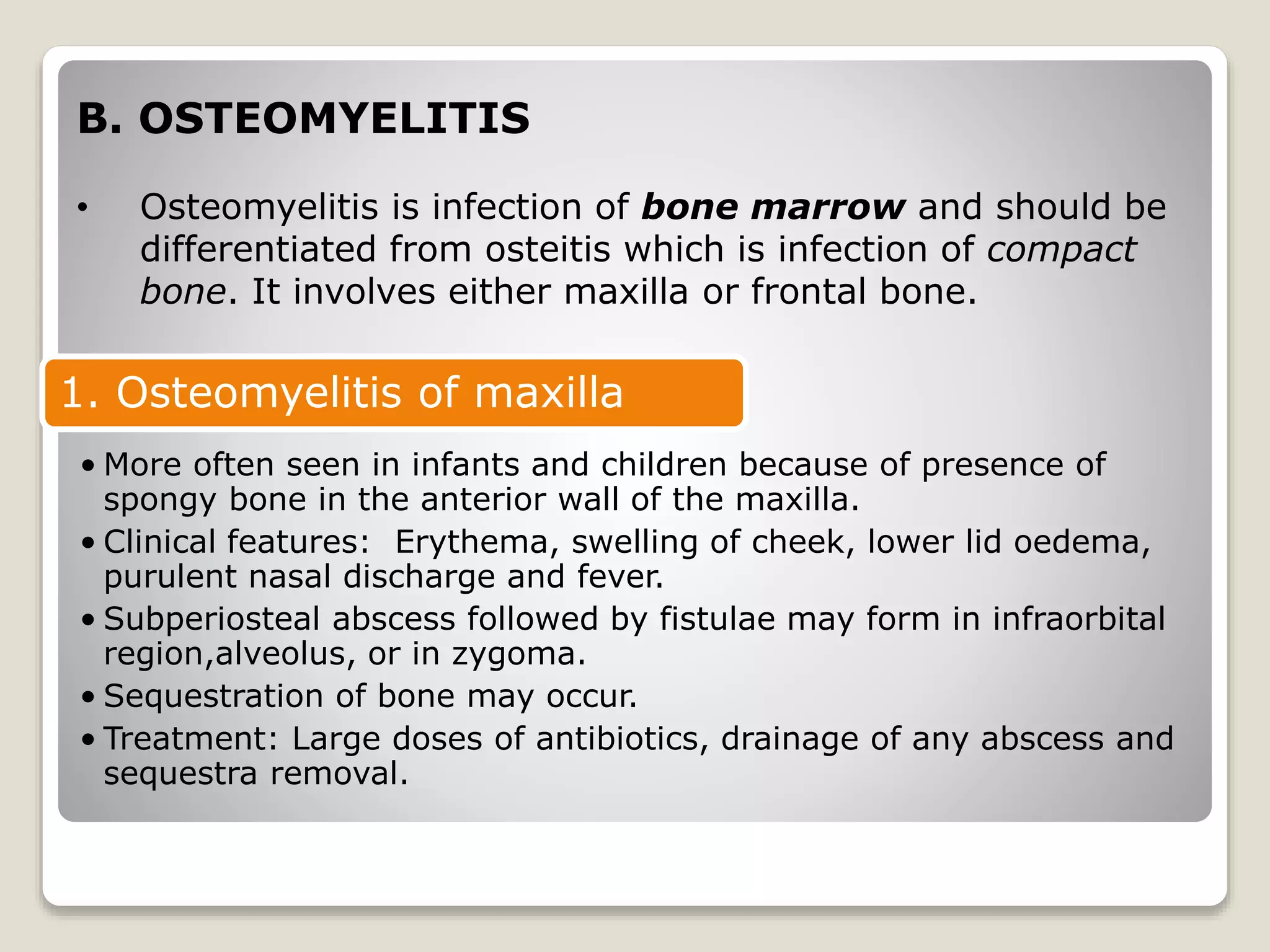
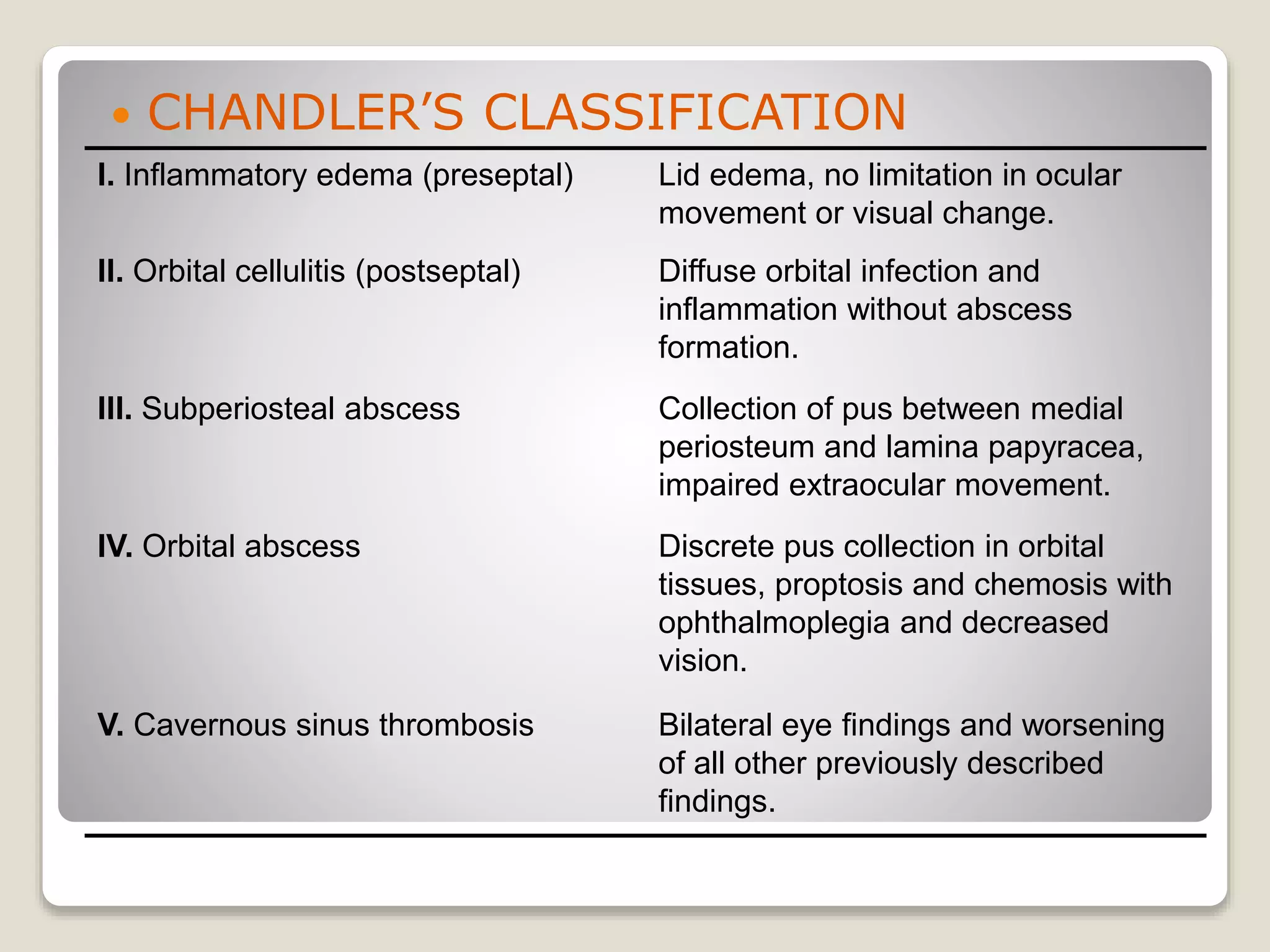
1) Sinusitis complications arise when infection spreads beyond the sinus mucosa into surrounding areas like the orbit or skull. Common local complications include mucoceles/pyocles, osteomyelitis of the frontal bone or maxilla, and orbital issues like preseptal cellulitis, subperiosteal abscesses, or orbital cellulitis.
