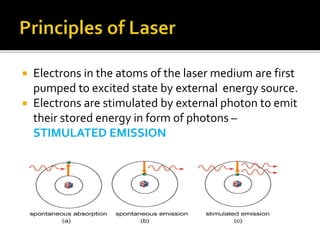
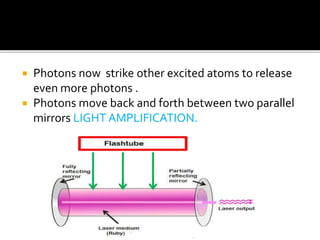
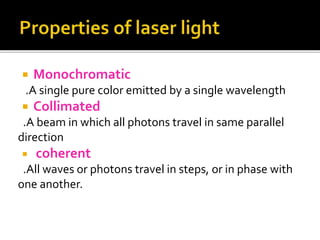
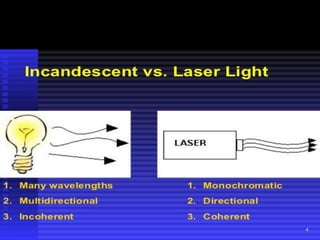
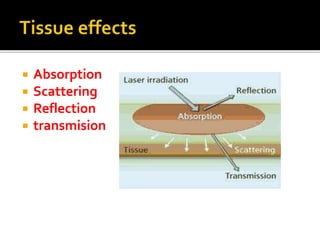
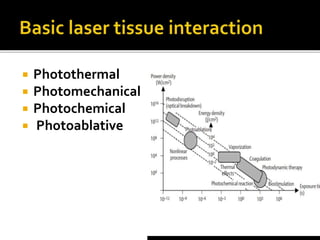
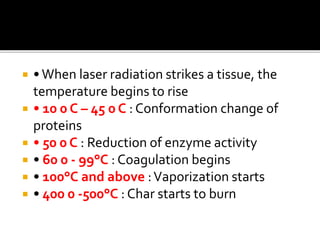
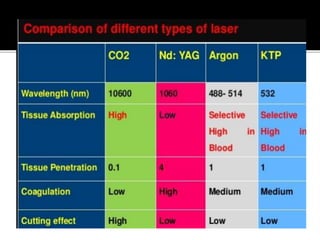
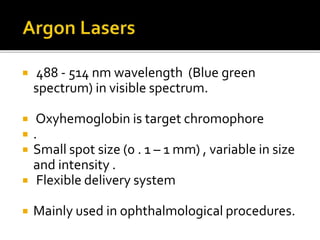
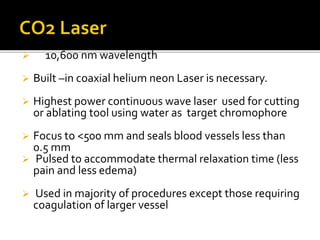
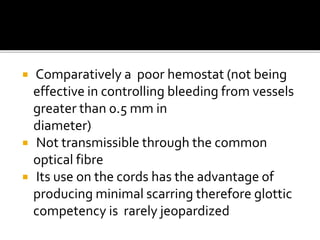
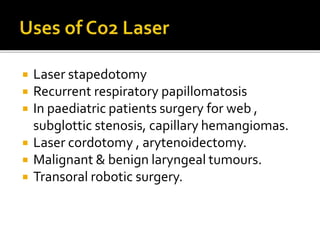
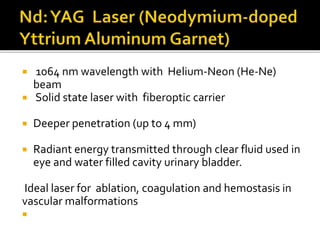
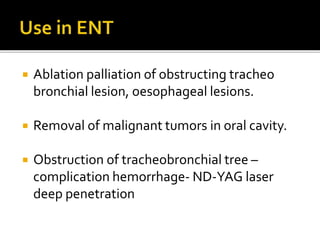
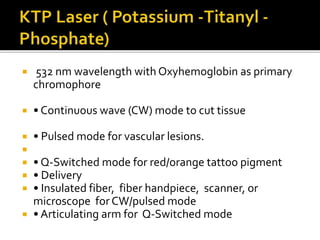
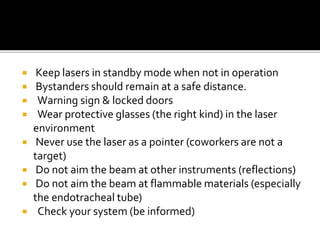
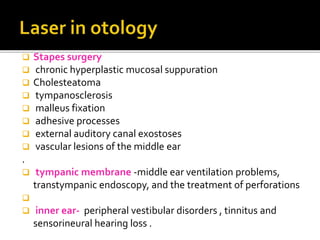
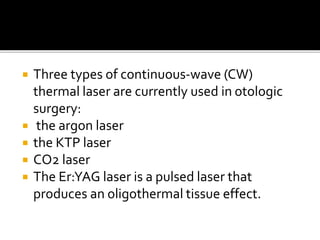
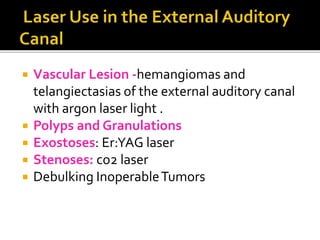
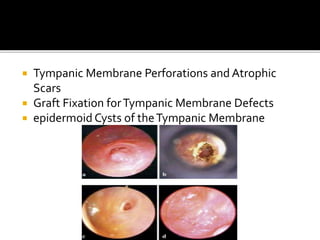
