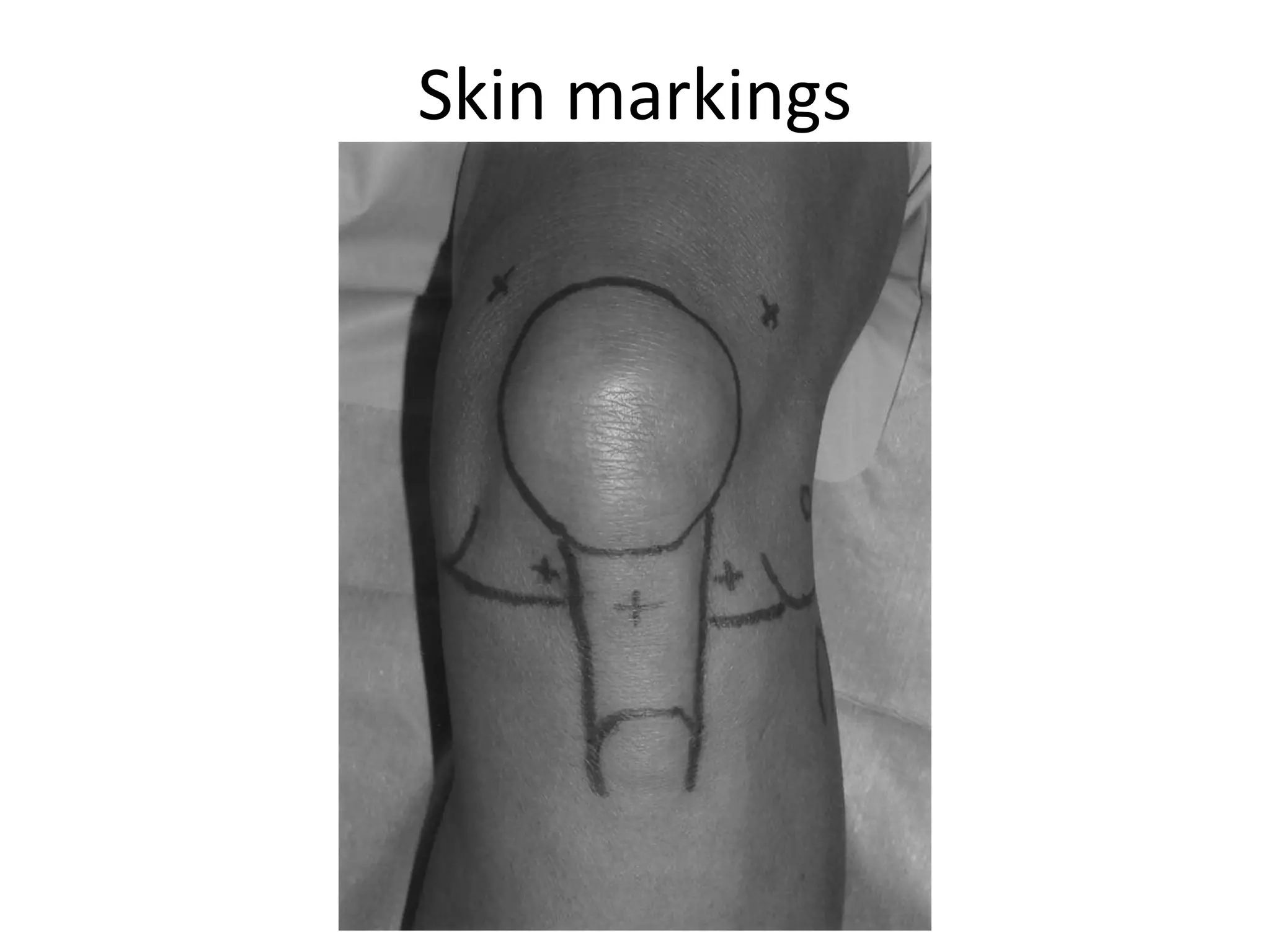
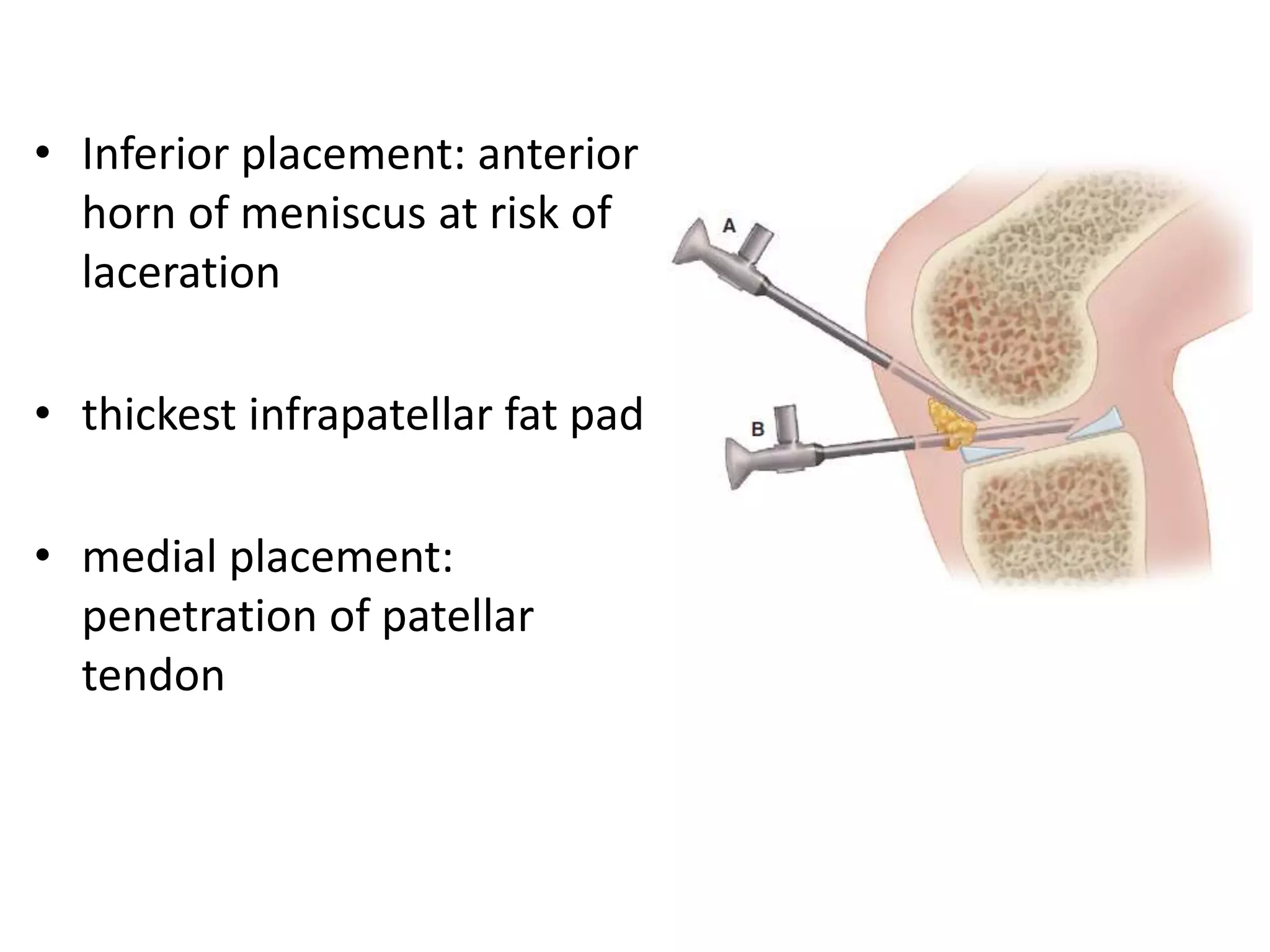
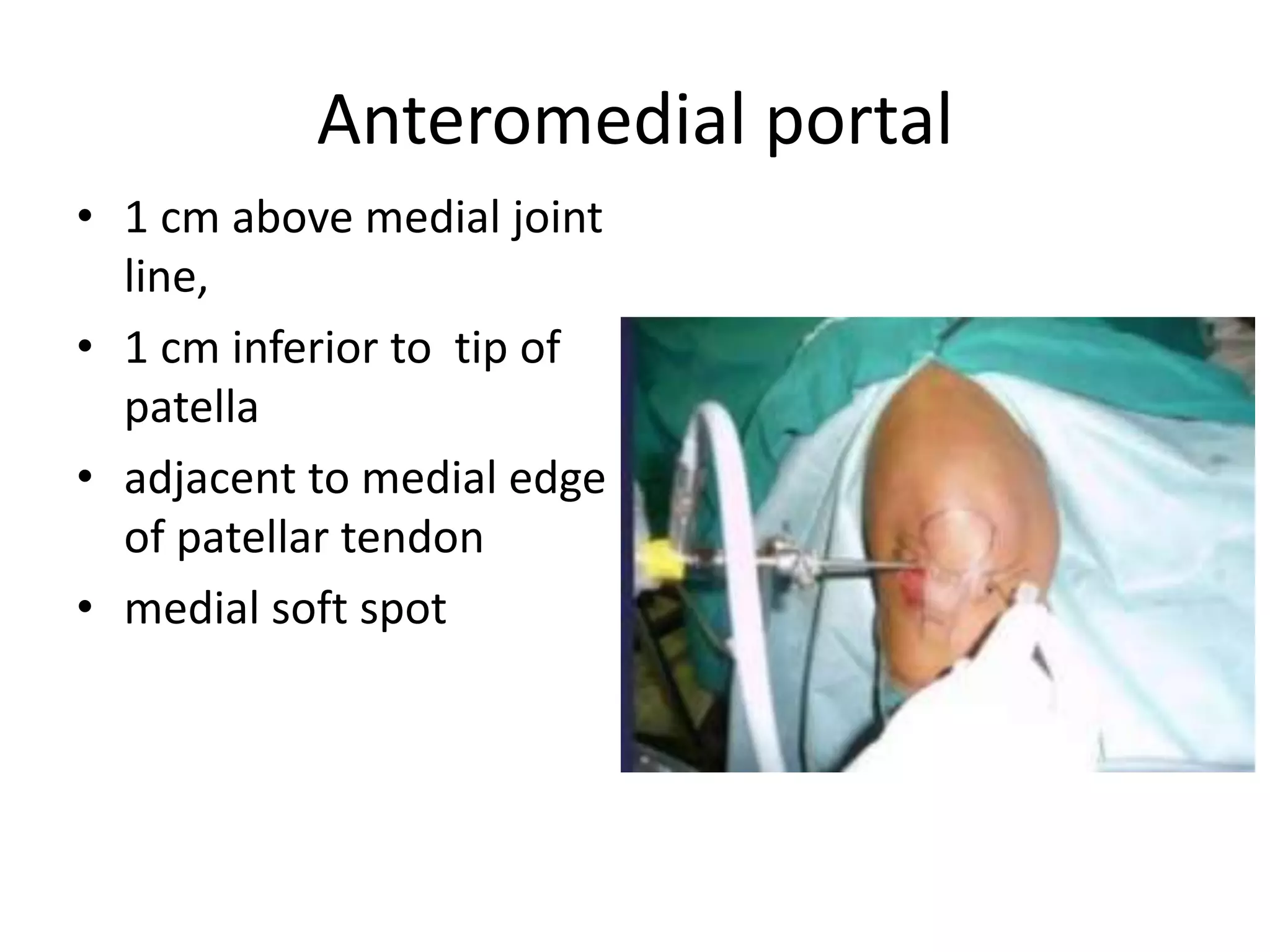
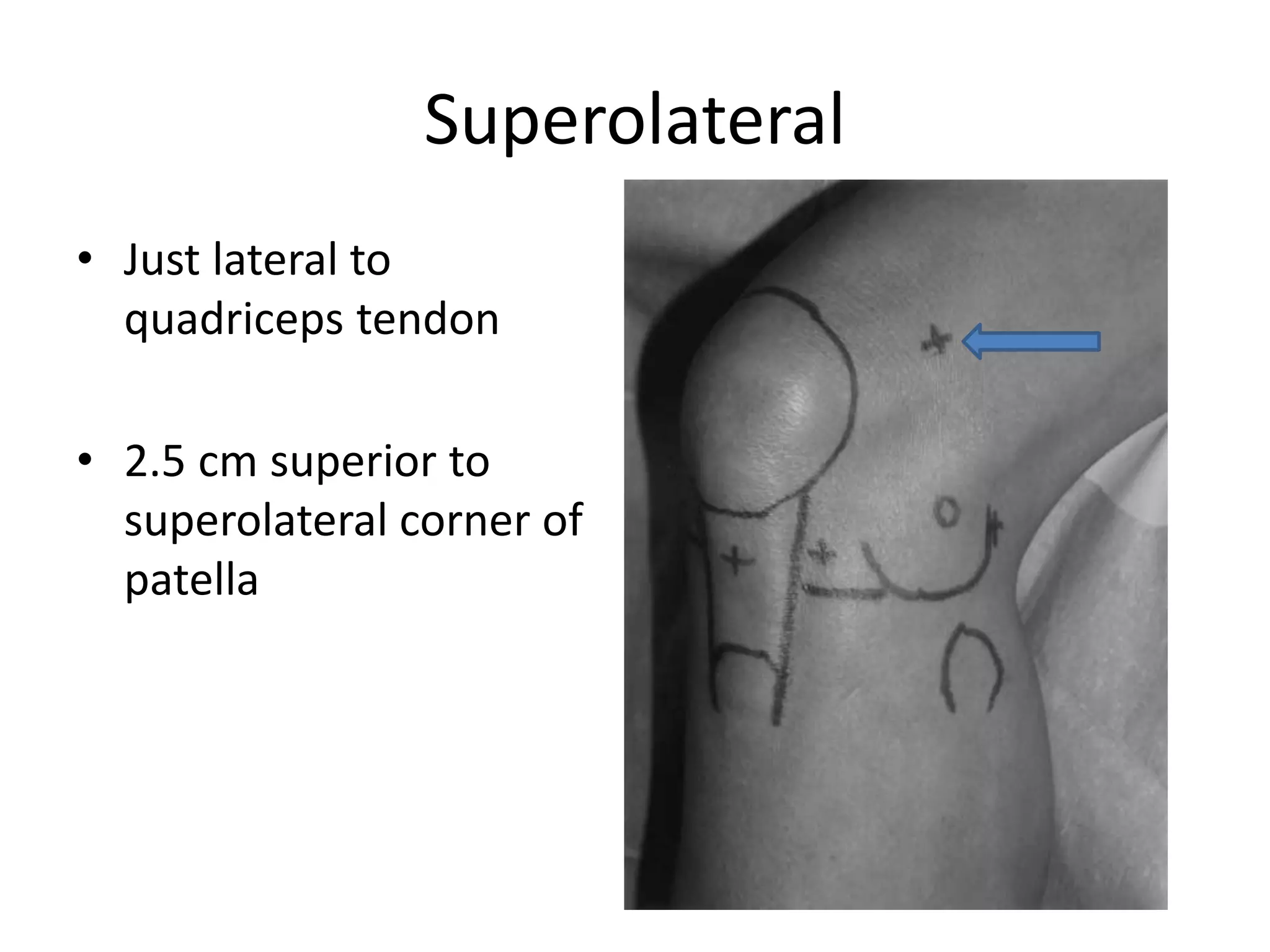
