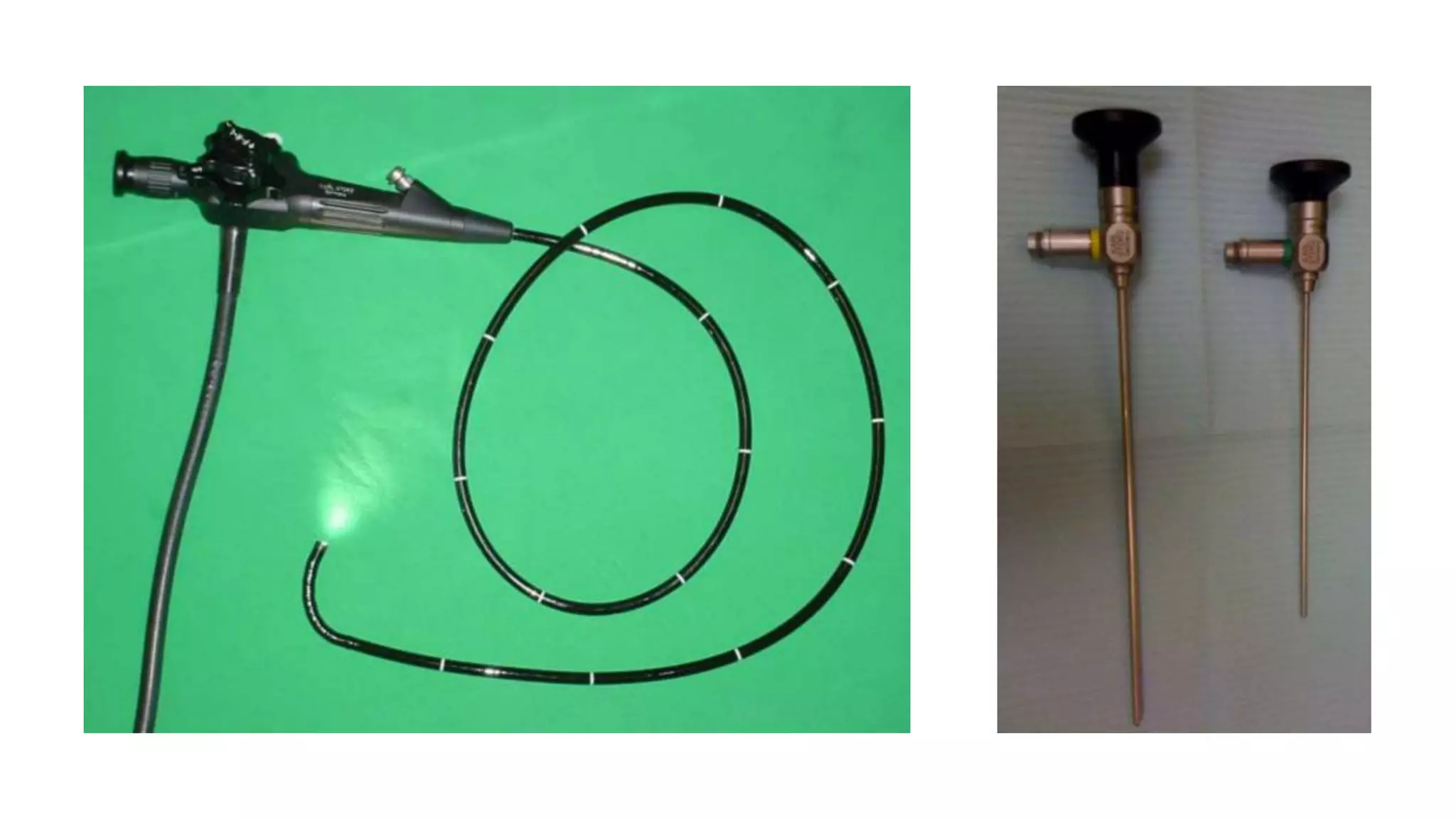
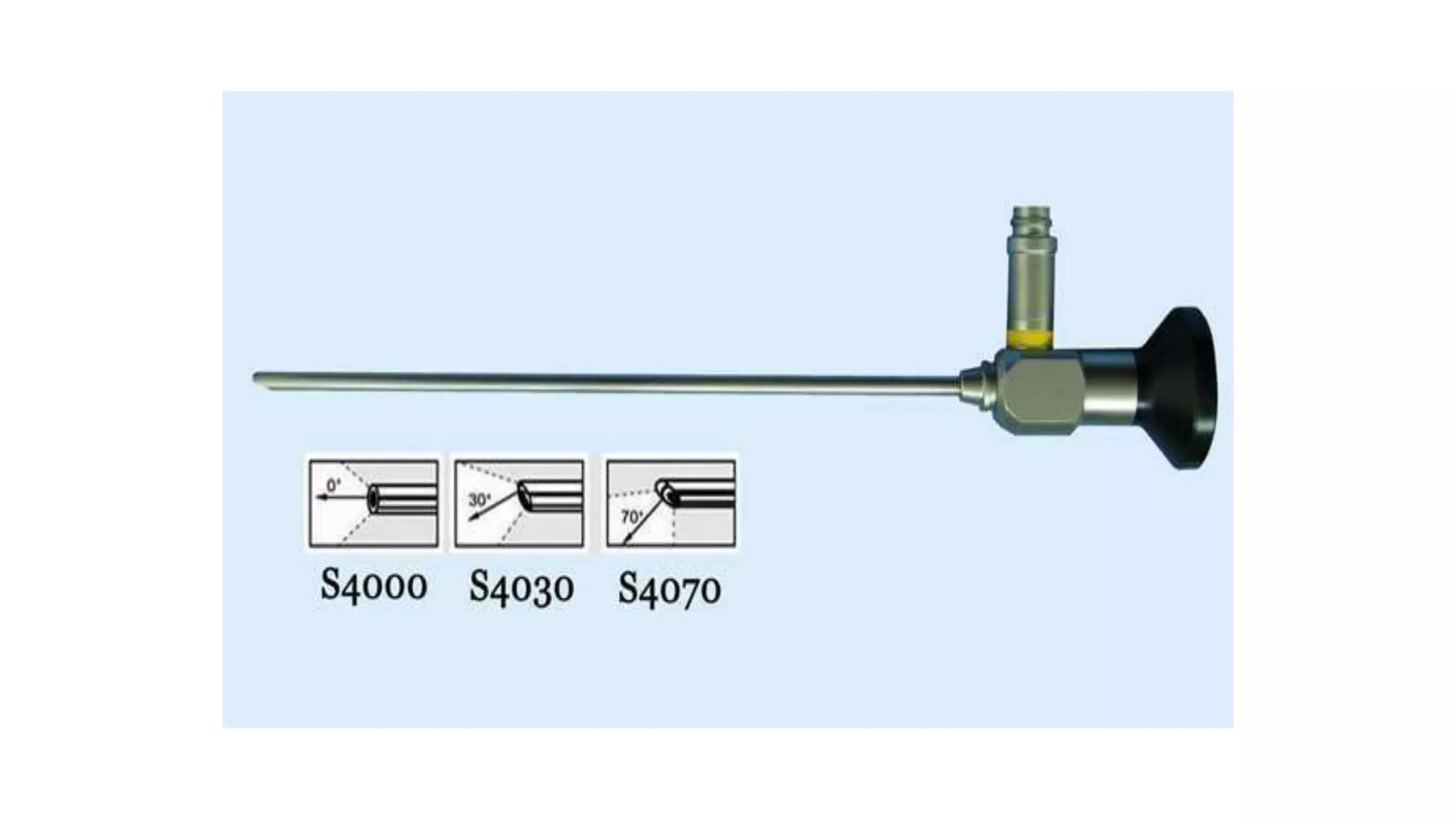
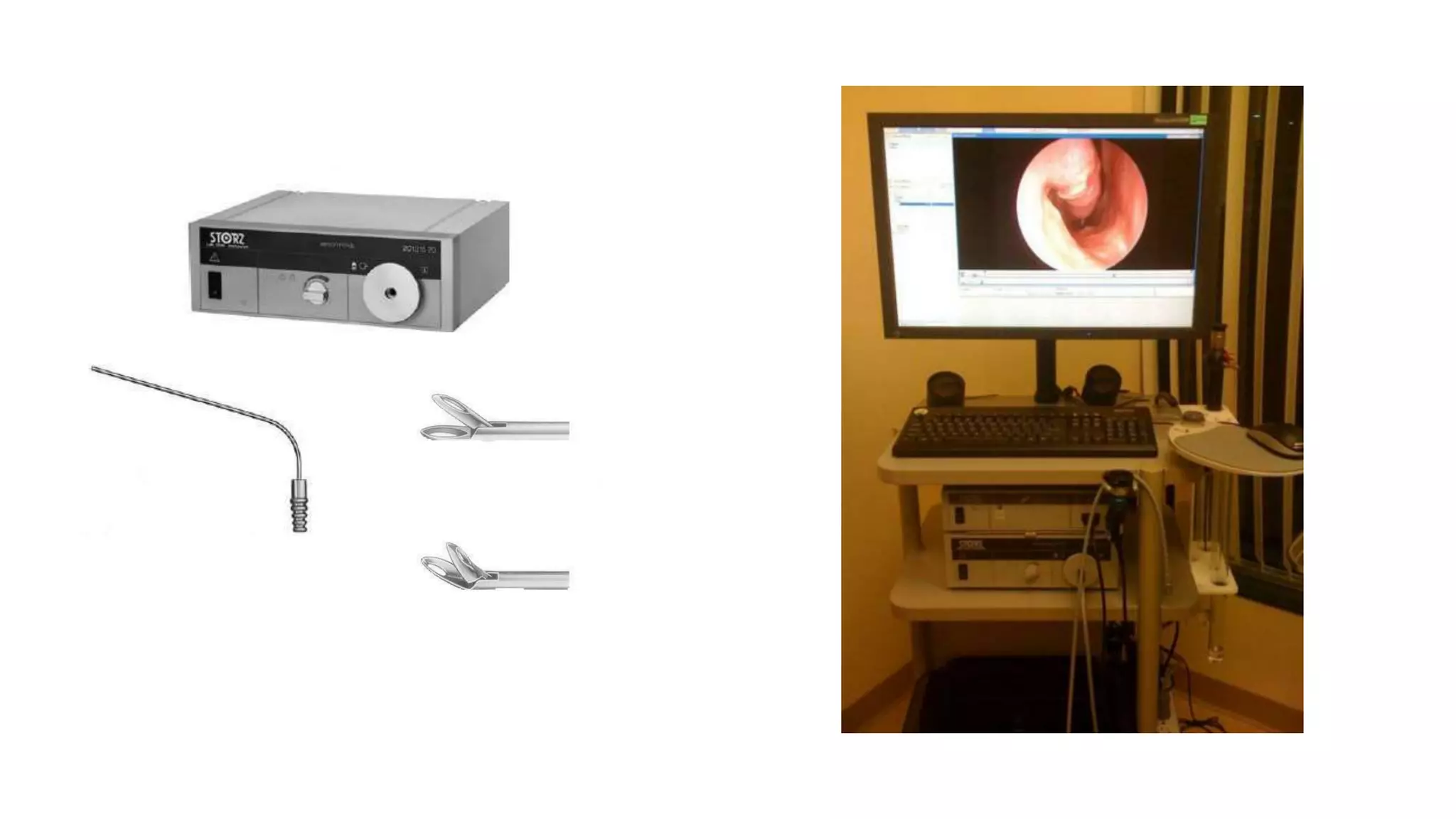
This document provides an overview of diagnostic nasal endoscopy. It discusses that nasal endoscopy allows direct visualization of the nasal and sinus passages using an endoscope. It can be performed with flexible or rigid endoscopes. The document outlines the indications, contraindications, technical considerations, equipment, patient preparation, technique, and potential complications of nasal endoscopy. Nasal endoscopy is a commonly used diagnostic tool by otolaryngologists to evaluate nasal pathology.