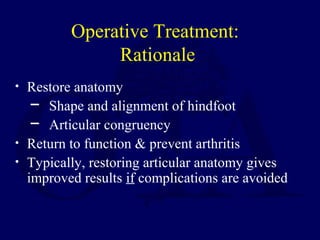
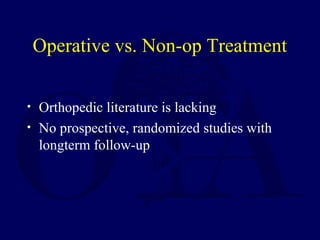
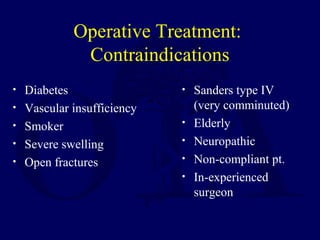
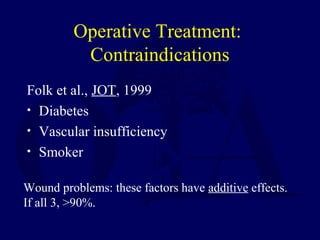
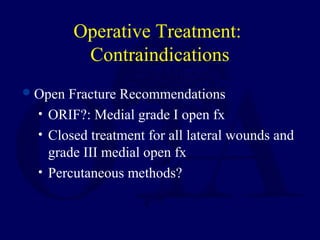
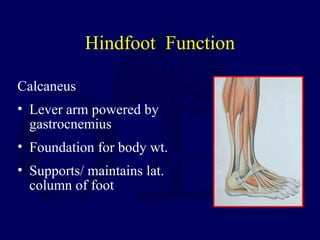
Fractures of the calcaneus can cause long-term disability if not treated properly. While the best treatment method is controversial, operative treatment via open reduction internal fixation may provide better outcomes than non-operative treatment by restoring anatomy and preventing malunion. However, operative treatment also carries risks of wound complications. Treatment must be individualized based on the injury pattern, patient characteristics, and surgeon experience to weigh the risks and benefits of operative versus non-operative management.







![Non-op Treatment: Natural History
Nade and Monahan, Injury, 1973
• 57% long term symptoms (pain, swelling,
stiffness)
• 95% symptoms on uneven ground
• 76% broad heel
As a standard treatment …..”[results] are not
good enough and deserve further studies”](https://image.slidesharecdn.com/l15-calcaneus-161225233549/85/L15-calcaneus-37-320.jpg)