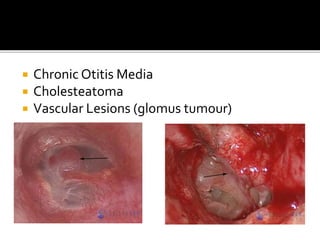
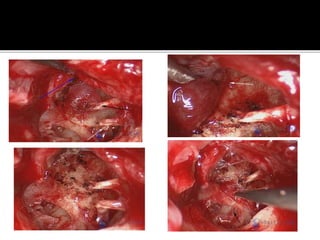
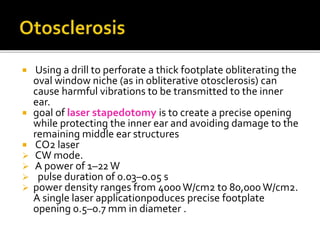
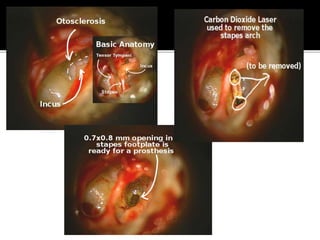
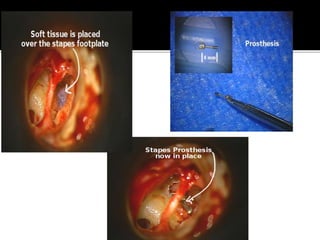
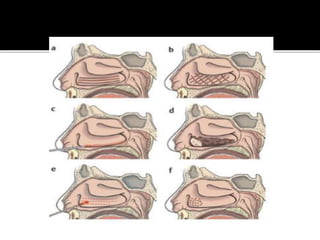
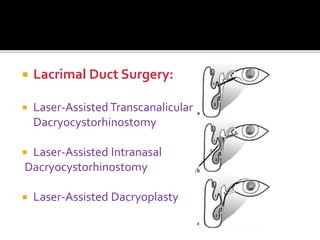
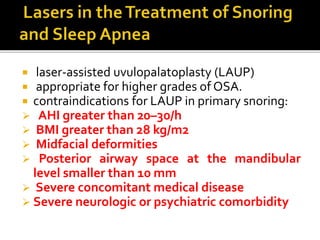
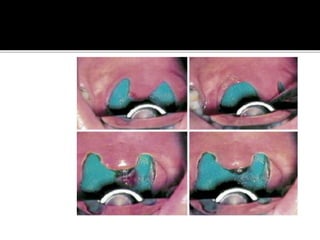
The document discusses lasers used in otolaryngology. It begins by explaining the basic principles of how lasers work, such as stimulated emission and amplification of photons. It then discusses different types of lasers used including CO2, KTP, Nd:YAG, and diode lasers. Applications are described for procedures like stapedotomy, turbinate reduction, and tumors. Safety considerations and the parameters used for different procedures are also outlined.