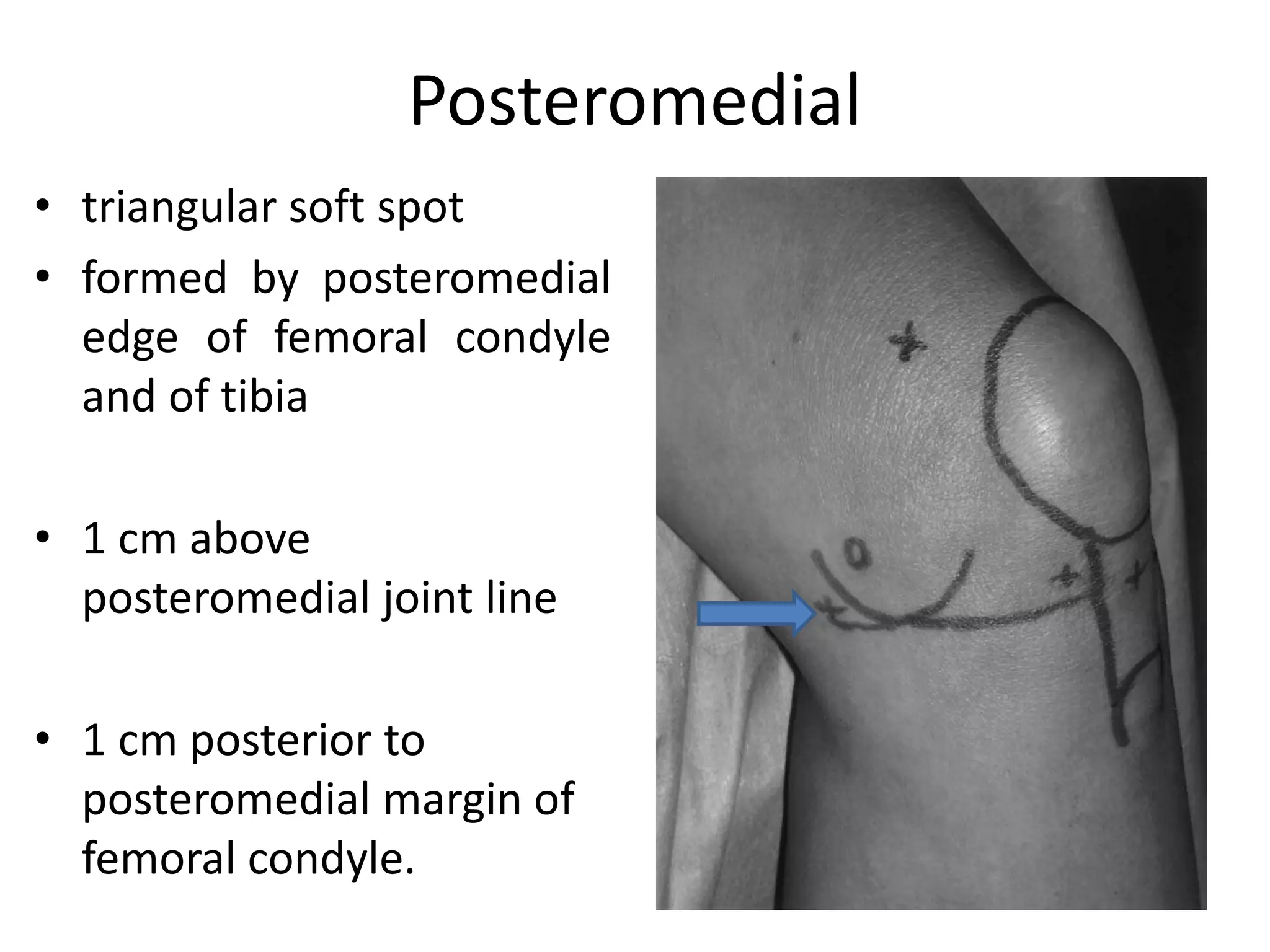
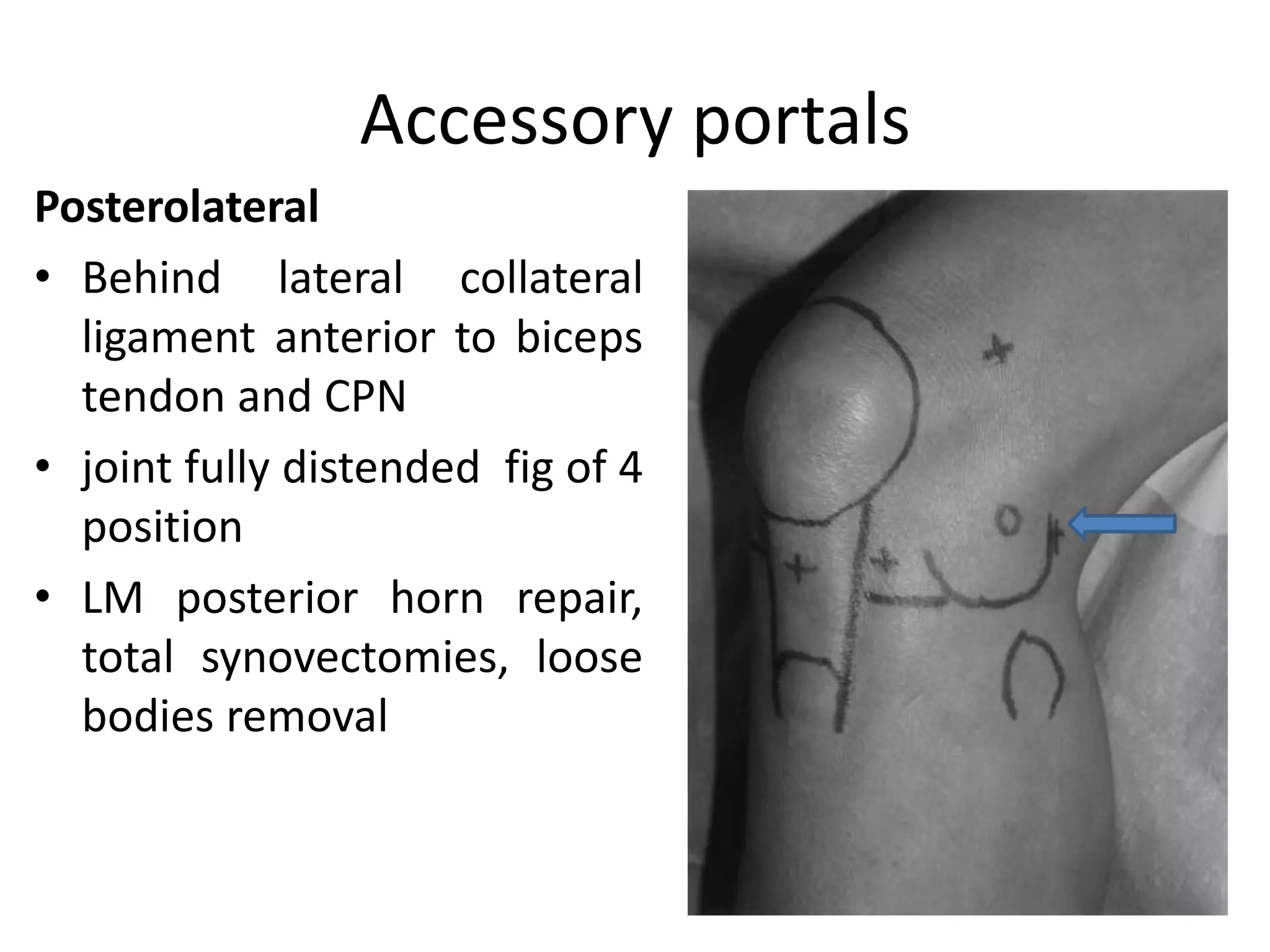
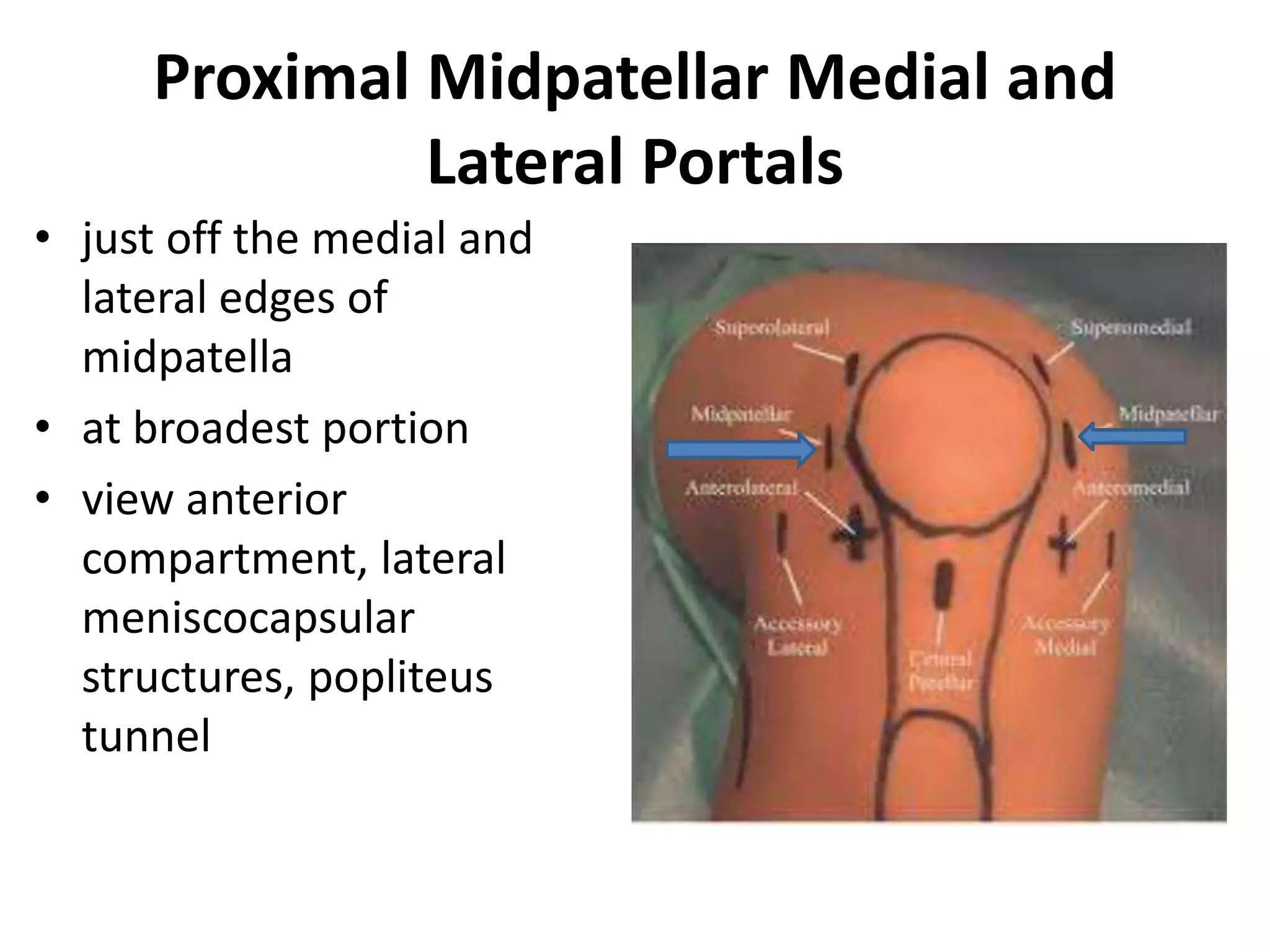
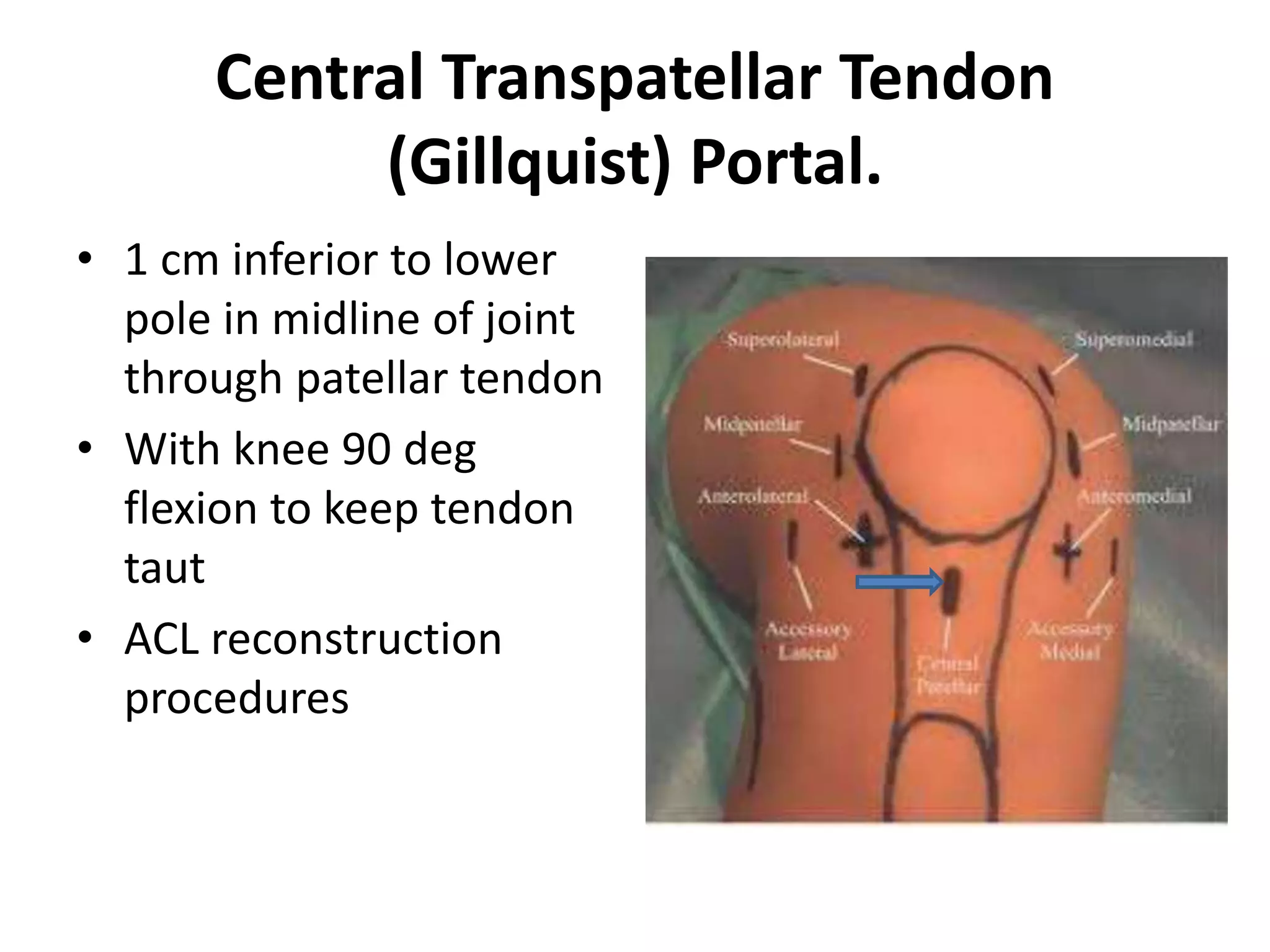