2) Intracranial complications from sinusitis spreading can cause meningitis, extradural or subdural abscesses, brain abscesses, or cavernous sinus thrombosis. Descending infections from sinus discharge can also lead to otitis media, pharyngitis, or laryngitis.
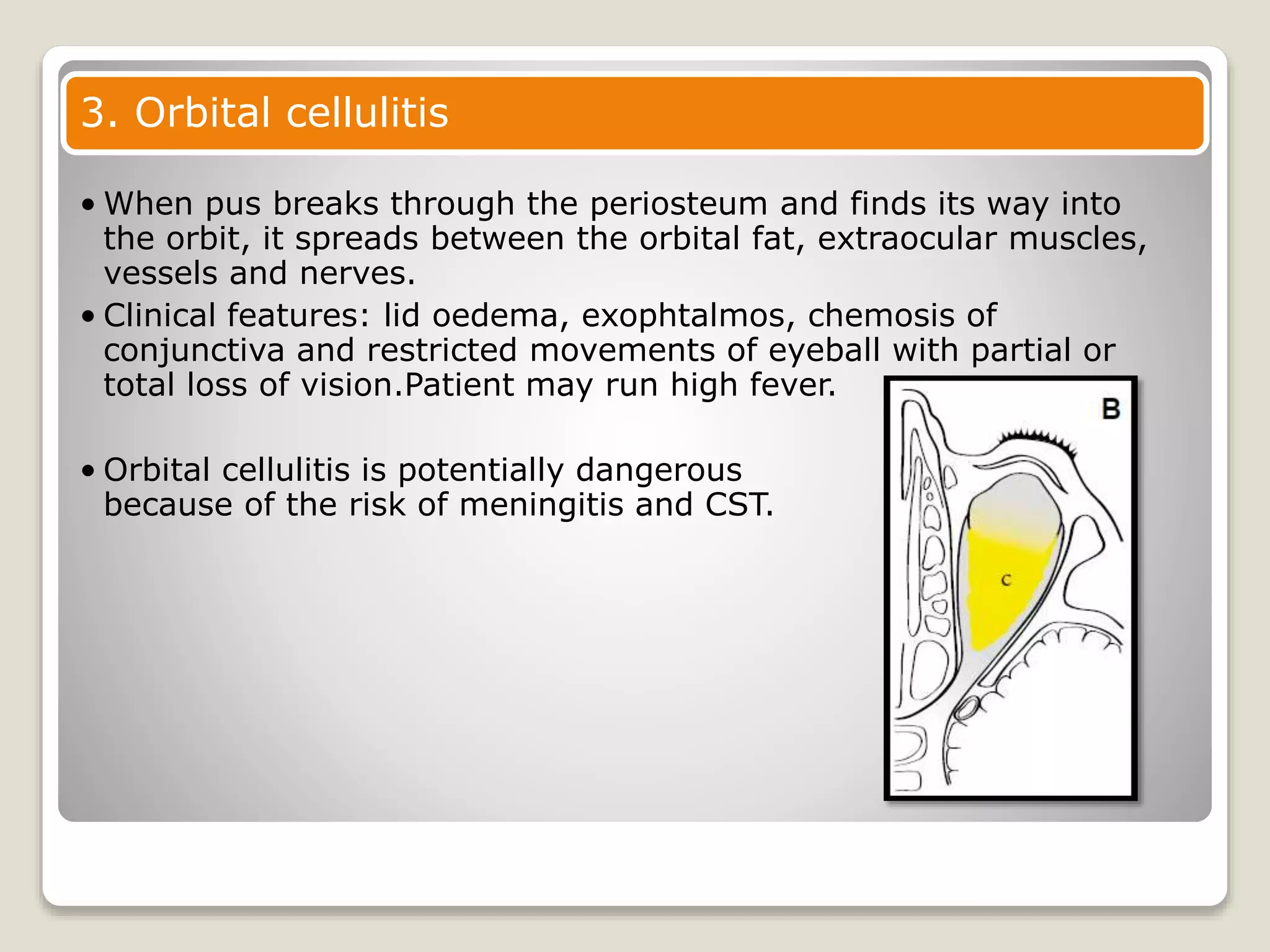
3) Orbital cell