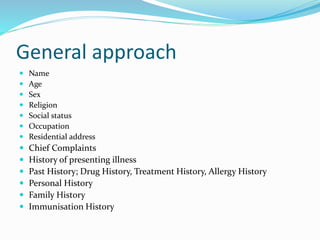
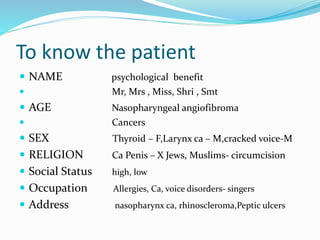
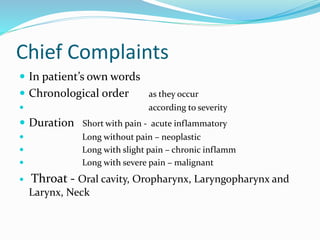
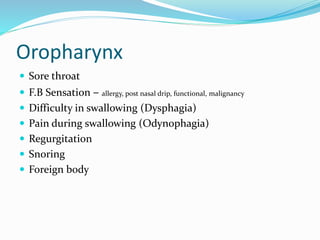
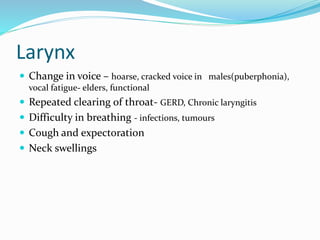
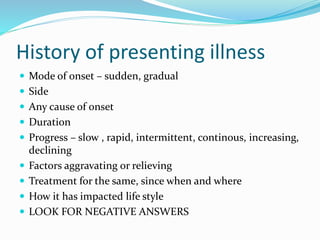
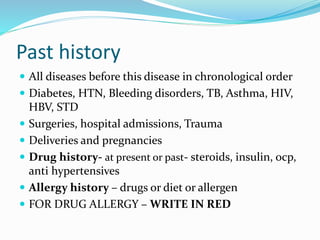
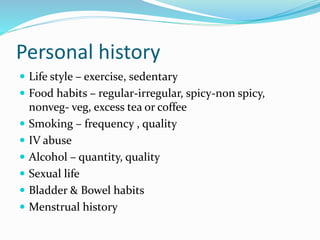
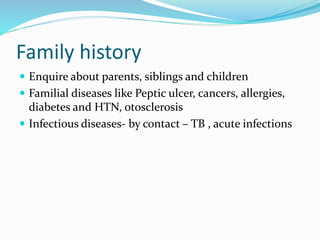
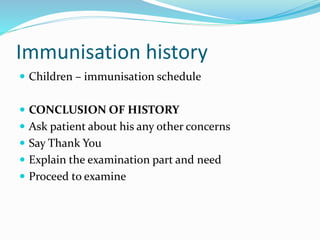
This document provides guidance on taking a thorough history from an ENT patient. It outlines the key components of the history to cover, including: patient identifying information like name, age, sex; chief complaints; history of present illness; past medical, surgical, drug and allergy histories; personal and family histories; and immunization history. It describes the importance of listening to the patient, using their language, making them comfortable and remembering they are assessing you too. Sections provide more detail on questions for specific anatomical areas like the oral cavity, oropharynx and larynx. The goal is to fully understand the patient and their condition.