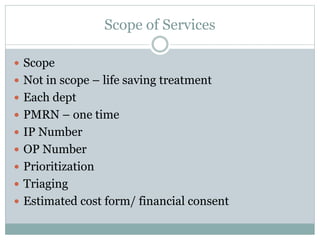
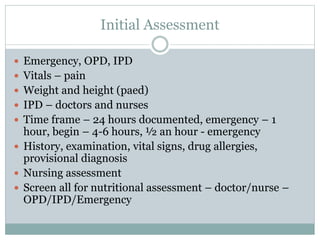
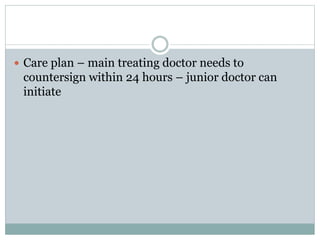
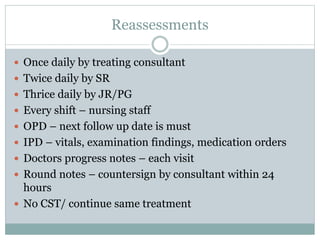
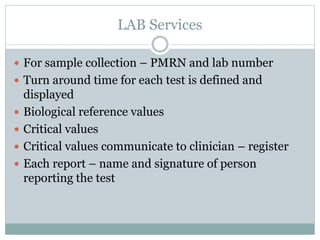
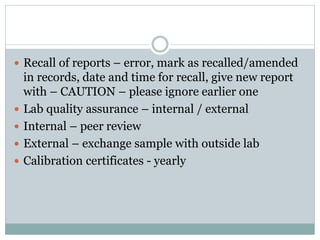
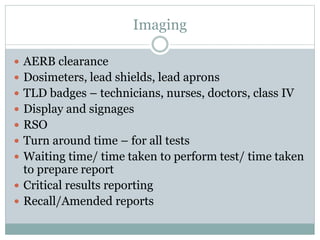
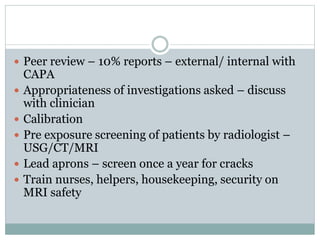
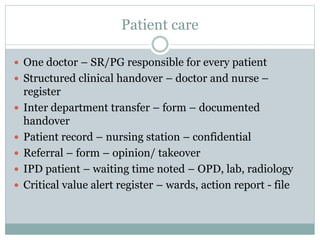
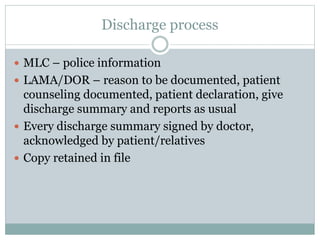
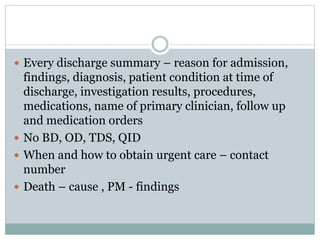
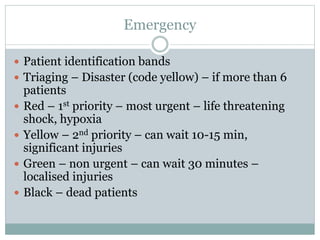
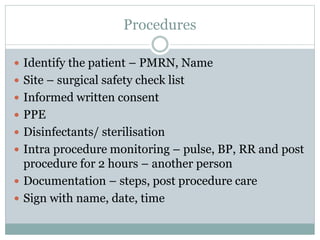
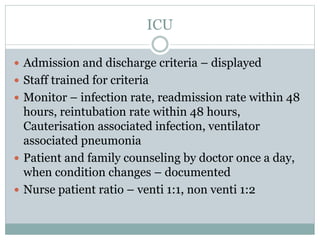
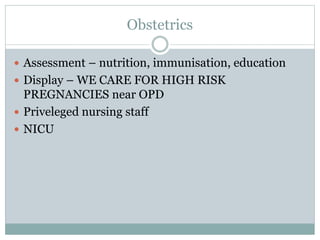
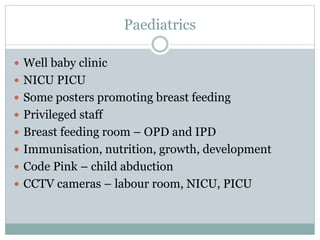
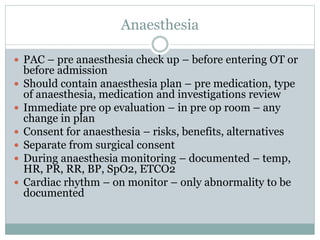
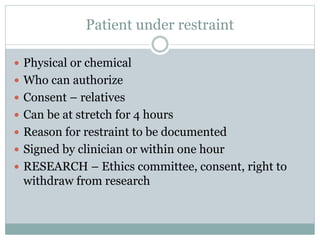
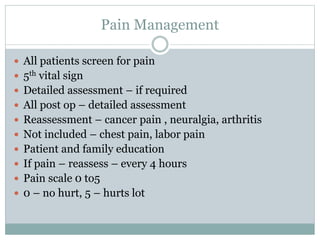
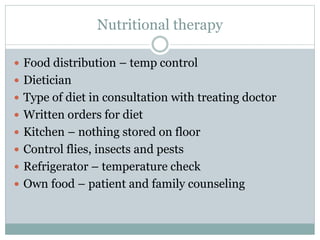
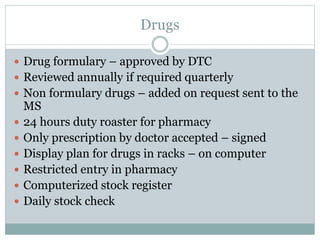