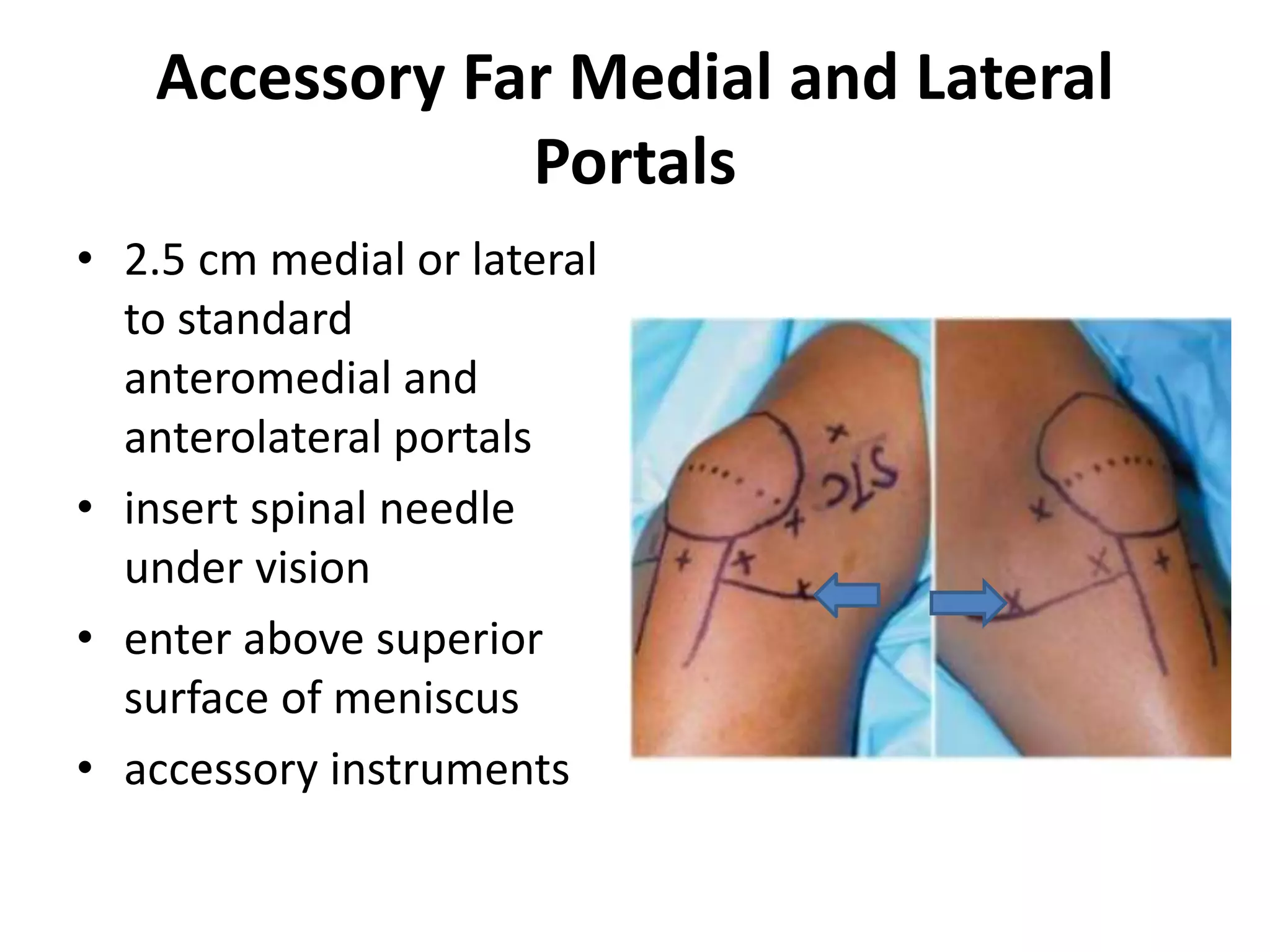
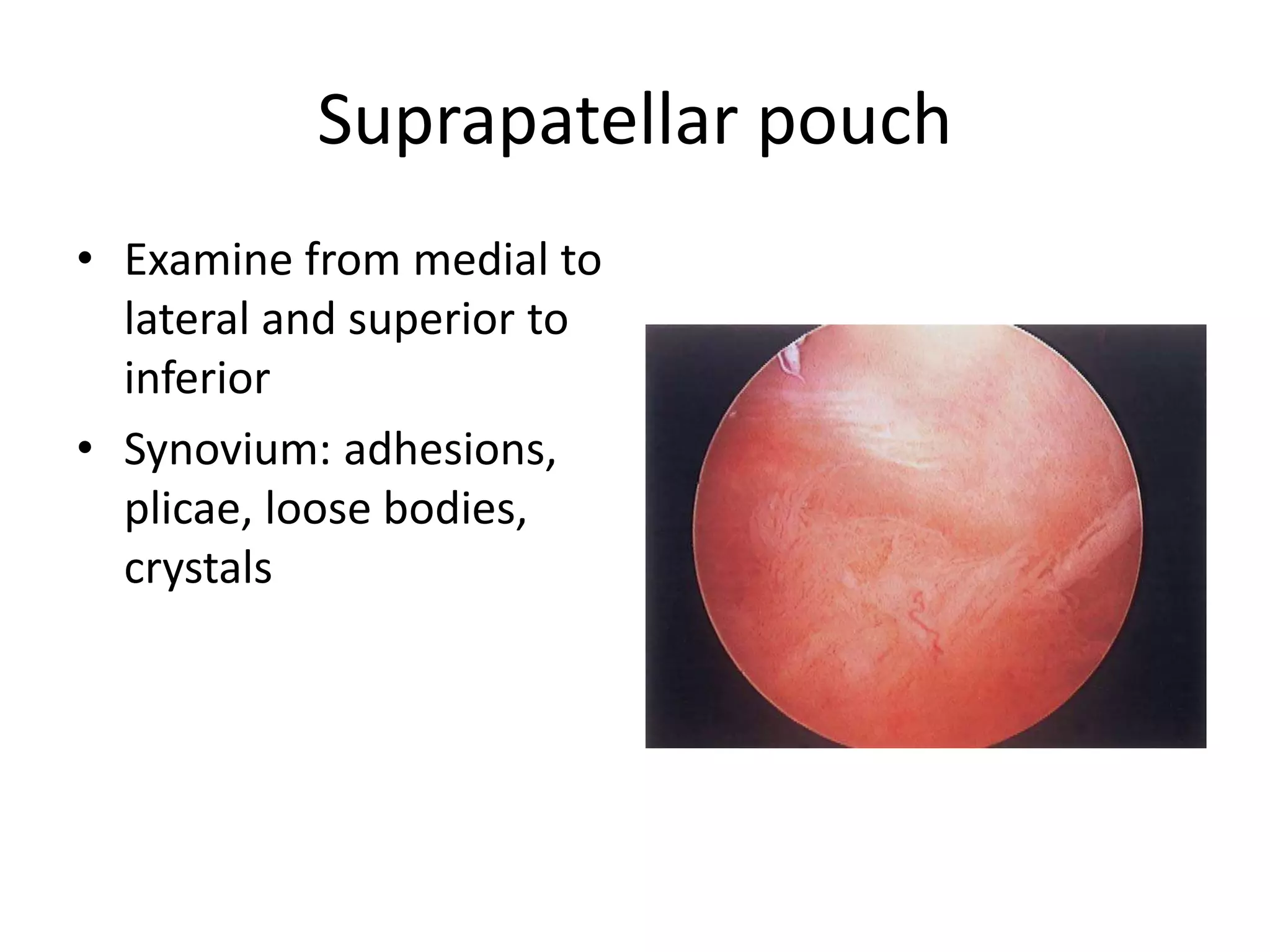
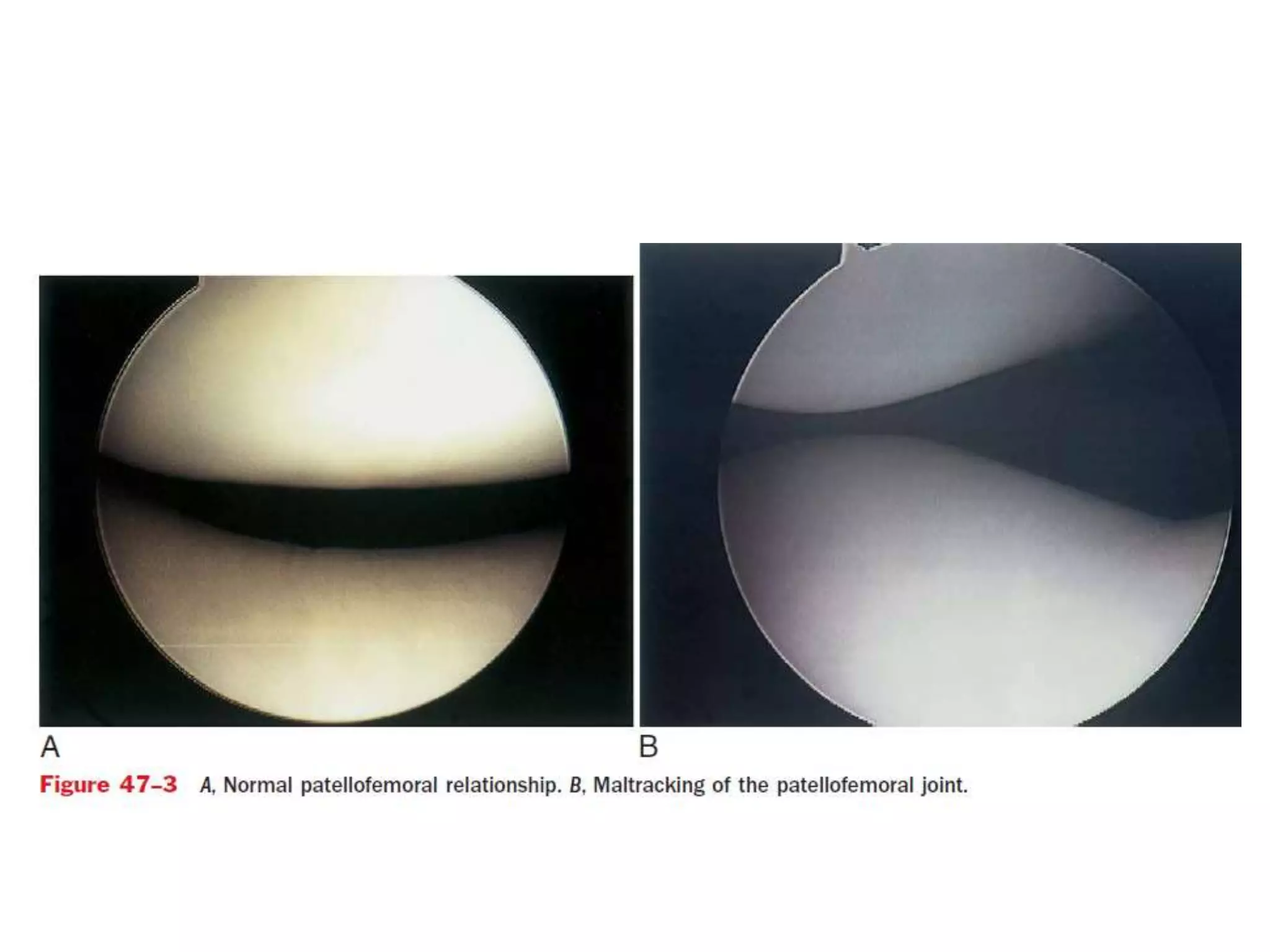
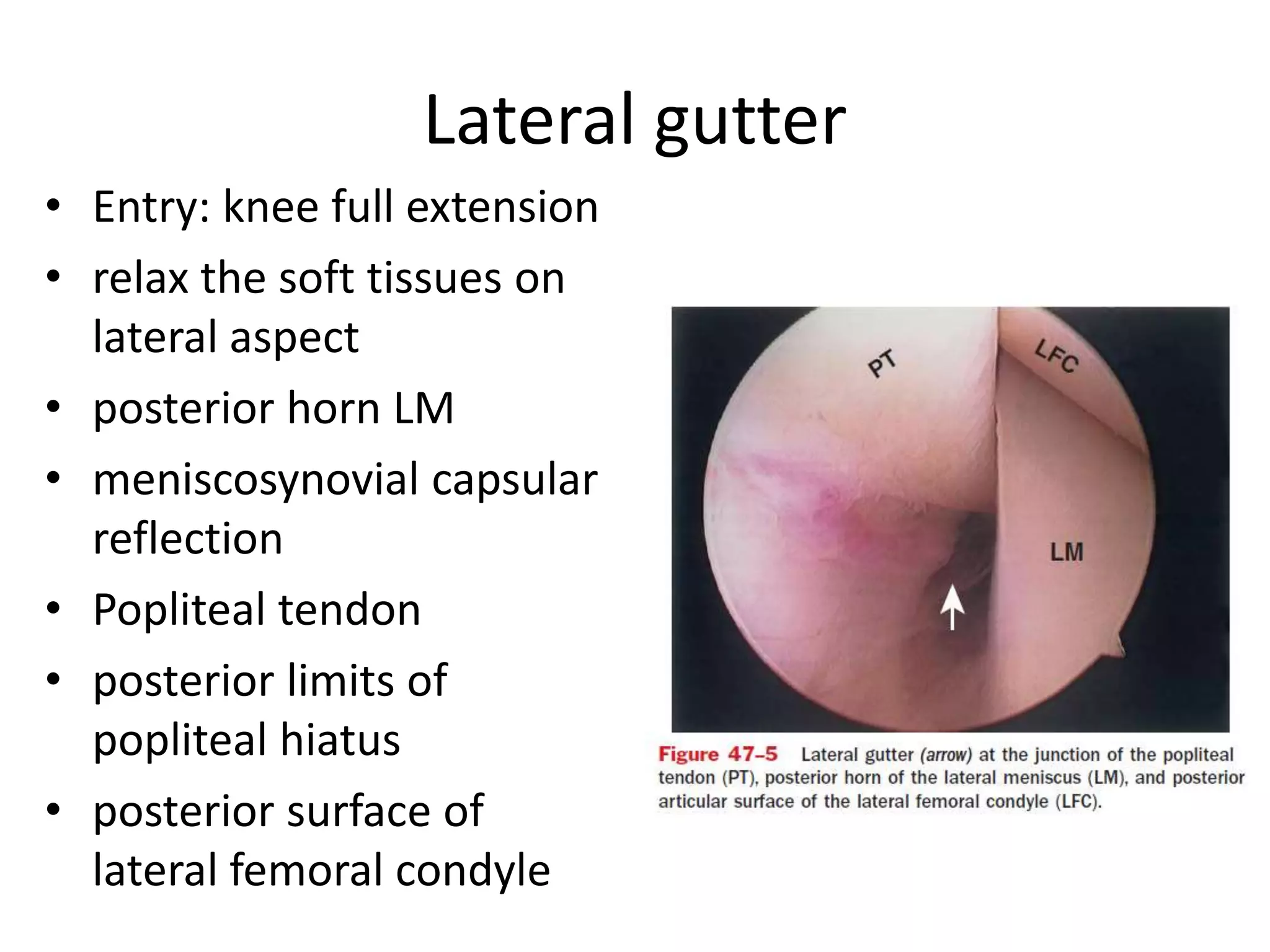
