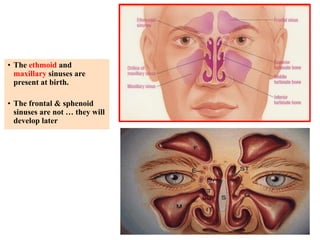
Rhinosinusitis is inflammation of the nasal passages and sinuses. The paranasal sinuses are air spaces surrounding the nasal cavity. Common causes include viral or bacterial infection leading to blocked sinus drainage and inflammation. Symptoms include facial pain, pressure, congestion, and mucus discharge. Treatment involves antibiotics, nasal steroids, surgery to improve drainage if symptoms persist long-term. Chronic rhinosinusitis lasts over 12 weeks and may require repeated treatments.