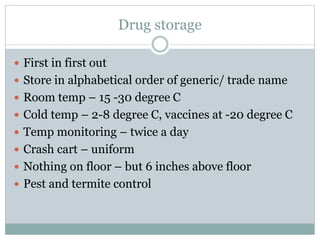
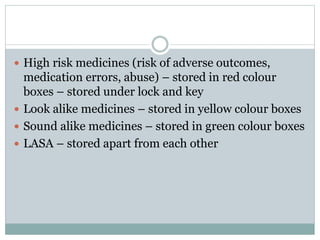
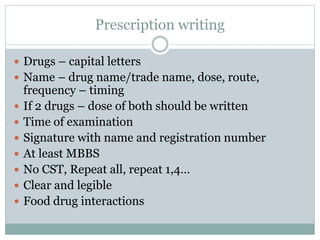
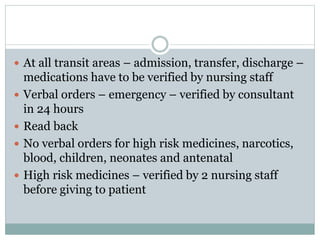
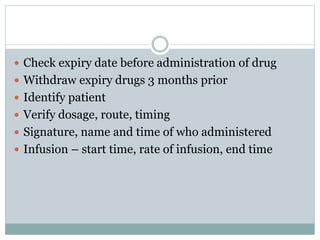
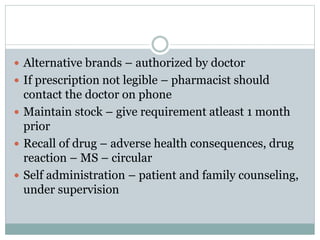
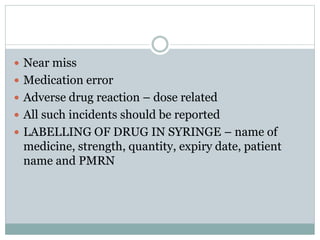
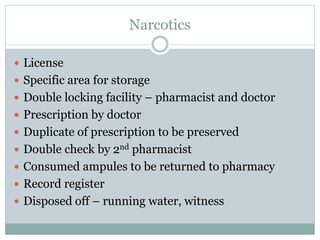
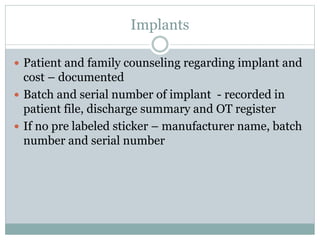
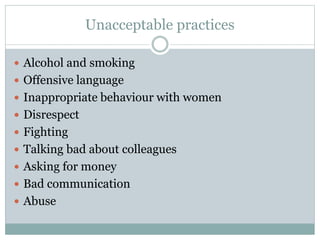
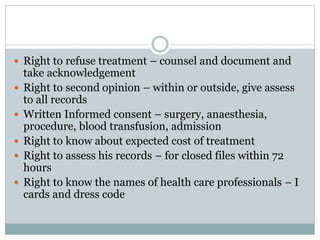
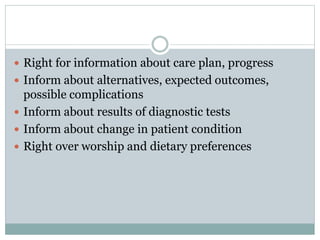
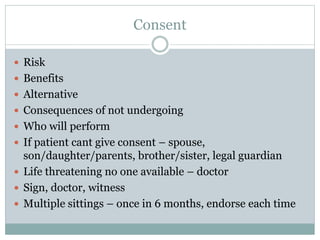
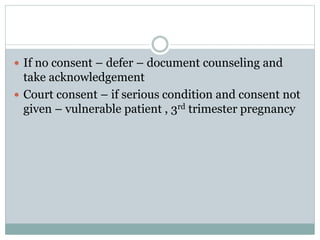
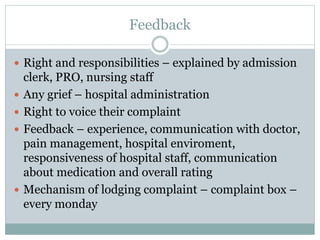
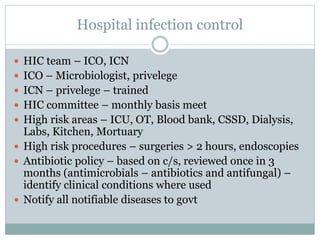
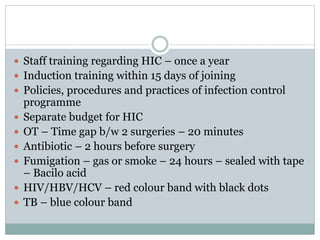
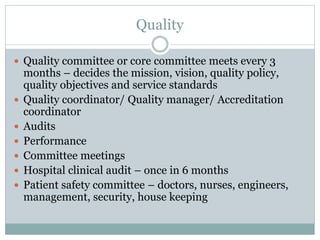
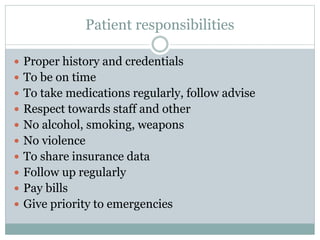
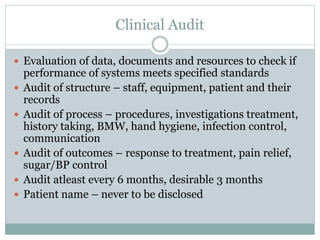
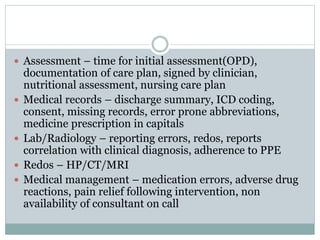