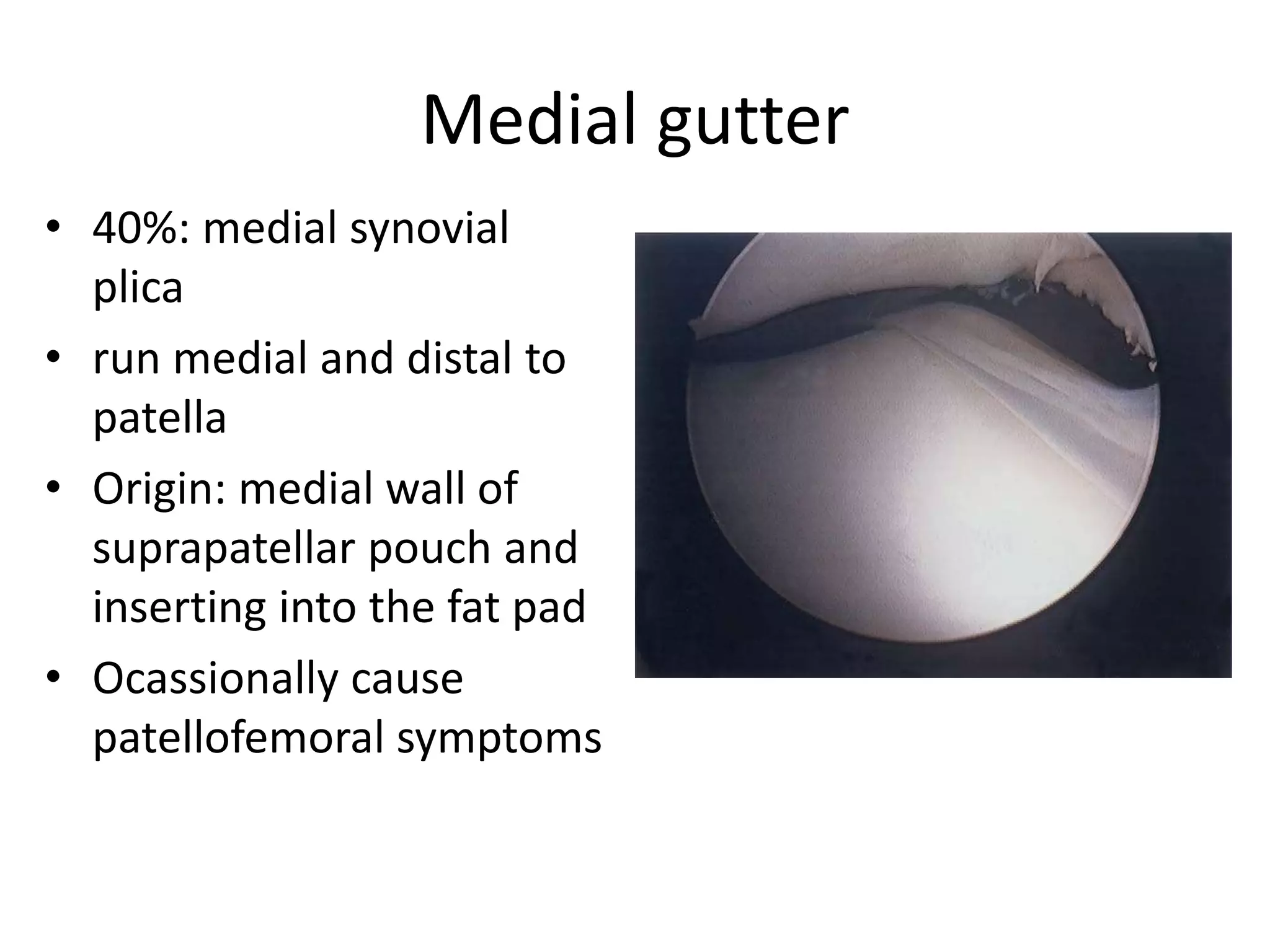
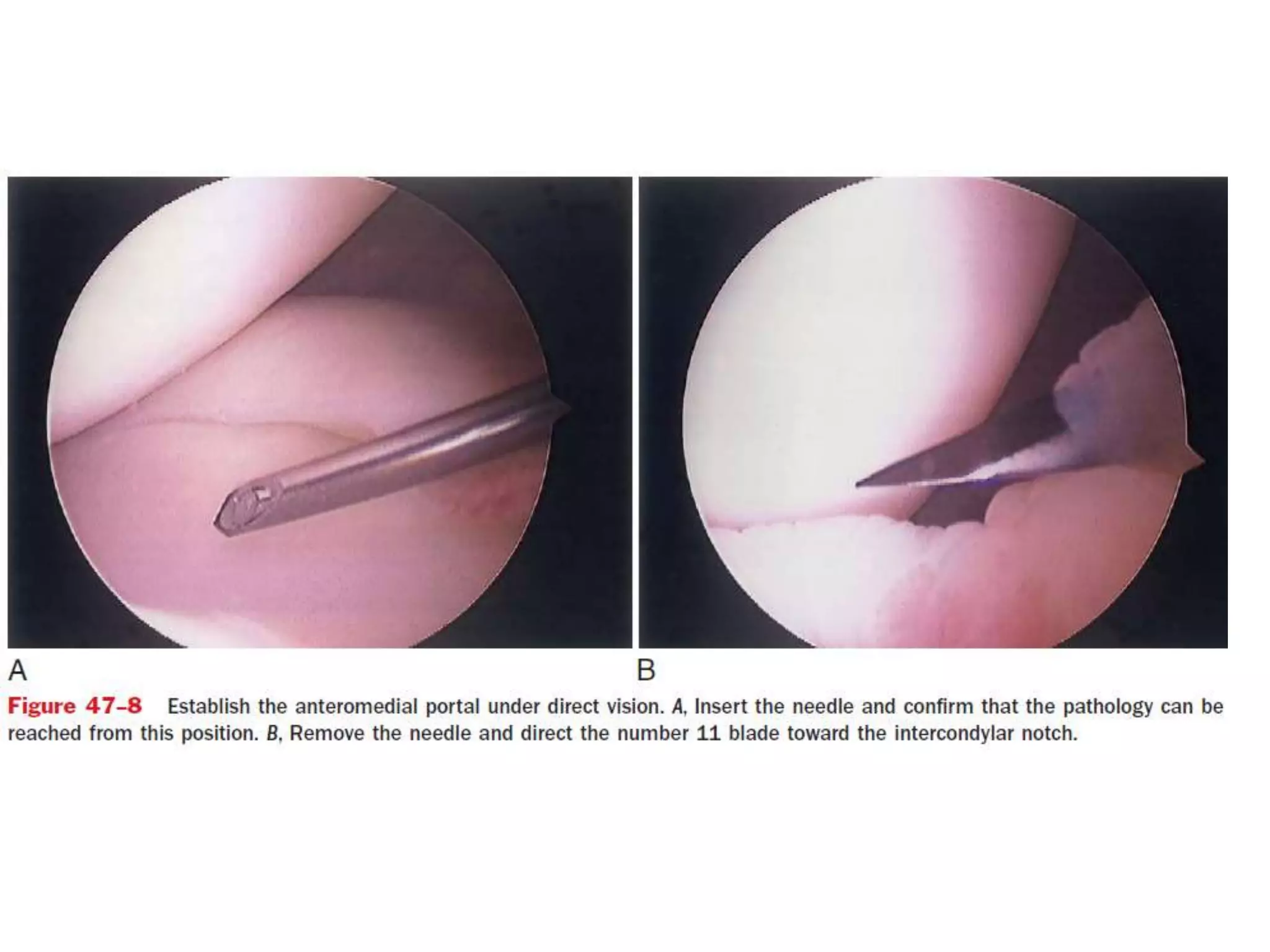
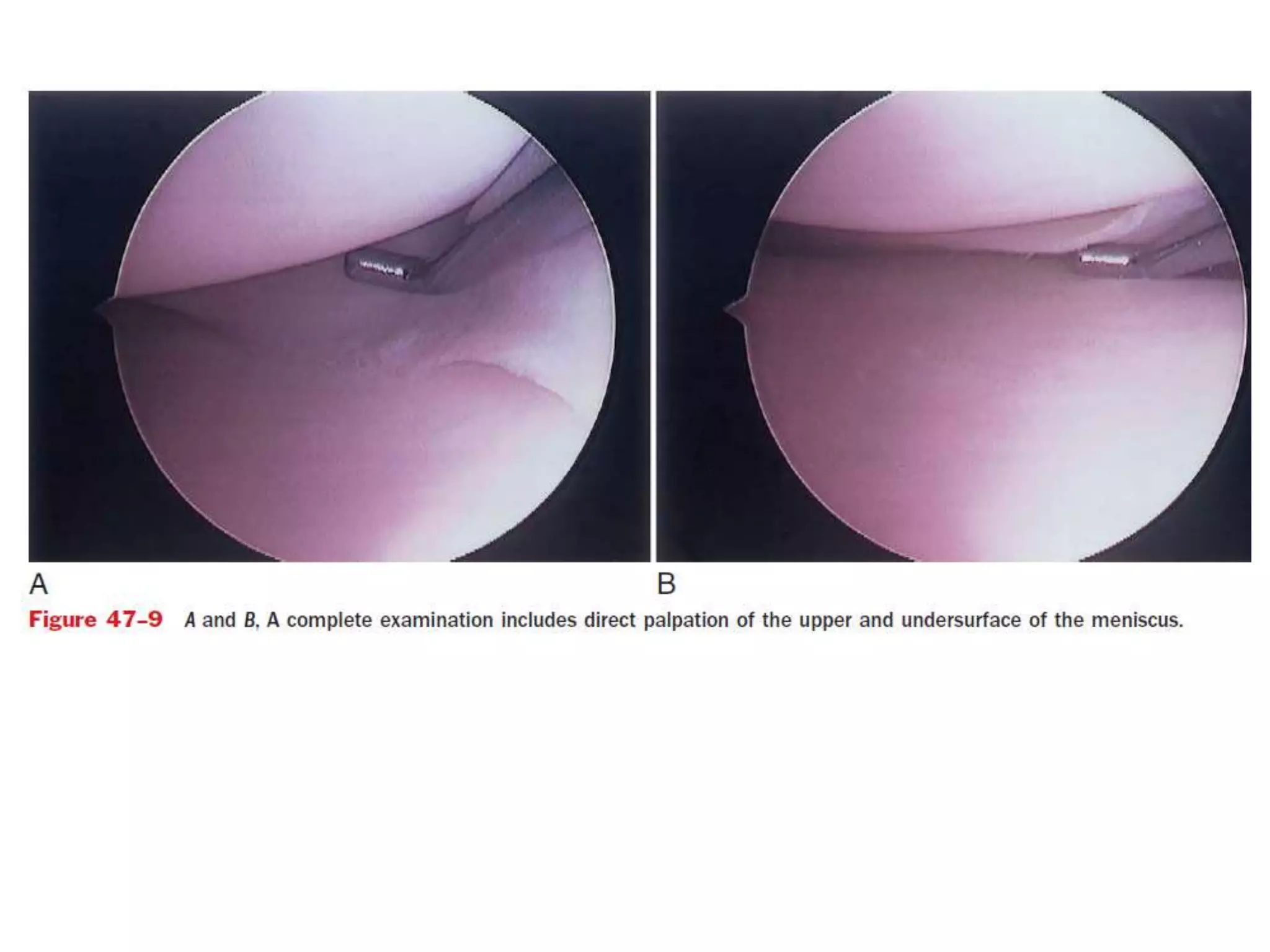
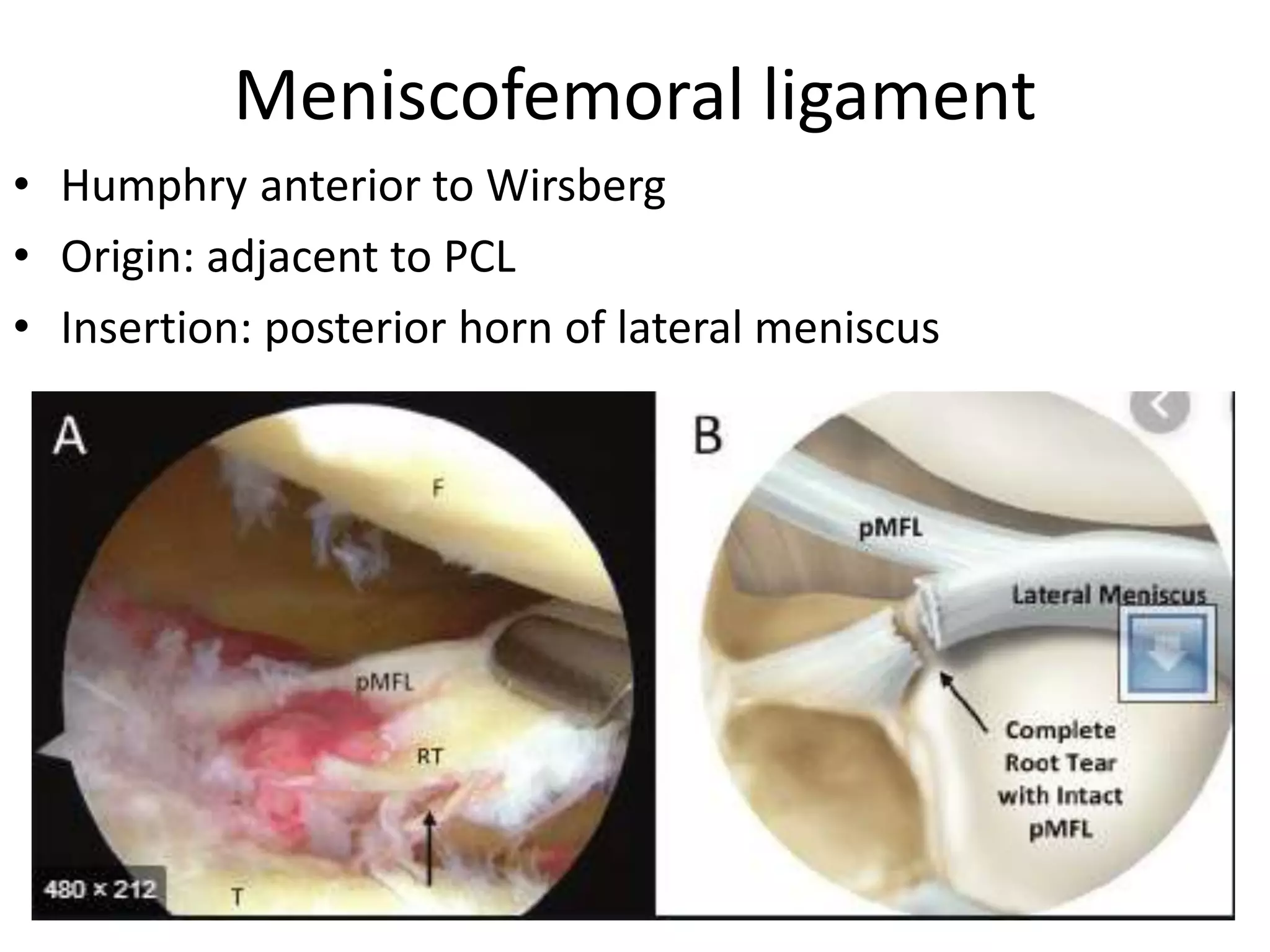