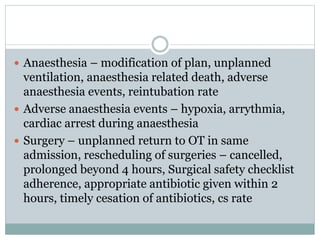
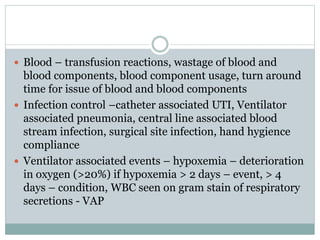
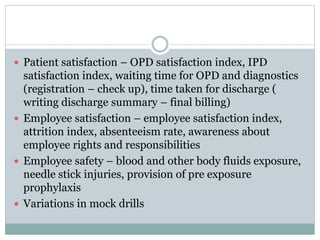
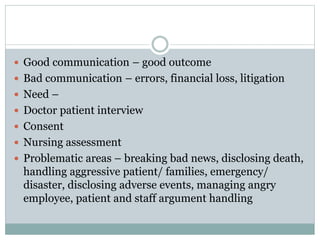
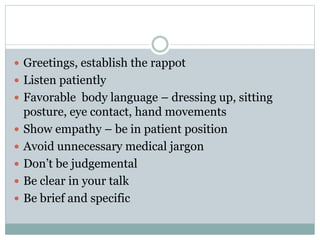
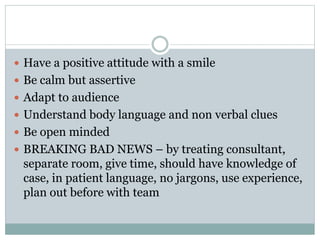
This document outlines policies and procedures for various departments and services within a hospital including emergency, imaging, laboratory, pharmacy, nursing, and patient rights. It describes requirements for initial patient assessments, monitoring and documentation, informed consent, infection control, quality assurance, and other standards. The key aspects covered are initial patient triaging and assessments, documentation of vital signs, examinations, test results and care plans, informed consent for procedures, proper prescribing and administration of medications, and protection of patient privacy, dignity and rights.