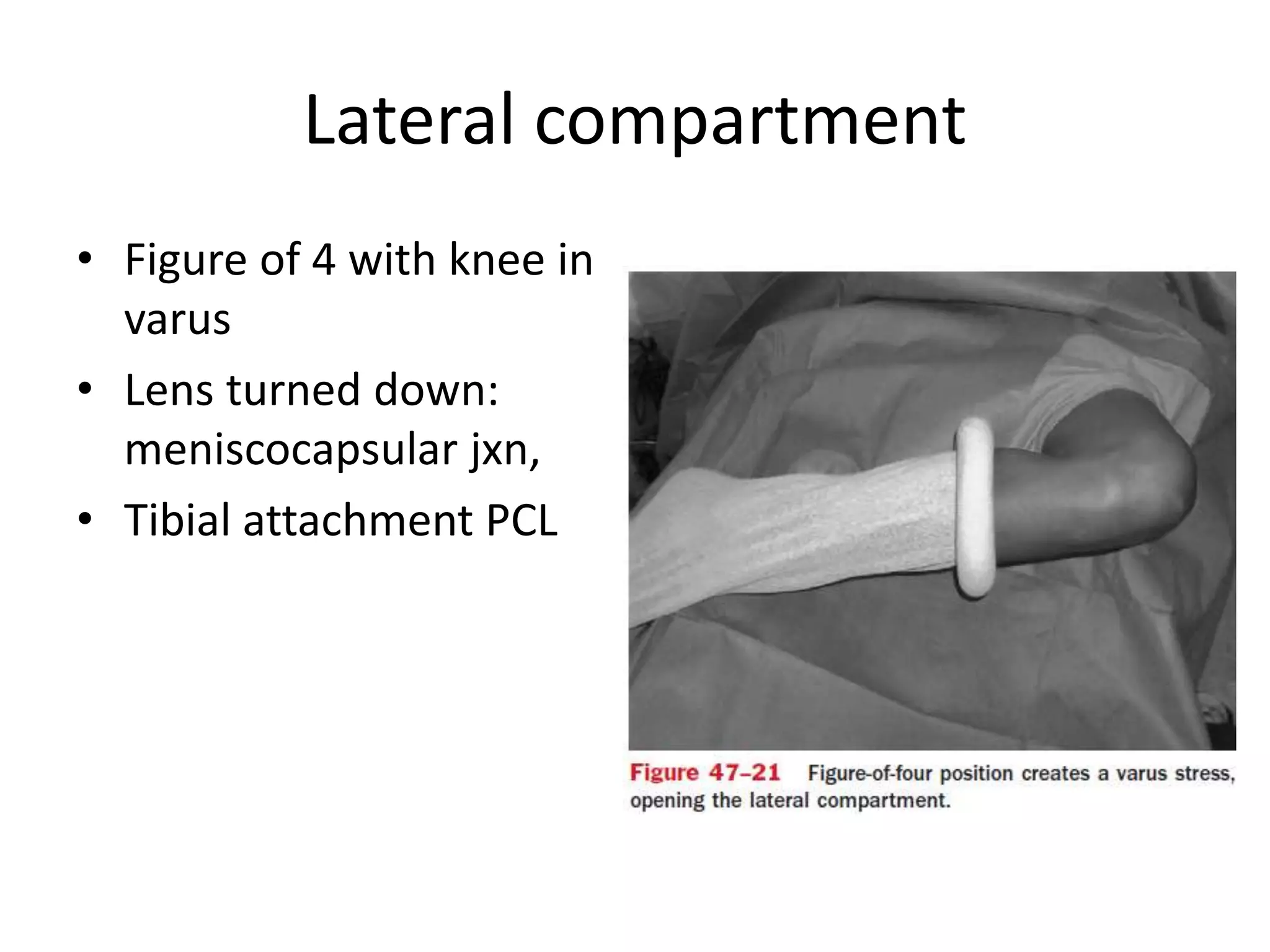
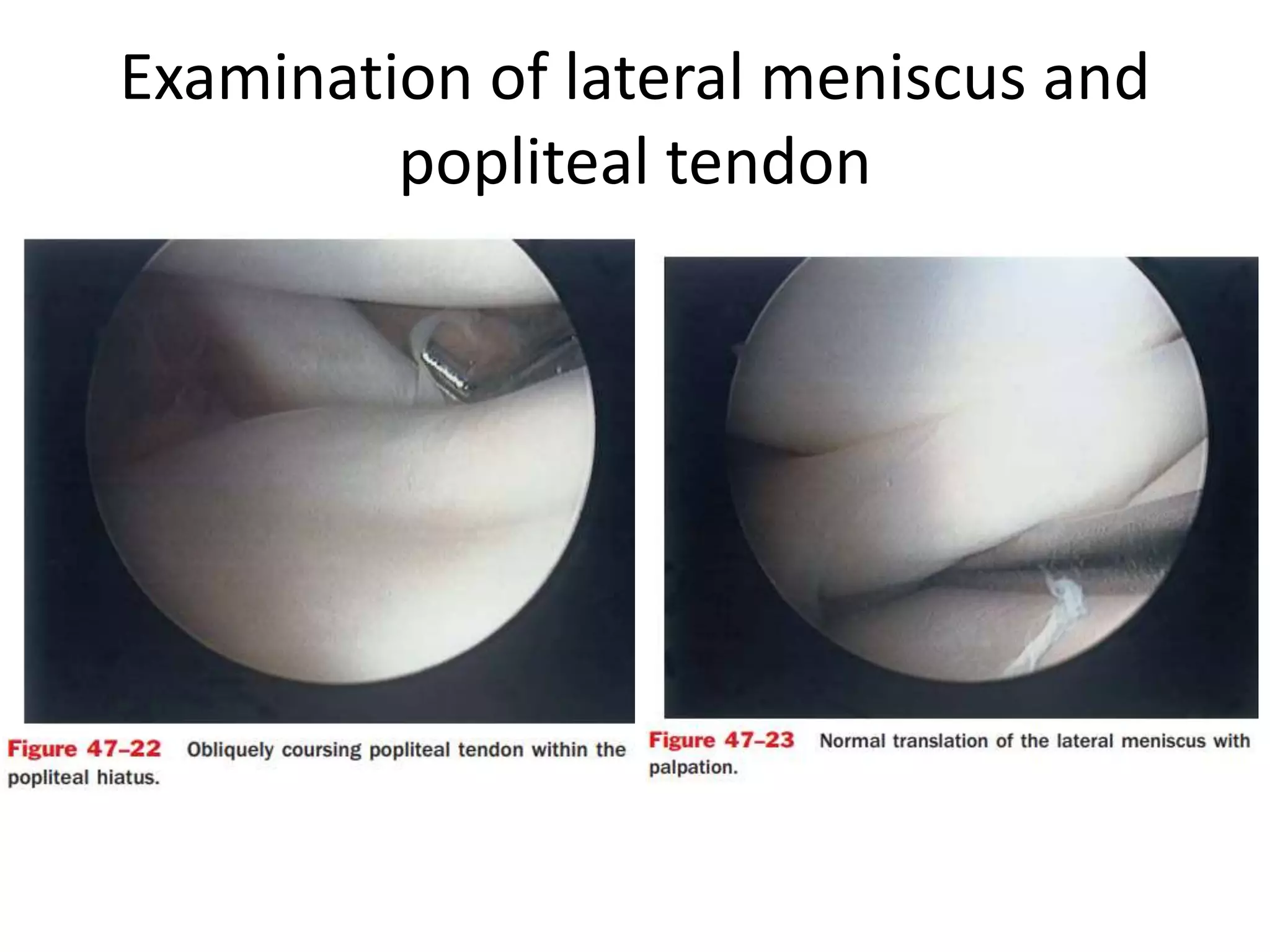
This document discusses knee arthroscopy portals and procedures. It outlines standard and accessory portals for the knee including anterolateral, anteromedial, posteromedial, and superolateral portals. It details patient positioning and skin markings. The document describes examining each compartment of the knee through the portals including the suprapatellar pouch, patellofemoral joint, medial and lateral gutters, medial and lateral menisci, intercondylar notch, ACL, PCL, and meniscofemoral ligaments. Procedures like diagnostic arthroscopy, creating portals, and visualizing structures are outlined.